Podcast
Questions and Answers
What is the optimal blood pressure range considered to be?
What is the optimal blood pressure range considered to be?
90/60mmHg - 120/80mmHg
What blood pressure is considered to be hypertension?
What blood pressure is considered to be hypertension?
140/90mmHg or higher
What blood pressure is considered to be isolated systolic hypertension in a 31-year-old?
What blood pressure is considered to be isolated systolic hypertension in a 31-year-old?
Greater than 130/65mmHg
What percentage of systemic hypertension cases are primary?
What percentage of systemic hypertension cases are primary?
What are the two main categories of secondary hypertension?
What are the two main categories of secondary hypertension?
What is the most common cause of secondary hypertension due to renal disease?
What is the most common cause of secondary hypertension due to renal disease?
Name one endocrine disease that can cause secondary hypertension.
Name one endocrine disease that can cause secondary hypertension.
Name one other cause of secondary hypertension.
Name one other cause of secondary hypertension.
What are the end organs affected by systemic hypertension?
What are the end organs affected by systemic hypertension?
What are the end organ effects of systemic hypertension?
What are the end organ effects of systemic hypertension?
What are some signs of poor weight gain or faltering growth in infants with significant cardiac disease?
What are some signs of poor weight gain or faltering growth in infants with significant cardiac disease?
What percentage of infants with significant cardiac disease have extracardiac anomalies (ECA)?
What percentage of infants with significant cardiac disease have extracardiac anomalies (ECA)?
What is the most common system affected by extracardiac anomalies in infants with significant cardiac disease?
What is the most common system affected by extracardiac anomalies in infants with significant cardiac disease?
How does the presence of an extracardiac anomaly (ECA) affect the mortality rate in infants with congenital heart disease (CHD)?
How does the presence of an extracardiac anomaly (ECA) affect the mortality rate in infants with congenital heart disease (CHD)?
What is the difference between fetal circulation and adult circulation?
What is the difference between fetal circulation and adult circulation?
What are some common congenital cardiovascular abnormalities?
What are some common congenital cardiovascular abnormalities?
How can congenital cardiovascular disease present?
How can congenital cardiovascular disease present?
What is the management approach for congenital cardiovascular disease?
What is the management approach for congenital cardiovascular disease?
What is the source of the information?
What is the source of the information?
How many infants with significant cardiac disease have some established syndrome?
How many infants with significant cardiac disease have some established syndrome?
What are some symptoms of heart failure in infants?
What are some symptoms of heart failure in infants?
What are some signs of heart failure in infants?
What are some signs of heart failure in infants?
What percentage of infants with significant cardiac disease have extracardiac anomalies?
What percentage of infants with significant cardiac disease have extracardiac anomalies?
What is the most common type of extracardiac anomaly in infants with significant cardiac disease?
What is the most common type of extracardiac anomaly in infants with significant cardiac disease?
What is the impact of having an extracardiac anomaly on the mortality rate in infants with congenital heart disease?
What is the impact of having an extracardiac anomaly on the mortality rate in infants with congenital heart disease?
What is the difference between foetal circulation and adult circulation?
What is the difference between foetal circulation and adult circulation?
Describe the common congenital cardiovascular abnormalities.
Describe the common congenital cardiovascular abnormalities.
How can congenital cardiovascular disease present?
How can congenital cardiovascular disease present?
What is the management approach for congenital cardiovascular disease?
What is the management approach for congenital cardiovascular disease?
What is the impact of having an extracardiac anomaly on the mortality rate in infants with congenital heart disease?
What is the impact of having an extracardiac anomaly on the mortality rate in infants with congenital heart disease?
