Podcast
Questions and Answers
Which subunit of troponin binds to tropomyosin?
Which subunit of troponin binds to tropomyosin?
- TnT (correct)
- TnI
- Actin
- TnC
What is the functional unit of muscle contraction?
What is the functional unit of muscle contraction?
- Myofibril
- Actin filament
- Z disc
- Sarcomere (correct)
What is the function of the M line in the sarcomere?
What is the function of the M line in the sarcomere?
- Site of calcium release
- Site of ATP hydrolysis
- Anchoring point for myosin tails (correct)
- Anchoring point for actin filaments
Which protein is responsible for connecting the cytoskeleton of a muscle fiber to the extracellular matrix?
Which protein is responsible for connecting the cytoskeleton of a muscle fiber to the extracellular matrix?
Which statement about myosin and actin is correct?
Which statement about myosin and actin is correct?
What is the main function of the T tubules in muscle cells?
What is the main function of the T tubules in muscle cells?
What happens to the sarcomere during muscle contraction?
What happens to the sarcomere during muscle contraction?
Which of the following proteins help maintain the elastic structure of muscle and transfer tension during contraction?
Which of the following proteins help maintain the elastic structure of muscle and transfer tension during contraction?
What is the typical diameter range for adult skeletal muscle fibers?
What is the typical diameter range for adult skeletal muscle fibers?
Which of the following is a primary function of muscle tissue?
Which of the following is a primary function of muscle tissue?
What are the undifferentiated, mononucleated cells that fuse to form muscle fibers during development?
What are the undifferentiated, mononucleated cells that fuse to form muscle fibers during development?
Which of these properties enables a muscle to recoil to its original resting length after being stretched?
Which of these properties enables a muscle to recoil to its original resting length after being stretched?
When is skeletal muscle differentiation typically considered complete?
When is skeletal muscle differentiation typically considered complete?
How do skeletal muscle fibers typically repair after being damaged after birth due to injury?
How do skeletal muscle fibers typically repair after being damaged after birth due to injury?
Skeletal muscle is characterized by which of the following features?
Skeletal muscle is characterized by which of the following features?
Which type of muscle tissue is found exclusively in the heart?
Which type of muscle tissue is found exclusively in the heart?
What is the primary method through which compensation for loss of muscle tissue occurs?
What is the primary method through which compensation for loss of muscle tissue occurs?
What is required for contracting skeletal muscle fibers?
What is required for contracting skeletal muscle fibers?
What is a key characteristic of smooth muscle?
What is a key characteristic of smooth muscle?
Which statement is true regarding skeletal muscle's nerve and blood supply?
Which statement is true regarding skeletal muscle's nerve and blood supply?
Which muscle type is primarily responsible for peristalsis?
Which muscle type is primarily responsible for peristalsis?
Which feature is unique to cardiac muscle tissue?
Which feature is unique to cardiac muscle tissue?
How do satellite cells aid in muscle repair?
How do satellite cells aid in muscle repair?
What is the term used to describe a single skeletal muscle cell?
What is the term used to describe a single skeletal muscle cell?
What layer of connective tissue surrounds each individual muscle fiber?
What layer of connective tissue surrounds each individual muscle fiber?
What is the primary function of myofibrils within a muscle fiber?
What is the primary function of myofibrils within a muscle fiber?
Which connective tissue layer surrounds groups of muscle fibers, also known as fascicles?
Which connective tissue layer surrounds groups of muscle fibers, also known as fascicles?
What are the two types of myofilaments that make up myofibrils?
What are the two types of myofilaments that make up myofibrils?
Which protein primarily composes thick filaments in muscle fibers?
Which protein primarily composes thick filaments in muscle fibers?
What role does tropomyosin play in muscle contraction?
What role does tropomyosin play in muscle contraction?
What structure is formed when collagen fibers of the connective tissue layers come together at each end of a muscle?
What structure is formed when collagen fibers of the connective tissue layers come together at each end of a muscle?
Which part of the myosin molecule serves as an enzyme for hydrolyzing ATP?
Which part of the myosin molecule serves as an enzyme for hydrolyzing ATP?
What is the primary role of the sarcoplasmic reticulum (SR) in skeletal muscle cells?
What is the primary role of the sarcoplasmic reticulum (SR) in skeletal muscle cells?
How do T tubules relate to terminal cisternae in skeletal muscle?
How do T tubules relate to terminal cisternae in skeletal muscle?
