Podcast
Questions and Answers
What effect does the activation of M2 muscarinic receptors in the heart have on heart rate?
What effect does the activation of M2 muscarinic receptors in the heart have on heart rate?
- Causes irregular heartbeats
- Increases heart rate
- Decreases heart rate (correct)
- Has no effect on heart rate
Which of the following drugs is classified as a cholinergic receptor blocking drug?
Which of the following drugs is classified as a cholinergic receptor blocking drug?
- Bethanechol
- Carbachol
- Pilocarpine
- Atropine (correct)
What is the primary effect of M3 receptor activation in the bladder?
What is the primary effect of M3 receptor activation in the bladder?
- Relaxation of the bladder
- Contraction of the bladder (correct)
- Increased urinary frequency
- Dilation of urinary passages
Which of the following describes the effect of M3 receptor activation on secretions?
Which of the following describes the effect of M3 receptor activation on secretions?
What type of structural classification do direct-acting cholinergic agonists belong to?
What type of structural classification do direct-acting cholinergic agonists belong to?
Which effect occurs due to blocking cholinergic activity?
Which effect occurs due to blocking cholinergic activity?
Activation of which muscarinic receptor subtype may lead to improved cognition?
Activation of which muscarinic receptor subtype may lead to improved cognition?
What is the result of M3 receptor activation in the gastrointestinal tract?
What is the result of M3 receptor activation in the gastrointestinal tract?
Which compound is specifically used to treat glaucoma?
Which compound is specifically used to treat glaucoma?
What is the clinical use of Bethanechol?
What is the clinical use of Bethanechol?
Which compound has selective binding to M3 muscarinic receptors?
Which compound has selective binding to M3 muscarinic receptors?
What type of receptors does ACh bind to in somatic motor neurons?
What type of receptors does ACh bind to in somatic motor neurons?
Which of the following substantiates the cause of one type of mushroom poisoning?
Which of the following substantiates the cause of one type of mushroom poisoning?
What is a key characteristic of Acetylcholine in relation to cholinesterase hydrolysis?
What is a key characteristic of Acetylcholine in relation to cholinesterase hydrolysis?
Which statement accurately describes parasympathomimetic drugs?
Which statement accurately describes parasympathomimetic drugs?
In which scenario does the sympathetic response increase?
In which scenario does the sympathetic response increase?
Which cholinergic compound does not have an effect on nicotinic receptors?
Which cholinergic compound does not have an effect on nicotinic receptors?
Which of the following compounds primarily targets muscarinic receptors with a low level of nicotinic activity?
Which of the following compounds primarily targets muscarinic receptors with a low level of nicotinic activity?
Which of the following neurons release ACh that binds to muscarinic receptors?
Which of the following neurons release ACh that binds to muscarinic receptors?
Which drug is classified as a synthetic muscarinic agonist?
Which drug is classified as a synthetic muscarinic agonist?
What effect do cholinolytic drugs have on the cholinergic system?
What effect do cholinolytic drugs have on the cholinergic system?
Which of the following is true of sympathetic postganglionic neurons in relation to ACh?
Which of the following is true of sympathetic postganglionic neurons in relation to ACh?
What defines cholinomimetic drugs?
What defines cholinomimetic drugs?
How do parasympatholytic drugs influence the autonomic nervous system?
How do parasympatholytic drugs influence the autonomic nervous system?
What is the primary ocular effect of M3 antagonists like cyclopentolate and tropicamide?
What is the primary ocular effect of M3 antagonists like cyclopentolate and tropicamide?
Which condition is contraindicated with the use of antimuscarinics due to potential complications?
Which condition is contraindicated with the use of antimuscarinics due to potential complications?
What effect do antimuscarinics have on bronchial muscle contraction?
What effect do antimuscarinics have on bronchial muscle contraction?
Which of the following is a common side effect caused by antimuscarinics on the eyes?
Which of the following is a common side effect caused by antimuscarinics on the eyes?
How are ipratropium and tiotropium administered for therapeutic effects?
How are ipratropium and tiotropium administered for therapeutic effects?
What effect does the relaxation of the ciliary muscle have in the context of antimuscarinics?
