Podcast
Questions and Answers
What causes muscle shortening according to the sliding filament model?
What causes muscle shortening according to the sliding filament model?
- Movement of actin filaments over myosin filaments (correct)
- Reduction in the distance between Z-lines
- Movement of myosin filaments over actin filaments
- Contraction of sarcomeres
The formation of cross-bridges between actin and myosin filaments is a key step in muscle contraction.
The formation of cross-bridges between actin and myosin filaments is a key step in muscle contraction.
True (A)
What are the four main steps involved in muscle contraction?
What are the four main steps involved in muscle contraction?
Excitation, excitation-contraction coupling, contraction, relaxation
The difference in electrical charge across the plasma membrane of a cell is known as a ______ potential.
The difference in electrical charge across the plasma membrane of a cell is known as a ______ potential.
Which of the following contributes to the polarization of a cell's membrane?
Which of the following contributes to the polarization of a cell's membrane?
Match the following ion channels with their triggering mechanism:
Match the following ion channels with their triggering mechanism:
The Na+/K+ pump contributes to the polarization of the cell membrane by pumping more positive charge out of the cell than in.
The Na+/K+ pump contributes to the polarization of the cell membrane by pumping more positive charge out of the cell than in.
What is the typical range of resting membrane potential (Vm) in inactive muscle cells?
What is the typical range of resting membrane potential (Vm) in inactive muscle cells?
What is the primary function of the longitudinal tubules (sER) in muscle cells?
What is the primary function of the longitudinal tubules (sER) in muscle cells?
Myofibrils are long bundles of protein structures called myofilaments.
Myofibrils are long bundles of protein structures called myofilaments.
What are the three main components of myofilaments?
What are the three main components of myofilaments?
The head of the myosin molecule forms ____ with the thin filaments.
The head of the myosin molecule forms ____ with the thin filaments.
Match the following proteins with their descriptions:
Match the following proteins with their descriptions:
What type of channel is opened by stretch or mechanical pressure?
What type of channel is opened by stretch or mechanical pressure?
Each muscle is served by multiple nerves, each carrying signals from the spinal cord.
Each muscle is served by multiple nerves, each carrying signals from the spinal cord.
What is the name of the bulbous swelling at the end of each telodendrium where a neuron interacts with another cell?
What is the name of the bulbous swelling at the end of each telodendrium where a neuron interacts with another cell?
The synapse between a neuron and a muscle is called the ______.
The synapse between a neuron and a muscle is called the ______.
Which of the following is NOT true about the motor end plate?
Which of the following is NOT true about the motor end plate?
The binding of acetylcholine to its receptors causes the opening of sodium (Na+) channels, leading to depolarization of the muscle cell.
The binding of acetylcholine to its receptors causes the opening of sodium (Na+) channels, leading to depolarization of the muscle cell.
What is the threshold value for depolarization that must be reached for voltage-gated ion channels to open?
What is the threshold value for depolarization that must be reached for voltage-gated ion channels to open?
The neuromuscular junction (NMJ) is characterized by bidirectional transmission of signals.
The neuromuscular junction (NMJ) is characterized by bidirectional transmission of signals.
Which of the following is NOT a characteristic of the neuromuscular junction?
Which of the following is NOT a characteristic of the neuromuscular junction?
The enzyme responsible for the synthesis of acetylcholine is called ______.
The enzyme responsible for the synthesis of acetylcholine is called ______.
What is the role of calcium ions in the release of acetylcholine at the NMJ?
What is the role of calcium ions in the release of acetylcholine at the NMJ?
Match the following drugs with their effects on the neuromuscular junction:
Match the following drugs with their effects on the neuromuscular junction:
Which of the following conditions can affect the neuromuscular junction?
Which of the following conditions can affect the neuromuscular junction?
Describe the role of T-tubules in excitation-contraction coupling.
Describe the role of T-tubules in excitation-contraction coupling.
The end plate potential (EPP) is always excitatory, leading to muscle fiber depolarization and contraction.
The end plate potential (EPP) is always excitatory, leading to muscle fiber depolarization and contraction.
Which band in the sarcomere contains only thin filaments?
Which band in the sarcomere contains only thin filaments?
The sliding filament hypothesis proposes that thick filaments slide over thin filaments during muscle contraction.
The sliding filament hypothesis proposes that thick filaments slide over thin filaments during muscle contraction.
What is the name of the structure that encircles each myofibril at the A-I junction?
What is the name of the structure that encircles each myofibril at the A-I junction?
The ______ is the area of attachment for the actin fibers in a sarcomere.