What is the resting membrane potential (RMP) of skeletal muscle cells?
What is the resting membrane potential (RMP) of skeletal muscle cells?
What is the final stimulus for contraction in skeletal muscles?
What is the final stimulus for contraction in skeletal muscles?
Which of the following events is NOT part of the process for skeletal muscle contraction?
Which of the following events is NOT part of the process for skeletal muscle contraction?
Which type of muscle action potential duration is longer?
Which type of muscle action potential duration is longer?
What is the primary function of calsequestrin within terminal cisternae?
What is the primary function of calsequestrin within terminal cisternae?
What is the approximate conduction speed of action potential along the skeletal muscle membrane?
What is the approximate conduction speed of action potential along the skeletal muscle membrane?
What is the primary function of the nicotinic ACh receptors located at the postsynaptic membrane?
What is the primary function of the nicotinic ACh receptors located at the postsynaptic membrane?
Which structure is found between the nerve terminal and the muscle cell?
Which structure is found between the nerve terminal and the muscle cell?
What initiates the release of acetylcholine from the vesicles in the nerve terminal?
What initiates the release of acetylcholine from the vesicles in the nerve terminal?
What is the result of the endplate potential generated at the postsynaptic membrane?
What is the result of the endplate potential generated at the postsynaptic membrane?
Which substance in the synaptic cleft is responsible for breaking down acetylcholine?
Which substance in the synaptic cleft is responsible for breaking down acetylcholine?
What change occurs to the postsynaptic membrane when acetylcholine binds to its receptors?
What change occurs to the postsynaptic membrane when acetylcholine binds to its receptors?
What role do mitochondria play in the nerve terminal of the neuromuscular junction?
What role do mitochondria play in the nerve terminal of the neuromuscular junction?
How does the muscle cell membrane respond to the increase in permeability caused by ACh binding?
How does the muscle cell membrane respond to the increase in permeability caused by ACh binding?
Flashcards
Muscle Cells
Muscle Cells
The specialized cells responsible for converting chemical energy into mechanical energy, enabling muscle contractions and movement.
Contractility
Contractility
The property of muscle tissue that allows it to shorten forcefully, generating tension and pulling on bones or other structures.
Excitability
Excitability
The capacity of muscle tissue to respond to stimuli, such as nerve impulses or chemical signals.
Extensibility
Extensibility
Signup and view all the flashcards
Elasticity
Elasticity
Signup and view all the flashcards
Skeletal Muscle
Skeletal Muscle
Signup and view all the flashcards
Cardiac Muscle
Cardiac Muscle
Signup and view all the flashcards
Smooth Muscle
Smooth Muscle
Signup and view all the flashcards
Endomysium
Endomysium
Signup and view all the flashcards
Perimysium
Perimysium
Signup and view all the flashcards
Epimysium
Epimysium
Signup and view all the flashcards
Sarcoplasma
Sarcoplasma
Signup and view all the flashcards
Sarcolemma
Sarcolemma
Signup and view all the flashcards
Thick filaments (Myosin)
Thick filaments (Myosin)
Signup and view all the flashcards
Thin filaments (Actin, Troponin, Tropomyosin)
Thin filaments (Actin, Troponin, Tropomyosin)
Signup and view all the flashcards
Myosin binding sites on actin
Myosin binding sites on actin
Signup and view all the flashcards
Muscle fiber
Muscle fiber
Signup and view all the flashcards
Myoblasts
Myoblasts
Signup and view all the flashcards
Muscle fiber differentiation
Muscle fiber differentiation
Signup and view all the flashcards
Satellite cells
Satellite cells
Signup and view all the flashcards
Muscle hypertrophy
Muscle hypertrophy
Signup and view all the flashcards
Muscle connective tissue sheaths
Muscle connective tissue sheaths
Signup and view all the flashcards
Nerve supply to muscle fiber
Nerve supply to muscle fiber
Signup and view all the flashcards
Blood supply to muscle fibers
Blood supply to muscle fibers
Signup and view all the flashcards
Troponin
Troponin
Signup and view all the flashcards
TnI (Troponin I)
TnI (Troponin I)
Signup and view all the flashcards