What effect does the relaxation of the ciliary muscle have in the context of antimuscarinics?
What role do antimuscarinics play before the administration of inhalant anesthetics?
What role do antimuscarinics play before the administration of inhalant anesthetics?
Which of the following best describes the mechanism of action of antimuscarinics on muscarinic receptors?
Which of the following best describes the mechanism of action of antimuscarinics on muscarinic receptors?
What is a common side effect of antimuscarinic treatment?
What is a common side effect of antimuscarinic treatment?
How does the antagonism of M3 receptors affect the gastrointestinal tract?
How does the antagonism of M3 receptors affect the gastrointestinal tract?
Which drug is primarily used to treat GI spasms and cramps?
Which drug is primarily used to treat GI spasms and cramps?
What effect do antimuscarinics have on urinary function?
What effect do antimuscarinics have on urinary function?
What condition may be precipitated by antimuscarinic agents in elderly men?
What condition may be precipitated by antimuscarinic agents in elderly men?
Which effect is NOT associated with antihistamines that have anticholinergic properties?
Which effect is NOT associated with antihistamines that have anticholinergic properties?
What is the use of antihistamines with antimuscarinic effects?
What is the use of antihistamines with antimuscarinic effects?
What is a potential central nervous system side effect of high doses of antihistamines with antimuscarinic effects?
What is a potential central nervous system side effect of high doses of antihistamines with antimuscarinic effects?
What is a notable effect of M2 muscarinic receptor activation in the cardiovascular system?
What is a notable effect of M2 muscarinic receptor activation in the cardiovascular system?
Which effect is associated with M3 receptor activation in the smooth muscle of the bladder?
Which effect is associated with M3 receptor activation in the smooth muscle of the bladder?
What common side effect can result from antimuscarinic drug administration?
What common side effect can result from antimuscarinic drug administration?
Which drug category inhibits the cholinergic system?
Which drug category inhibits the cholinergic system?
What is the effect of M3 receptor activation on exocrine gland secretions?
What is the effect of M3 receptor activation on exocrine gland secretions?
Which factor differentiates chemical structures of direct-acting cholinergic agonists?
Which factor differentiates chemical structures of direct-acting cholinergic agonists?
Which compound is primarily used to increase salivary and lacrimal secretions?
Which compound is primarily used to increase salivary and lacrimal secretions?
Which drug selectively activates M3 muscarinic receptors?
Which drug selectively activates M3 muscarinic receptors?
What is a potential effect of cholinomimetic drugs on the central nervous system?
What is a potential effect of cholinomimetic drugs on the central nervous system?
What is a clinical use of Bethanechol?
What is a clinical use of Bethanechol?
What is an expected outcome of M3 receptor antagonism in the eye?
What is an expected outcome of M3 receptor antagonism in the eye?
Which of the following compounds does not undergo hydrolysis by cholinesterase?
Which of the following compounds does not undergo hydrolysis by cholinesterase?
Which compound is associated with one type of mushroom poisoning?
Which compound is associated with one type of mushroom poisoning?
How is Carbachol classified in terms of receptor specificity?
How is Carbachol classified in terms of receptor specificity?
What clinical condition does Pilocarpine primarily treat?
What clinical condition does Pilocarpine primarily treat?
What effect does Methacholine primarily have on cholinesterase hydrolysis?
What effect does Methacholine primarily have on cholinesterase hydrolysis?
What effect do muscarinic agonist drugs have on patients with asthma?
What effect do muscarinic agonist drugs have on patients with asthma?
Which of the following drugs can be used for the treatment of dry mouth (xerostomia)?
Which of the following drugs can be used for the treatment of dry mouth (xerostomia)?
What is the primary role of muscarinic receptor antagonists?
What is the primary role of muscarinic receptor antagonists?
Which of the following compounds is a natural muscarinic receptor antagonist found in solanaceous plants?
Which of the following compounds is a natural muscarinic receptor antagonist found in solanaceous plants?
How do cholinomimetic drugs primarily function within the body?
How do cholinomimetic drugs primarily function within the body?
What physiological effect is associated with stimulation of the bladder detrusor muscle?
What physiological effect is associated with stimulation of the bladder detrusor muscle?