The ______ is the area of attachment for the actin fibers in a sarcomere.
Match the following structures with their descriptions:
Match the following structures with their descriptions:
Which of the following characteristics are associated with fast fibers?
Which of the following characteristics are associated with fast fibers?
Fast fibers fatigue quickly due to their reliance on aerobic metabolism.
Fast fibers fatigue quickly due to their reliance on aerobic metabolism.
What is the primary role of calmodulin in smooth muscle contraction?
What is the primary role of calmodulin in smooth muscle contraction?
Myasthenia gravis is an autoimmune disease that affects the ______, leading to muscle weakness and fatigability.
Myasthenia gravis is an autoimmune disease that affects the ______, leading to muscle weakness and fatigability.
Match the following terms with their related descriptions:
Match the following terms with their related descriptions:
Which of the following is NOT a characteristic of smooth muscle?
Which of the following is NOT a characteristic of smooth muscle?
Neostigmine is a type of drug used to treat Myasthenia gravis by inhibiting acetylcholinesterase activity.
Neostigmine is a type of drug used to treat Myasthenia gravis by inhibiting acetylcholinesterase activity.
What is the primary difference between the mechanism of calcium release in skeletal and cardiac muscle?
What is the primary difference between the mechanism of calcium release in skeletal and cardiac muscle?
Flashcards
Longitudinal tubules (sER)
Longitudinal tubules (sER)
Specialized structures in muscle cells responsible for storing calcium ions (Ca2+).
Myofibrils
Myofibrils
Rod-like structures in muscle fibers that enable muscle contraction through bundles of myofilaments.
Myofilaments
Myofilaments
Protein structures in myofibrils classified as thick (myosin) and thin (actin) filaments with regulatory proteins.
Myosin structure
Myosin structure
Signup and view all the flashcards
Actin structure
Actin structure
Signup and view all the flashcards
Sarcomere
Sarcomere
Signup and view all the flashcards
A band
A band
Signup and view all the flashcards
I band
I band
Signup and view all the flashcards
T-Tubules
T-Tubules
Signup and view all the flashcards
Sliding Filament Hypothesis
Sliding Filament Hypothesis
Signup and view all the flashcards
Cross-bridges
Cross-bridges
Signup and view all the flashcards
Z-lines
Z-lines
Signup and view all the flashcards
Excitation (muscle)
Excitation (muscle)
Signup and view all the flashcards
Membrane potential (Vm)
Membrane potential (Vm)
Signup and view all the flashcards
Polarized cells
Polarized cells
Signup and view all the flashcards
Gated ion channels
Gated ion channels
Signup and view all the flashcards
Ligand-gated channels
Ligand-gated channels
Signup and view all the flashcards
Mechanically-gated channels
Mechanically-gated channels
Signup and view all the flashcards
Neuromuscular junction (NMJ)
Neuromuscular junction (NMJ)
Signup and view all the flashcards
Motor end plate
Motor end plate
Signup and view all the flashcards
Acetylcholine (ACh)
Acetylcholine (ACh)
Signup and view all the flashcards
Synaptic cleft
Synaptic cleft
Signup and view all the flashcards
Depolarization
Depolarization
Signup and view all the flashcards
Threshold
Threshold
Signup and view all the flashcards
Motor unit
Motor unit
Signup and view all the flashcards
Fast Fibers
Fast Fibers
Signup and view all the flashcards
Myasthenia Gravis
Myasthenia Gravis
Signup and view all the flashcards
Anticholinesterase Treatment
Anticholinesterase Treatment
Signup and view all the flashcards
Smooth Muscle Tone
Smooth Muscle Tone
Signup and view all the flashcards
Calmodulin in Smooth Muscle
Calmodulin in Smooth Muscle
Signup and view all the flashcards
Cardiac Muscle Contraction
Cardiac Muscle Contraction
Signup and view all the flashcards
Phosphorylation in Muscle Contraction
Phosphorylation in Muscle Contraction
Signup and view all the flashcards
Role of Acetylcholine (ACh)
Role of Acetylcholine (ACh)
Signup and view all the flashcards
Synthesis of ACh
Synthesis of ACh
Signup and view all the flashcards
Release mechanism of ACh
Release mechanism of ACh
Signup and view all the flashcards
Excitatory postsynaptic potential (EPP)
Excitatory postsynaptic potential (EPP)
Signup and view all the flashcards
Synaptic delay
Synaptic delay
Signup and view all the flashcards
Factors affecting NMJ
Factors affecting NMJ
Signup and view all the flashcards
Excitation-contraction coupling
Excitation-contraction coupling
Signup and view all the flashcards
Study Notes
Chapter IV: Physiology of Muscle
- This chapter covers the physiology of muscle tissue, including different types, fine structure, mechanisms of contraction, and the neuromuscular junction.