Flashcards are hidden until you start studying
Study Notes
Aortic Valve Stenosis
- Results from minor to severe degrees of aortic valve maldevelopment or thickening
- One of 4 subtypes of left ventricular outlet obstruction (LVOT)
- Presentation depends on the severity of the obstruction
- Most patients are asymptomatic
- Older patients may present with chest pain or syncope
- In the neonatal period, those with critical aortic stenosis and duct-dependent systemic circulation may present with severe heart failure leading to shock
- A subset of patients present with poor left ventricular function, low cardiac output, and signs of shock and congestive heart failure ('critical' aortic stenosis)
- ECG may show evidence of left ventricular hypertrophy
- CXR may reveal a prominent aorta because of post-stenotic dilation
- Echocardiography helps accurately evaluate aortic valve morphology and estimate the pressure gradient across the LVOT
Left Heart Outflow Obstruction
- In the first week of life, heart failure usually results from left heart obstruction
- If the obstructive lesion is very severe, arterial perfusion may be predominantly by right-to-left blood flow via the arterial duct, so-called duct-dependent systemic circulation
- Closure of the duct under these circumstances rapidly leads to severe acidosis
Duct Dependent Coarctation of the Aorta
- Due to arterial duct tissue encircling the aorta at the duct's insertion point
- Commonly associated with a bicuspid aortic valve (in 70% of patients)
- When the duct closes, the aorta also constricts, causing severe obstruction to the left ventricular outflow
- Presentation: acute circulatory collapse at about two days of age when the duct closes
- Examination: absent femoral pulses, severe metabolic acidosis
- Amenable to surgical repair or balloon dilation
Prenatal Diagnosis of Congenital Heart Defects
- In high-income countries, between 18-20 weeks' gestation, 70% of those infants who require surgery in the first six months of life can be diagnosed antenatally
Symptoms of Congenital Heart Disease
- Depend on the condition
- Although congenital heart disease is present at birth, the symptoms may not appear immediately
- Some problems, such as a small VSD, ASD, or PDA, may never cause any problems
- Murmurs are the most common presentation of minor congenital heart disease
- Symptoms of heart failure: breathlessness, sweating, poor feeding, recurrent chest infections
Ventricular Septal Defects (VSDs)
- Medium VSDs are less likely to close on their own and may require treatment
- Large VSDs allow a lot of blood to flow from the left ventricle to the right ventricle
- Extra blood flow increases blood pressure in the right side of the heart and the lungs
- Symptoms: tachypnoea, tachycardia, pallor, poor feeding, and poor weight gain
- Treatment: closure of the defect (either surgical closure or transcatheter device closure)
Patent Ductus Arteriosus (PDA)
- Persistent patency occurs in 1 in 5000 live births in full-term infants
- Much more common in preterm neonates
- There is a 30-fold higher incidence in patients born at higher altitudes
- PDA is a persistent communication between the descending thoracic aorta and the pulmonary artery
- Murmur: continuous murmur as the pressure in the pulmonary artery is lower than in the aorta throughout the cardiac cycle
- ECG and CXR often are normal
- Echocardiography allows the delineation of the PDA anatomy and the direction and volume of the shunt
- Treatment: intravenous indomethacin or ibuprofen in newborns, closure is recommended to avoid the risk of infective endocarditis in older children
Atrial Septal Defects (ASDs)
- 6-10% of all CHD
- Small ASDs allow only a little blood to leak from one atrium to the other
- Medium and large ASDs allow more blood to leak from one atrium to the other
- Children with isolated ASDs are frequently asymptomatic
- Untreated defect leads to exercise intolerance and atrial arrhythmias in the third or fourth decade of life
- Signs: ejection systolic murmur, pulmonary area