How do antimuscarinic agents affect bronchial muscle contraction?
How do antimuscarinic agents affect bronchial muscle contraction?
What is a potential side effect of using cholinergic receptor blocking drugs?
What is a potential side effect of using cholinergic receptor blocking drugs?
What is the main active compound found in deadly nightshade?
What is the main active compound found in deadly nightshade?
Hyoscine butylbromide is commonly used for which of the following purposes?
Hyoscine butylbromide is commonly used for which of the following purposes?
Which of the following accurately describes the nature of atropine?
Which of the following accurately describes the nature of atropine?
What can be a consequence of consuming Jimson weed seeds?
What can be a consequence of consuming Jimson weed seeds?
What are synthetic antimuscarinics primarily developed for?
What are synthetic antimuscarinics primarily developed for?
Atropine's effects in low doses include which of the following?
Atropine's effects in low doses include which of the following?
What distinguishes tertiary ammonium compounds like atropine and hyoscine from quaternary ammonium compounds?
What distinguishes tertiary ammonium compounds like atropine and hyoscine from quaternary ammonium compounds?
Tachycardia is a potential effect of which dosage level of atropine?
Tachycardia is a potential effect of which dosage level of atropine?
What is the primary result of M3 receptor antagonism on gastrointestinal function?
What is the primary result of M3 receptor antagonism on gastrointestinal function?
Which medication is indicated for treating an overactive bladder by relaxing the bladder detrusor muscle?
Which medication is indicated for treating an overactive bladder by relaxing the bladder detrusor muscle?
Which antimuscarinic side effect is associated with first-generation antihistamines?
Which antimuscarinic side effect is associated with first-generation antihistamines?
What complication can arise from antimuscarinic treatment in elderly men?
What complication can arise from antimuscarinic treatment in elderly men?
In what condition can antihistamines with anticholinergic effects be particularly beneficial?
In what condition can antihistamines with anticholinergic effects be particularly beneficial?
What is a common side effect of using antimuscarinics on the salivary glands?
What is a common side effect of using antimuscarinics on the salivary glands?
What physiological change occurs in the bladder due to M3 receptor antagonism?
What physiological change occurs in the bladder due to M3 receptor antagonism?
What effect does the use of hyoscine butylbromide have on the gastrointestinal tract?
What effect does the use of hyoscine butylbromide have on the gastrointestinal tract?
Flashcards are hidden until you start studying
Study Notes
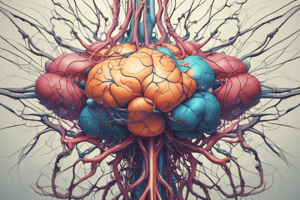
Muscarinic Receptors
- Muscarinic receptors are activated by acetylcholine, a neurotransmitter responsible for various bodily functions.
- M1 receptors: Found in the central nervous system (CNS), and stimulation may cause tremor, hypothermia, and improved cognition. Antagonists can cause sedation, reduce involuntary movement, and rigidity.
- M2 receptors: Located in the heart, and stimulation causes a decrease in heart rate and force of contraction, as well as generalised vasodilation and lowered blood pressure. Antagonists have modest tachycardia effects.
- M3 receptors: Found in various locations:
- Gastrointestinal Tract (GIT): Stimulation causes contraction of smooth muscle, increasing GI motility. Antagonists decrease motility.
- Bladder and Bronchi: Stimulation causes contraction of smooth muscle. Antagonists cause relaxation, potentially leading to urinary retention.
- Exocrine glands (sweat, lacrimal, salivary, bronchial): Stimulation increases secretion. Antagonists decrease secretion.
- Eye: Stimulation causes contraction of the ciliary muscle, resulting in pupil constriction. Antagonists dilate pupils and increase intraocular pressure.
Muscarinic Agonists
- Muscarinic agonists mimic the effects of acetylcholine by binding to and activating cholinergic receptors.
- Several types of muscarinic agonists exist, classified into three groups:
- Choline esters: Acetylcholine, carbachol, methacholine, and bethanechol. Vary in their affinity for muscarinic and nicotinic receptors and susceptibility to hydrolysis by cholinesterase enzymes.