Learning Objectives
- Students should be able to describe the different types of muscle tissue.
- Students will be able to explain the fine structure of skeletal muscle.
- Students will be able to outline the mechanism of muscle contraction.
- Students will be able to describe the neuromuscular junction.
Introduction
- Muscle is the fleshy organ in the body that converts potential energy from food into mechanical energy.
- The human body is comprised of over 400 skeletal muscles.
- Skeletal muscles account for 40% of total body weight (BW).
- Muscle tissue, combined with nerves, blood vessels, and connective tissues, forms the muscle organs we are familiar with.
- Muscles are complex structures, demonstrating principles of biology and physics.
- Muscle functions include:
- Movement
- Maintaining posture
- Generating heat
- Stabilizing joints
Types of Muscles (part 1)
- Skeletal Muscle:
- Located attached to bones, and responsible for moving the skeleton.
- Elongated, cylindrical, and multi-nucleated cells.
- Striated muscle.
- Voluntary muscle, controlled by the somatic nervous system (SNS).
- Cardiac Muscle:
- Muscle of the heart, uni or bi- nucleated.
- Striated, branched cells.
- Cells are connected by intercalated discs, which are composed of desmosomes and gap junctions.
- Involuntary muscle, controlled by the autonomic nervous system (ANS), and hormones.
- Has properties of autorhythmicity and syncytium.
Types of Muscles (part 2)
- Smooth Muscle:
- Located in walls of hollow organs (digestive tract, blood vessels, urinary bladder, Iris)
- Mononucleated, non-striated cells.
- Involuntary muscle, controlled by the autonomic nervous system (ANS) and hormones.
- Has properties of autorhythmicity and syncytium.
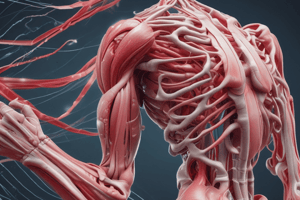
Skeletal Muscle (part 1)
- Skeletal muscles are predominately composed of muscle tissue, and also contain nervous, vascular, and connective tissues.
- The epimysium is a dense, irregular connective tissue that surrounds the skeletal muscle.
Skeletal Muscle (part 2)
- The epimysium surrounds bundles known as fascicles.
- A fascicle is a bundle of super-long skeletal muscle cells (muscle fibers) surrounded by the perimysium.
- Each muscle cell extends the length of the entire muscle organ and is surrounded by the endomysium.
Skeletal Muscle (part 3)
- Each skeletal muscle is supplied by one nerve, one artery, and one or more veins.
- These vascular and neural components enter/exit via connective tissue coverings.
- Most joints are attached to bones. The attachment of the muscle to the immovable bone is the origin. The attachment to the movable bone is the insertion.
Skeletal Muscle (part 4)
- Each skeletal muscle cell is known as a skeletal muscle fiber.
- Their length can be as long as 30 cm.
- Their diameter can be up to 100 μm.
- The length comes from the fusion of embryonic precursor cells called myoblasts.
- A cell made from the fusion of many others is a syncytium.
Components of a Muscle Fiber
- The illustration displays the components of a muscle fiber, including the nucleus, sarcolemma, sarcoplasmic reticulum, T-tubules, mitochondria, and myofibrils.
Fine Structure of Skeletal Muscle (part 1)
-
Motor end plate: The contact surface of an axon terminal on a muscle cell membrane.
-
Sarcolemma: Muscle cell membrane.
-
Sarcoplasm: Muscle cell cytoplasm.
-
The sarcoplasm contains numerous mitochondria for energy production and glycogen granules for glucose storage.
-
Myofibrils: Rod-like structures that extend throughout the muscle cell.
-
Contains sarcoplasmic reticulum, myoglobin, glycogen, and creatine-PK.
Fine Structure of Skeletal Muscle (part 2)
- Myoglobin: An iron-containing protein that stores oxygen in muscle cells, giving the muscle cells a red color.
- Function of Myoglobin: To store and reserve oxygen for muscle metabolism
- T-tubules: Transverse tubules; function in conduction of depolarization
- SR (sarcoplasmic reticulum): Longitudinal tubules; function in Ca2+ storage.
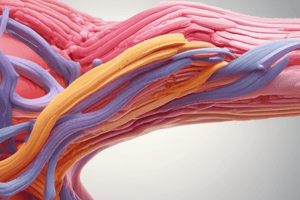
Fine Structure of Skeletal Muscle (part 3)
- Myofibrils: Rod-like structures that extend throughout the muscle cell.