- CXR usually normal in a small ASD
- ECG may be normal in a small lesion but in a larger lesion, there may be right atrial enlargement, right ventricular enlargement, or right axis deviation
- Treatment: either an operation or percutaneous device closure
Tetralogy of Fallot (TOF)
- A combination of four defects
- Most patients with TOF have progressive cyanosis after birth followed by dyspnoea on exertion as a young child
- Faltering growth may be present
- Hypoxic episodes or 'tet spells’ consist of an abrupt onset of rapid shallow breathing, increased agitation, cyanosis, and a decrease in murmur intensity due to reduced blood flow through the RVOT
- Older children with hypoxic spells will squat to increase systemic vascular resistance and thereby reduce hypoxaemia
- Most are diagnosed: antenatally or following the identification of a murmur in the first two months of life
- Cyanosis at this stage may not be apparent, although a few present with severe cyanosis in the first few days of life
- A loud ejection systolic murmur is heard at the left upper sternal border with radiation to both axillae due to the RVOT obstruction
- Treatment: palliative surgery or complete repair
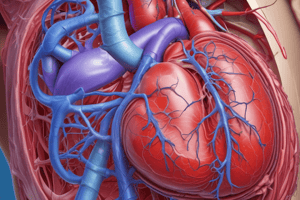
Cardiac Failure
- Failure of the heart to pump sufficient blood, and deliver sufficient oxygen, to satisfy metabolic demands
- Results in under-perfusion which may cause fluid retention and increased blood volume
- Acute and chronic cardiac failure
- Systolic and diastolic cardiac failure
- Right and left ventricular failure
- Causes of left and right ventricular failure
- Coronary heart disease
- Hypertension
- Cardiomyopathies
- Toxins
- Endocrine disorders
- Nutritional deficiencies
- Infiltrative diseases
- Others
Systemic and Pulmonary Hypertension
- Distinguish between pulmonary and systemic hypertension
- B-natriuretic peptide (BNP)
- Causes of systemic hypertension
- End-organ effects of systemic hypertension
- Causes of pulmonary hypertension
- End-organ effects of pulmonary hypertension
Aneurysms and Neoplasms
- Define an aneurysm
- Describe the causes of aneurysms
- Describe the effects of aneurysms
- Define neoplasms
- Describe the causes of neoplasms
- Describe the effects of neoplasms### Causes of Left and Right Ventricular Failure
- Coronary heart disease
- Hypertension
- Cardiomyopathies:
- Familial/genetic
- Non-familial/non-genetic (including acquired, e.g. myocarditis)
- Hypertrophic (HCM)
- Dilated (DCM)
- Restrictive (RCM)
- Arrhythmogenic right ventricular (ARVC)
- Unclassified
- Drugs:
- Beta-blockers
- Calcium antagonists
- Antiarrhythmics
- Cytotoxic agents
- Toxins:
- Alcohol
- Medication
- Cocaine
- Trace elements (mercury, cobalt, arsenic)
- Endocrine:
- Diabetes mellitus
- Hypo/hyperthyroidism
- Cushing syndrome
- Adrenal insufficiency
- Excessive growth hormone
- Phaeochromocytoma
- Nutritional deficiencies:
- Thiamine
- Selenium
- Carnitine
- Obesity and cachexia
- Infiltrative:
- Sarcoidosis
- Amyloidosis
- Haemochromatosis
- Connective tissue disease
- Others:
- Chagas' disease
- HIV infection
- Peripartum cardiomyopathy
- End-stage renal failure
Clinical Effects of Left and Right Ventricular Failure
- "Forward" failure:
- Reduced perfusion of tissues
- Tends to be more associated with advanced failure
- "Backward" failure:
- Due to increased venous pressures
- Dominated by fluid retention and tissue congestion
B-Natriuretic Peptide (BNP)
- Produced by ventricular muscle in response to stress
- Acts on the ANP receptor but with relatively lower affinity and longer half-life than other natriuretic proteins
- Part of a family: ANP (produced in atrial muscle), CNP (from large blood vessels), DNP (present in blood, probably originates from heart)
- Effects:
- Vessel dilatation
- Reduced load on heart
- Changes in glomerular filtration
- Inhibits renin secretion
- Decreases aldosterone
- Natriuresis
- Reduction in blood pressure
Hypertension
- Definition: Persistent raised blood pressure above 140/90 mmHg