- Plant alkaloids: Muscarine, nicotine, pilocarpine, and cevimeline. These also differ in their affinity and susceptibility to cholinesterase enzymes.
- Synthetics: Varenicline and cevimeline.
- Clinical uses: These drugs are utilized to treat a variety of conditions, including:
- Urinary and GI hypotonia (bethanechol)
- Glaucoma (pilocarpine)
- Sjogren's syndrome (cevimeline)
Antimuscarinic Drugs
- Antimuscarinic (cholinolytic) drugs work by blocking muscarinic receptors, preventing acetylcholine from activating them.
- This effectively inhibits the parasympathetic nervous system, leading to an increase in sympathetic response.
- Different antimuscarinic drugs have varying selectivity for specific muscarinic receptor subtypes (M1, M2, M3, M4, M5).
- The effects of antimuscarinic drugs depend on their receptor selectivity and the targeted tissue.
Ocular Effects of Antimuscarinics
- Antimuscarinics relax the iris sphincter muscle, resulting in pupil dilation (mydriasis).
- They also relax the ciliary muscle, causing paralysis of accommodation (cycloplegia) and impairing near vision.
- Antimuscarinics can increase intraocular pressure by impairing the outflow of aqueous humor, making them contraindicated in glaucoma.
- They can inhibit lacrimal gland secretion, leading to dry eyes.
- Cyclopentolate and tropicamide are used as eye drops to facilitate fundoscopy (examine the back of the eye).
Respiratory Effects of Antimuscarinics
- Antagonism of M3 receptors in the airways leads to:
- Decreased bronchial muscle contraction (bronchodilation).
- Inhibition of secretions in the upper and lower respiratory tract..
- Ipratropium and tiotropium are inhaled bronchodilators used for asthma and COPD.
- Antimuscarinics can be used pre-operatively to reduce secretions and the possibility of laryngospasm during inhalation anesthesia.
GIT Effects of Antimuscarinics
- Antagonism at M3 receptors in the GIT results in: - Decreased salivary, gastric and other secretions, leading to dry mouth, a common side effect. - Decreased GIT motility due to reduced contraction of smooth muscle, leading to decreased tone and propulsive movements, prolonged gastric emptying time, and increased intestinal transit time. - Hyoscine butylbromide is used to treat GI spasm and cramps, but atropine is not recommended for diarrhoea.
Urinary Tract Effects of Antimuscarinics
-
Antagonism of M3 receptors in the bladder:
- Relaxes the bladder detrusor muscle.
- Contracts the internal sphincter of the bladder.
- Combined effect inhibits micturition.
-
Oxybutinin and darifenacin are used to treat overactive bladder, incontinence, and frequent urination. However, antimuscarinics can cause urinary retention, particularly in elderly men with prostatic enlargement.
Antimuscarinic Effects of Antihistamines
- Several first-generation antihistamines (H1 receptor antagonists), in addition to their antihistamine effects, also possess anticholinergic effects at muscarinic receptors, especially at M3 receptors in the GIT.
- Some antihistamines are used to manage nausea, vomiting, vertigo, and motion sickness due to their antimuscarinic effects. However, they can also cause side effects typical of antimuscarinics, such as:
- Dry mouth.
- Blurred vision.
- Tachycardia.
- Urinary retention.
- Hallucinations (at high doses).
Muscarinic receptors
- Muscarinic receptors are a class of acetylcholine receptors that are found in the peripheral nervous system.
- They are involved in a variety of functions, including regulating heart rate, smooth muscle contraction, and gland secretions.
- Muscarinic agonists stimulate these receptors, leading to effects similar to those caused by acetylcholine.
- Muscarinic antagonists block these receptors, preventing acetylcholine from binding and therefore inhibiting its actions.
Muscarinic agonists
- Muscarinic agonists are divided into three main groups based on their chemical structures: choline esters, plant alkaloids, and synthetic drugs.
Choline esters
- Acetylcholine is the naturally occurring neurotransmitter of the parasympathetic nervous system.
- Carbachol is a cholinergic agonist that is more resistant to breakdown than acetylcholine.
- Methacholine is similar to acetylcholine but has a shorter duration of action than acetylcholine.