- Composed of myofilaments – thick and thin filaments.
- Myofilaments are comprised of actin (thin), myosin (thick), and regulatory proteins like troponin and tropomyosin.
Myosin Structure (thick myofilaments)
- The myosin protein resembles two golf clubs twisted about each other.
- Approximately 300 myosin molecules join to form a thick filament.
- The head of the myosin forms cross-bridges with the thin filaments.
- The enzyme ATPase (in the head) releases energy for contraction.
Actin Structure (thin myofilaments)
- Formed from three proteins:
- Globular (G) actins: bind to myosin heads.
- Tropomyosin: a long, fibrous protein that regulates the interaction between actin and myosin by covering the binding sites.
- Troponin: binds to calcium, and regulates the position of tropomyosin and thus influences actin-myosin interaction.
The Sarcomere
- Myofibrils are organized into a repetitive pattern known as a sarcomere.
- Myosin forms thick filaments.
- Actin forms thin filaments.
- A band - contains thick filaments (darkened)
- I band - contains thin filaments (lightened)
- H zone – contains only thick filaments.
- Z line - point of attachment of actin fibers.
- M line – myosin fiber centers.
T-Tubules and the SR
- Each muscle fiber has multiple T-tubules.
- Each myofibril has a branch of a T-tubule circling it at each A-I junction.
- The SR expands to form a dilated disc known as the terminal cisterna.
- These structures form a triad (one T-tubule and two terminal cisternae) at each A-I junction.
- Muscle Contraction*:
The Sliding Filament Hypothesis (part 1)
- Hanson and Huxley proposed that skeletal muscle shorten by the sliding of thick and thin filaments.
- The thin filaments slide over the thick filaments, pulling the Z lines closer together.
- When this process happens in all sarcomeres in a muscle fiber, the fiber shortens.
The Sliding Filament Hypothesis (part 2)
- Muscle shortening occurs through the movement of the actin filaments over the myosin filaments.
- Cross-bridges form between actin and myosin filaments.
- The distance between the Z lines of the sarcomere reduces.
Muscle Contraction Steps
- Excitation: The process in which a stimulus causes a change in voltage of the muscle membrane.
- Excitation-contraction coupling: A series of steps connecting excitation to the contraction of myofibrils.
- Contraction: The act of shortening the sarcomere, caused by the interaction of actin and myosin filaments.
- Relaxation: The process that reverts the muscle fiber back to its resting state. The stimulus stops.
Excitation (part 1)
- All cells exhibit a voltage difference across their plasma membrane.
- This membrane potential (Vm) is due to differences in ion concentrations inside and outside the cell. Specifically, high extracellular sodium and high intracellular potassium.
- The cell membrane (plasma membrane) is more permeable to potassium ions (K⁺) than sodium ions (Na⁺). Passive leak of K⁺ causes an overall negative charge inside the cell.
- The Na+/K+ pump actively maintains this imbalance.
Excitation (part 2)
- Plasma membrane proteins, called channels, open and close in response to various signals, altering ion flow and membrane potential.
- There are three types of gated channels:
- Ligand-gated: opening controlled by an extracellular signal
- Voltage-gated: opening controlled by change in membrane potential
- Mechanically gated: opening controlled by mechanical pressure
Excitation (part 3)
- In muscle cells, the neuron-muscle connection is called the neuromuscular junction (NMJ).
- Signals across the NMJ (from neuron to muscle) involve a neurotransmitter called acetylcholine (ACh).
Excitation (part 4)
- The NMJ is the site of interaction between a neuron and a muscle fiber.
- The neurotransmitter is acetylcholine (ACh).
- A bundle of axons carrying signals is called a nerve.
- ACh is released into the synapse (space between the axon and muscle).
The Neuromuscular Junction
- The synaptic cleft is the space between the synaptic end bulb and the muscle cell membrane (sarcolemma).
- The motor end plate is a depression in the sarcolemma containing acetylcholine receptors.
- Acetylcholine is released from synaptic vesicles by exocytosis.
- ACh binds to acetylcholine receptors (nicotinic receptors).
Transmission of Nerve Impulse at the NMJ (part 1)
- A nerve signal causes acetylcholine-containing vesicles to release acetylcholine (ACh).
- ACh diffuses across the synaptic cleft and attaches to ACh receptors.
- ACh receptors are ligand-gated sodium (Na⁺) channels.
- The binding of ACh opens the channels, causing Na⁺ to rush into the muscle cell.