TnT (Troponin T)
TnT (Troponin T)
Signup and view all the flashcards
TnC (Troponin C)
TnC (Troponin C)
Signup and view all the flashcards
Sarcomere
Sarcomere
Signup and view all the flashcards
Titin
Titin
Signup and view all the flashcards
Actinin
Actinin
Signup and view all the flashcards
Dystrophin
Dystrophin
Signup and view all the flashcards
Sarcoplasmic Reticulum (SR)
Sarcoplasmic Reticulum (SR)
Signup and view all the flashcards
Longitudinal Element of SR
Longitudinal Element of SR
Signup and view all the flashcards
Terminal Cisternae of SR
Terminal Cisternae of SR
Signup and view all the flashcards
Calsequestrin
Calsequestrin
Signup and view all the flashcards
Muscle Triad
Muscle Triad
Signup and view all the flashcards
Neuromuscular Junction
Neuromuscular Junction
Signup and view all the flashcards
Motor Unit
Motor Unit
Signup and view all the flashcards
Impulse Transmission at the Neuromuscular Junction
Impulse Transmission at the Neuromuscular Junction
Signup and view all the flashcards
Presynaptic Portion of Neuromuscular Junction
Presynaptic Portion of Neuromuscular Junction
Signup and view all the flashcards
Acetylcholine Vesicles
Acetylcholine Vesicles
Signup and view all the flashcards
Postsynaptic Portion of Neuromuscular Junction
Postsynaptic Portion of Neuromuscular Junction
Signup and view all the flashcards
Postjunctional Folds
Postjunctional Folds
Signup and view all the flashcards
Nicotinic Acetylcholine Receptors
Nicotinic Acetylcholine Receptors
Signup and view all the flashcards
Synaptic Cleft
Synaptic Cleft
Signup and view all the flashcards
Acetylcholinesterase (AChE)
Acetylcholinesterase (AChE)
Signup and view all the flashcards
Endplate Potential (EPP)
Endplate Potential (EPP)
Signup and view all the flashcards
Study Notes
Muscle Physiology Overview
- Muscle tissue constitutes 50% of the body weight.
- Muscle cells are specialized for converting chemical energy (ATP) into mechanical energy.
- Several types of muscle exist, each adapted for specific functions (e.g., locomotion, blood pumping, peristalsis).
Muscular System Functions
- Body movement.
- Maintenance of posture.
- Respiration.
- Production of body heat.
- Communication (speech, writing, expression).
- Constricting organs and vessels.
- Heart beat.
Properties of Muscle
- Contractility: Ability to shorten with force.
- Excitability: Ability to respond to a stimulus.
- Extensibility: Ability to be stretched.
- Elasticity: Ability to recoil to original resting length after stretching.
Muscle Tissue Types
- Skeletal Muscle:
- Attached to bones.
- Multinucleated and striated.
- Voluntary control (conscious action) and involuntary control (reflexes).
- Cardiac Muscle:
- Found only in the heart.
- Striated, but branching pattern and intercalated discs.
- Involuntary and automatic.
- Usually single nucleus.
- Smooth Muscle:
- Found in walls of hollow organs, blood vessels, etc.
- Non-striated.
- Involuntary.
- Single nucleus.
Skeletal Muscle (Striated Muscle)
-
Attaches to the skeleton.
-
Microscopically displays striations.
-
Is voluntary, controlled consciously.
-
Multinucleated cells.
-
Cells have diameters between 10 and 100 μm and lengths extending up to 25 cm.
Skeletal Muscle Fibers Repair
- Skeletal muscle fibers damaged after birth cannot be replaced by the division of existing muscle fibers.
- However, new fibers can be formed from undifferentiated satellite cells.
- Satellite cells are located adjacent to the muscle fibers and differentiate similar to embryonic myoblasts.
Skeletal Muscle: Nerve and Blood Supply
- Each muscle is typically served by a nerve, an artery, and one or more veins.
- Nerves, arteries, and veins enter near the central part of the muscle and branch throughout it.
- Each muscle fiber (cell) is supplied with a nerve ending that controls contraction.
- Contracting fibers require a continuous supply of oxygen and nutrients via arteries.
- Muscle cells produce metabolic wastes that are removed via veins.
Skeletal Muscle – CT Sheaths
- Skeletal muscles are surrounded by three connective tissue sheaths.
- Endomysium: Delicate connective tissue surrounding each muscle fiber (cell).
- Perimysium: Connective tissue surrounding groups of muscle fibers.
- Epimysium: Dense regular connective tissue surrounding the entire muscle.
- Tendon or aponeurosis formation at the end of the muscle is formed by the collagen fibers of these 3 sheaths uniting.