- Bethanechol is used to treat bladder and GI hypotonia.
Plant alkaloids
- Muscarine is found in poisonous mushrooms and can cause severe poisoning.
- Pilocarpine is used to treat glaucoma by constricting the pupil and reducing intraocular pressure.
- Cevimeline is selective for M3 receptors and is used to treat Sjogren's syndrome by increasing salivary and lacrimal secretions.
Synthetic drugs
- Varenicline is a partial nicotinic receptor agonist used for smoking cessation.
Muscarinic receptor subtypes
- M1 receptors are found in the central nervous system and are involved in cognition, learning, and memory.
- M2 receptors are located in the heart and are involved in the regulation of heart rate and contractility.
- M3 receptors are found in smooth muscle and glands and are responsible for smooth muscle contraction and the secretion of saliva, sweat, and gastric juices.
Muscarinic antagonists
- Muscarinic antagonists are also known as cholinergic receptor blocking drugs or anticholinergics.
- These drugs inhibit the activation of cholinergic receptors by blocking the binding of acetylcholine.
- This leads to decreased parasympathetic activity and an overall increase in sympathetic effects.
Atropine and Hyoscine
- Atropine and hyoscine (also known as scopolamine) are naturally occurring belladonna alkaloids found in solanaceous plants.
- They are both tertiary ammonium compounds that are lipophilic and can cross the blood-brain barrier, affecting the central nervous system.
- These compounds can be highly toxic and have been implicated in accidental or intentional poisonings.
Synthetic Muscarinic Antagonists
- Hyoscine butylbromide (Buscopan) is a synthetic antimuscarinic drug commonly used to relieve intestinal, ureteric, and uterine cramps.
- Oxybutinin and darifenacin are used to treat overactive bladder, incontinence, and frequent urination.
Anticholinergic side effects
- Dry mouth is a common side effect of antimuscarinic drugs, especially with higher doses.
- Blurred vision can also occur due to the relaxation of the ciliary muscle in the eye.
- Tachycardia (increased heart rate) can be caused by the blocking of M2 receptors in the heart.
- Urinary retention can occur due to the relaxation of the bladder detrusor muscle and the contraction of the internal sphincter of the bladder.
- Hallucinations can occur at high doses, especially with atropine and hyoscine.
First-generation antihistamines
- Several first-generation antihistamine drugs (H1 receptor antagonists) also have anticholinergic effects.
- Due to their antimuscarinic effects, these antihistamines can be useful for managing nausea, vomiting, vertigo, and motion sickness, but can also have side effects such as dry mouth, blurred vision, tachycardia, and urinary retention.
GIT effects of antimuscarinic drugs
- Decreased salivation, gastric, and other secretions in the GIT can be a symptom of antimuscarinic drug use.
- Decreased GIT motility can also occur, leading to slower gastric emptying and increased intestinal transit time.
Urinary tract effects of antimuscarinic drugs
- Relaxation of the bladder detrusor muscle and contraction of the internal sphincter of the bladder can cause urinary retention, a potential side effect of antimuscarinic drugs.
Therapeutic uses of Muscarinic Agonists and Antagonists
- Glaucoma: Pilocarpine is used to treat glaucoma by constricting the pupil and reducing intraocular pressure.
- Dry Mouth (Xerostomia): Pilocarpine and cevimeline are used to treat dry mouth in conditions like Sjogren's syndrome.
- Overactive Bladder: Oxybutinin and darifenacin are used to treat an overactive bladder, incontinence, and frequent urination.
- Smoking Cessation: Varenicline is a partial nicotinic receptor agonist used for smoking cessation.
- Gastrointestinal Spasm and Cramps: Hyoscine butylbromide (Buscopan) is used to relieve intestinal, ureteric, and uterine cramps.
Important Notes
- Drug interactions: Antimuscarinic drugs can interact with other medications, increasing their effects and possibly causing adverse reactions.
- Individual variability: The effects of cholinergic drugs can vary based on individual factors, such as age, health status, and genetic makeup.
- Careful monitoring: It is important to monitor patients carefully when they are taking cholinergic drugs to ensure safe and effective treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.