Transmission of Nerve Impulse at the NMJ (part 2)
- The influx of sodium (Na⁺) depolarizes the muscle cell membrane.
- This depolarization is necessary to open voltage-gated channels in the muscle membrane for the next step (excitation-coupling).
Synaptic events
- Illustrated in an image, showing the synaptic events of the NMJ. Note the action potential signal; voltage-gated Ca++ channels; and the release of ACh from the motor neuron.
Characteristics of Neuromuscular Junction
- Signal transmission is unidirectional.
- There is a single NMJ per muscle fiber.
- The neurotransmitter is always acetylcholine (ACh).
- ACh is synthesized from choline and acetyl-CoA, stored in vesicles, and released by Ca²⁺-dependent exocytosis.
- ACh is metabolized by acetylcholinesterase.
- Post-junctional receptors are nicotinic and EPSP/endplate potentials (EPPs) are excitatory and have a high safety margin.
Factors Affecting the NMJ
- Calcium Level: Hypercalcemia inhibits, hypocalcemia increases excitability.
- Hypoxia: Inhibits excitability.
- Drugs: various drugs affect the NMJ (e.g., release inhibitors, blockers, stimulants, anti-cholinesterase).
Excitation-Contraction Coupling (part 1)
- Muscle fiber membrane depolarization triggers the contraction process.
- The process of depolarization initiating contraction is excitation-contraction coupling (ECC).
- Steps in ECC include:
- Action potential initiates and propagates along the motor nerve fiber.
- Arrival at the end feet, opens VG-Ca channels causing Ca influx which causes ACh release.
- Ach diffuses across the synaptic cleft and binds to NR on the muscle membrane.
- Opening of ligand-gated Na+ channels causes Na+ influx which produces EPP.
- Spread of depolarization through the sarcolemma and T tubules.
Excitation-Contraction Coupling (part 2)
- Depolarization triggers release of Ca2+ from the sarcoplasmic reticulum (SR).
- Ca2+ binds to troponin-C, causing a conformational change that detaches tropomyosin from the actin active sites.
- Myosin heads bind to actin, and the sliding filament mechanism begins.
- ATP hydrolysis provides the energy for the power stroke of myosin heads pulling on the actin filaments.
Mechanism of Muscle Relaxation
- Following contraction Ca2+ is reabsorbed by the sarcoplasmic reticulum (SR)
- Calcium release from troponin-C, resulting in the re-covering of the actin-binding sites by tropomyosin.
- The myosin heads detach from actin, and the muscle relaxes, requiring energy by ATP breakdown.
Types of Skeletal Muscle Fibers
- Slow Fibers:
- Contract slowly due to the slow ATPase activity.
- Depend on oxygen delivery and aerobic metabolism.
- Fatigue resistant, High endurance.
- Thin diameter; large amount of cytoplasm impedes oxygen and nutrient diffusion.
- Red fibers; slow oxidative fibers, type-1 fibers.
- Fast Fibers:
- Rapid contraction and high tension development.
- Depend on anaerobic metabolism and use ATP rapidly.
- Fatigue rapidly.
- Fast fatigue (FF) fibers, fast glycolytic (FG) fibers , white fibers.
- Large in diameter containing densely packed myofibrils, large glycogen reserves, and relatively few mitochondria.
Myasthenia Gravis
- Myasthenia Gravis (MG) is characterized by skeletal muscle weakness, fatigue.
- It's an autoimmune disease where antibodies attack acetylcholine receptors (ACh receptors) at the neuromuscular junction (NMJ).
Myasthenia Gravis (Treatment)
- Treatment for MG often involves anticholinesterase drugs (e.g., neostigmine) to increase acetylcholine's effect at the NMJ; as well as using immunosuppressants like steroids.
Smooth Muscle
- Smooth muscle maintains a normal level of activity known as muscle tone.
- Smooth muscle can be excited or inhibited, contracting or relaxing, in response to stimuli such as neurotransmitters, hormones, pH, and metabolites.
Contraction of Smooth Muscle
- Smooth muscle contains both actin and myosin filaments, but doesn't contain tropinin.
- The contraction process is activated by Ca²⁺.
- ATP is required for muscle contraction.
- Ca²⁺ combines with calmodulin to activate myosin kinase, which phosphorylates myosin and triggers contraction.
Cardiac Muscle Contraction
- Release of Ca²⁺ from the SR is triggered by Ca²⁺ influx through the T-tubules.
- Influx of calcium through T-tubules initiate the release of Ca from SR.
- Ca²⁺ binds to troponin, causing contraction. (systole)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.