- They provide support, strength, flexibility, and electrical insulation.
Microscopic Anatomy – Skeletal Muscle Fiber
- Sarcoplasm: Muscle cell cytoplasm.
- Sarcolemma: Muscle cell membrane.
- Within the muscle fiber (cell), there are also myofibrils, sarcoplasmic reticulum, and T-tubules.
- Sarcoplasm contains glycosomes (granules of glycogen) and myoglobin (oxygen-binding protein).
Myofibrils and Striations
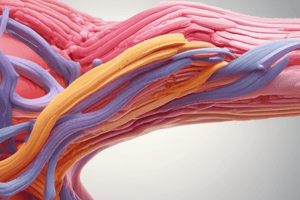
- Each muscle fiber is made from many myofibrils containing the contractile elements of skeletal muscle cells.
- Myofibrils compose about 80% of the muscle volume.
- Myofibrils are made up of myofilaments (thick and thin).
Myofilaments: Thick and Thin
- Thick filaments: Composed of myosin protein.
- Thin filaments: Composed of actin protein, and regulatory proteins tropomyosin and troponin.
- Myosin consists of two heads and one tail.
- Actin is a major component of the thin filament; there are myosin binding sites on actin in the thin filament.
- Tropomyosin molecules are long filaments that spiral around actin and block active sites in a relaxed muscle fiber.
- Troponin molecules bind to tropomyosin and actin, and bind calcium ions, triggering contraction.
- A band in myofibrils/muscle contains the thick filaments, and is made up of parts of thick and thin filaments.
### Structure of Actin and Myosin
- Describe the structure of actin and myosin filaments, including their components (heavy and light chains, hinge regions, etc.), and their role in sarcomere structure.
Myofibrils - Striations - Banding
- The arrangement of myofibrils creates a repeating series of dark (A bands) and light (I bands) bands.
- Each segment is a sarcomere, the smallest functional contractile unit of a muscle.
- Specific regions within a sarcomere include the Z line (or disc), H zone or band, and M line.
- There are thick filaments in the A band, and thick and thin filaments in both the A and I bands.
Sarcomere Shortening
- Actin filaments move towards the center of the sarcomere.
- The sarcomere shortens when the Z disks move closer together.
- A and I bands change in appearance as the muscle contracts and shortens.
Ca2+ and the Contraction Mechanism
- Calcium ions and regulatory proteins (troponin, tropomyosin) are essential for muscle contraction.
- At low intracellular calcium levels, tropomyosin blocks the binding sites of actin, and myosin cannot bind.
- Increasing intracellular calcium causes a conformational change in troponin, causing tropomyosin to move away from the actin binding sites, allowing the myosin head to attach and detach and initiating the power stroke cycle.
Neuromuscular Junction
- Junction where the motor neuron stimulates the muscle fiber.
- The axon of the motor neuron branches into several terminals forming the presynaptic part of the neuromuscular junction.
- The postsynaptic part of the junction is the muscle cell membrane, with folds containing nicotinic ACh receptors.
- The pre- and postsynaptic membranes are separated by the synaptic cleft, containing acetylcholinesterase (AChE).
Electrical Events at the Neuromuscular Junction
- Depolarization of the nerve terminal causes the release of acetylcholine (ACh) into the synaptic cleft.
- ACh binds to receptors on the muscle fiber, leading to depolarization (end-plate potential).
- Depolarization triggers an action potential in the muscle fiber, initiating muscle contraction.
Propagation of Action Potential on Muscle Membrane
- The action potential spreads through the T tubules.
- This stimulates the release of calcium ions from the SR, causing muscle contraction through the cross-bridge cycle.
Dihydropyridine and Ryanodine Receptors
- Action potentials in T-tubules activate DHP receptors, causing the release of calcium ions from the sarcoplasmic reticulum terminal cisternae.
- Calcium ions initiate muscle contraction.
Neuromuscular Transmission (Toxins and Drugs)
- Presynaptic blockade (e.g., Botulinum toxin) interferes with ACh release.
- Postsynaptic blockade (e.g., Curare-Tubocurarine) prevents ACh from binding and triggering a muscle contraction.
Sliding Filament Model of Contraction
- The sliding filament model explains how muscle fibers shorten during contraction.
- Myosin heads bind to actin filaments, causing them to slide past each other.
- The cross bridge cycle describes the individual steps involved in the overlapping, sliding filament mechanism of the contraction process.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.