- Classification:
- Primary vs secondary (based on cause)
- Essential vs accelerated (based on clinical presentation)
- Epidemiology:
- Estimated 1.28 billion adults worldwide have hypertension
- Most (two-thirds) living in low- and middle-income countries
- Impact:
- Major risk factor for cardiovascular disease
- Ischaemic heart disease
- Accelerated atherosclerosis
- Alzheimer-type dementia
- Importance: Preventable cause of premature disease and death in developed and developing countries
Pulmonary Hypertension
- Definition: Elevated pulmonary artery pressure >25 mmHg at rest
- Causes:
- Increased pulmonary vascular resistance
- Diffuse lung disease (e.g. COPD)
- Elevated left atrial pressure (e.g. left ventricular failure, mitral valve stenosis)
- Recurrent pulmonary emboli
- Primary pulmonary hypertension (unknown cause) - genetics
- Left-right shunts (e.g. ASD, VSD)
End-Organ Effects of Systemic Hypertension
- Brain:
- Atherosclerosis
- Ischaemia and TIA
- Infarct
- Haemorrhage
- Eyes:
- Retinal damage
- Blindness
- Kidneys:
- Nephrosclerosis
- Proteinuria
- Haematuria
- Chronic renal failure
- Acceleration of atherosclerosis
- Heart:
- Left ventricular hypertrophy
- Ischaemic heart disease
Aneurysms
- Definition: Bulging or swollen blood vessel
- Causes:
- Atherosclerosis
- Hypertension
- Berry aneurysm (congenital)
- Dissecting aneurysm (e.g. Marfan's syndrome)
- Mycotic aneurysm (infective endocarditis)
- Effects:
- Local and systemic effects
- Screening, prevention, and treatment
Other Topics
- Transposition of the Great Arteries
- Atrioventricular Septal Defect (AVSD)
- Pulmonary Valve Stenosis
- CHD affecting the valves inside the heart (Atresia, Stenosis, Regurgitation)
- Congenital heart defects (CHD)
- Foetal circulation
- Neonatal circulation - the transition### Congenital Heart Disease (CHD)
- CHD is a problem with the heart's structure that is present at birth
- 0.8% of live births have CHD, making it the most common type of congenital disability
Types of CHD
Non-Cyanotic CHD
- Ventricular Septal Defect (VSD)
- Atrial Septal Defect (ASD)
- Pulmonary Stenosis
- Aortic Stenosis
- Coarctation of the Aorta
- Patent Ductus Arteriosus (PDA)
Cyanotic CHD
- Tetralogy of Fallot (TOF)
- Total Anomalous Pulmonary Venous Return
- Transposition of the Great Arteries
- Tricuspid Atresia
- Truncus Arteriosus
- Hypoplastic Left Heart
- Pulmonary Atresia
Ventricular Septal Defect (VSD)
- 20% of CHD cases
- Defect in the wall between the ventricles
- Small VSDs may close on their own, while medium and large VSDs require treatment
- Signs: Tachypnoea, Tachycardia, Poor weight gain, Heart murmur, Gallop rhythm, Enlarged heart, Hepatomegaly, Cool peripheries
Atrial Septal Defect (ASD)
- 6-10% of CHD cases
- Defect in the wall between the atria
- Small ASDs may close on their own, while medium and large ASDs require treatment
- Signs: Recurrent chest infections, No symptoms, Ejection systolic murmur, Pulmonary area
Patent Ductus Arteriosus (PDA)
- 9-12% of CHD cases
- Failure of the ductus arteriosus to close after birth
- Left-to-right shunt, allowing blood to flow from the aorta to the pulmonary artery
- Signs: Continuous murmur, Poor weight gain, Tachypnoea, Tachycardia
Tetralogy of Fallot (TOF)
- Combination of four defects: Pulmonary valve stenosis, Ventricular Septal Defect, Overriding aorta, Right ventricular hypertrophy
- 4-8% of CHD cases
- Signs: Cyanosis, Dyspnoea on exertion, Faltering growth, Hypoxic episodes ('tet spells')
Transposition of the Great Arteries
- Pulmonary arteries supplied by the left ventricle, and the aorta by the right ventricle
- Cyanosis is always present
- Second heart sound is often loud and single
- No murmur
Atrioventricular Septal Defect (AVSD)
- Holes between the chambers of the right and left sides of the heart
- Valves that control blood flow may not be formed correctly
- Common in babies with Down syndrome
- Signs: Cyanosis at birth or heart failure at 2-3 weeks of life, No murmur heard
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.