Podcast
Questions and Answers
What is the primary mode of action for M1, M3, and M5 muscarinic receptors?
What is the primary mode of action for M1, M3, and M5 muscarinic receptors?
- Inhibit adenylyl cyclase
- Regulate ion channels via Gi and Go
- Directly activate nicotinic receptors
- Activate the Gq-PLC pathway (correct)
Which muscarinic receptor subtype is primarily involved in the modulation of nicotinic cholinergic transmission in the ganglia?
Which muscarinic receptor subtype is primarily involved in the modulation of nicotinic cholinergic transmission in the ganglia?
- M4
- M2
- M1 (correct)
- M5
What effect do M2 and M4 muscarinic receptors have on cellular activity?
What effect do M2 and M4 muscarinic receptors have on cellular activity?
- They inhibit adenylyl cyclase (correct)
- They stimulate adenylyl cyclase
- They enhance polyphosphoinositides hydrolysis
- They activate the Gq-PLC pathway
Which muscarinic receptor subtype has effects on the hydrolysis of polyphosphoinositides?
Which muscarinic receptor subtype has effects on the hydrolysis of polyphosphoinositides?
What is a common therapeutic use of muscarinic receptor agonists?
What is a common therapeutic use of muscarinic receptor agonists?
Which statement correctly describes the structure of muscarinic receptors?
Which statement correctly describes the structure of muscarinic receptors?
What is a significant toxicological consideration with muscarinic receptor antagonists?
What is a significant toxicological consideration with muscarinic receptor antagonists?
Which of the following is a characteristic of the pharmacological effects of acetylcholine?
Which of the following is a characteristic of the pharmacological effects of acetylcholine?
Which muscarinic receptor agonist effect is primarily associated with the M2 receptor subtype?
Which muscarinic receptor agonist effect is primarily associated with the M2 receptor subtype?
What is the dominant cardiovascular response when administering atropine?
What is the dominant cardiovascular response when administering atropine?
Why is atropine not the preferred choice for treating patients with COPD?
Why is atropine not the preferred choice for treating patients with COPD?
What receptor primarily mediates the increase in secretory activity of the stomach and intestines?
What receptor primarily mediates the increase in secretory activity of the stomach and intestines?
How does atropine administration affect the heart rate at maximal exertion?
How does atropine administration affect the heart rate at maximal exertion?
What happens to heart rate at average clinical doses of atropine?
What happens to heart rate at average clinical doses of atropine?
What effect does the activation of M2 and M3 receptors have on norepinephrine (NE) release?
What effect does the activation of M2 and M3 receptors have on norepinephrine (NE) release?
In the SA node, what is the primary outcome of increased intracellular calcium affecting heart rate?
In the SA node, what is the primary outcome of increased intracellular calcium affecting heart rate?
What limits the systemic administration of acetylcholine (ACh)?
What limits the systemic administration of acetylcholine (ACh)?
Which of the following is true regarding the effect of atropine on presynaptic M1 receptors?
Which of the following is true regarding the effect of atropine on presynaptic M1 receptors?
Which inhaled medications are preferred over atropine for COPD patients?
Which inhaled medications are preferred over atropine for COPD patients?
How does the activation of M3 receptors affect salivary secretion?
How does the activation of M3 receptors affect salivary secretion?
Which of the following is NOT a site where cholinergic synapses occur?
Which of the following is NOT a site where cholinergic synapses occur?
What is the impact of cholinergic agonists on the atrioventricular (AV) node?
What is the impact of cholinergic agonists on the atrioventricular (AV) node?
What is one of the pharmacological effects of acetylcholine on the cardiovascular system?
What is one of the pharmacological effects of acetylcholine on the cardiovascular system?
Which muscarinic receptor is primarily responsible for bronchoconstriction?
Which muscarinic receptor is primarily responsible for bronchoconstriction?
The term 'miosis' refers to which action in the eye?
The term 'miosis' refers to which action in the eye?
What characteristic of acetylcholine's chemical structure affects its ability to penetrate the blood-brain barrier?
What characteristic of acetylcholine's chemical structure affects its ability to penetrate the blood-brain barrier?
What effect does hyperpolarization have in the atria of the heart?
What effect does hyperpolarization have in the atria of the heart?
Which type of receptor contributes significantly to cholinergic stimulation of salivary secretion?
Which type of receptor contributes significantly to cholinergic stimulation of salivary secretion?
Which of the following is a negative chronotropic effect of acetylcholine?
Which of the following is a negative chronotropic effect of acetylcholine?
What happens to the ventricular rate during atrial flutter/fibrillation with increased parasympathetic tone?
What happens to the ventricular rate during atrial flutter/fibrillation with increased parasympathetic tone?
What occurs when acetylcholine stimulates the cardiovascular system?
What occurs when acetylcholine stimulates the cardiovascular system?
What role does B1 adrenergic receptor have in the presence of M2 and M3 receptors regarding NE?
What role does B1 adrenergic receptor have in the presence of M2 and M3 receptors regarding NE?
What is one of the effects of acetylcholine on the respiratory tract?
What is one of the effects of acetylcholine on the respiratory tract?
Which of the following statements about muscarinic receptors is correct?
Which of the following statements about muscarinic receptors is correct?
In which of the following scenarios would acetylcholine prove to be less significant?
In which of the following scenarios would acetylcholine prove to be less significant?
What is the primary effect of muscarinic receptor antagonists like atropine?
What is the primary effect of muscarinic receptor antagonists like atropine?
Which drug is specifically noted for undergoing rapid hydrolysis in plasma?
Which drug is specifically noted for undergoing rapid hydrolysis in plasma?
What is a side effect commonly associated with muscarinic antagonists?
What is a side effect commonly associated with muscarinic antagonists?
Which of the following drugs is primarily used for its effects on the respiratory tract?
Which of the following drugs is primarily used for its effects on the respiratory tract?
What is the role of the allosteric site on the muscarinic receptor?
What is the role of the allosteric site on the muscarinic receptor?
What pharmacological effect does atropine have on rhinorrhea?
What pharmacological effect does atropine have on rhinorrhea?
Which of the following statements is true regarding ipratropium and tiotropium?
Which of the following statements is true regarding ipratropium and tiotropium?
Which compound is not classified as a quaternary ammonium compound?
Which compound is not classified as a quaternary ammonium compound?
What is a common indication for using muscarinic receptor antagonists?
What is a common indication for using muscarinic receptor antagonists?
Which of the following would likely not be a clinical reason for using atropine?
Which of the following would likely not be a clinical reason for using atropine?
Flashcards are hidden until you start studying
Study Notes
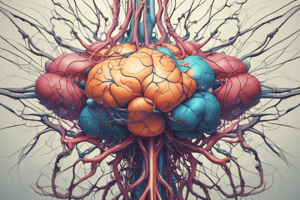
Acetylcholine & Muscarinic Receptor Target
- Acetylcholine (ACh) is a neurotransmitter that interacts with muscarinic receptors.
- Muscarinic receptors are G protein-coupled receptors (GPCRs) involved in various physiological functions.
Muscarinic Receptor Subtypes
- Muscarinic receptors are divided into five subtypes: M1, M2, M3, M4, and M5.
- M1, M3, and M5 activate Gq-PLC pathway, leading to hydrolysis of polyphosphoinositides and mobilization of intracellular Ca2+.
- M2 and M4 inhibit adenylyl cyclase and regulate specific ion channels via coupling to pertussis toxin-sensitive Gi and Go.
- M1 plays a crucial role in modulating nicotinic cholinergic transmission in the ganglia.
Pharmacological Effects of Acetylcholine
- ACh is a quaternary ammonium compound with limited penetration into the CNS due to its chemical structure.
- ACh's systemic administration is limited due to rapid hydrolysis by plasma butyrylcholinesterase (bAChE).
Cardiovascular System
- ACh exerts four primary effects on the cardiovascular system: vasodilation, decreased heart rate (negative chronotropic), decreased AV conduction velocity (negative dromotropic), and decreased force of cardiac contraction (negative inotropic).
- ACh's effects on the heart are primarily mediated by parasympathetic (vagal) stimulation.
- In the SA node, ACh slows down spontaneous depolarization, delaying the attainment of threshold potential, resulting in decreased heart rate.
- ACh's effects on contractility are mediated by inhibiting cAMP production and the release of norepinephrine (NE).
- In the atria, ACh induces hyperpolarization and decreases action potential duration by increasing IK-ACh.
- In the AV node, ACh slows down conduction and increases refractory period by inhibiting calcium channel opening (ICa-L), potentially leading to complete heart block with high doses of cholinergic agonists.
Respiratory Tract
- ACh causes bronchoconstriction, increased tracheobronchial secretions, and stimulation of chemoreceptors of the aortic and carotid bodies, primarily through M3 receptors.
Gastrointestinal Tract
- M3 receptors are primarily responsible for increased amplitude of contractions and secretory activity in the stomach and intestine, while M2 receptors also contribute.
Secretory Effects
- ACh increases secretions in lacrimal, nasopharyngeal, salivary, and sweat glands through M3 receptors.
- M1 receptors significantly contribute to the cholinergic stimulation of salivary secretion.
Eye
- ACh causes miosis (contracting pupillary sphincter muscle) and accommodation (contracting ciliary muscle for near vision), mainly mediated by M3 receptors.
Muscarinic Receptor Antagonists
- Muscarinic receptor antagonists competitively inhibit the actions of ACh and its congeners.
Atropine
- Atropine is a prototypical muscarinic antagonist.
- Atropine's pharmacological effects differ from other muscarinic antagonists.
- Atropine is used for its effects on the cardiovascular, respiratory, and gastrointestinal systems.
Cardiovascular System
- Atropine mainly alters heart rate, primarily causing tachycardia.
- Smaller doses (0.4-0.6 mg) can temporarily induce bradycardia, but this is usually followed by tachycardia.
- Atropine blocks presynaptic M1 receptors in the SA node, reducing the release of ACh and contributing to its tachycardia effect.
- Atropine blocks M2 receptors on the nodal pacemaker cells, further increasing heart rate.
- Large doses of atropine can progressively increase heart rate by blocking M2 receptors on the pacemaker cells.
- Atropine can prevent or abruptly abolish bradycardia.
- Important note:* In infants, elderly patients, and individuals with heart failure, even large doses of atropine may fail to accelerate the heart rate.
Respiratory System
- Atropine dries the mucous membranes of the respiratory tract by inhibiting secretions from the nose, mouth, pharynx, and bronchi.
- Atropine is used to reduce rhinorrhea (runny nose) and prevent irritating inhalational anesthetics (e.g., diethyl ether) from increasing bronchial secretions.
- Quaternary ammonium compounds like ipratropium, tiotropium, aclidinium, and umeclidinium are used primarily for their effects on the respiratory tract.
- Aclidinium undergoes rapid hydrolysis in plasma to inactive metabolites, reducing systemic exposure.
- Ipratropium and tiotropium have minimal inhibitory effects on mucociliary clearance compared to atropine, minimizing the accumulation of lower airway secretions.
- Key takeaway:* For COPD patients, ipratropium and tiotropium are preferred over atropine because atropine also inhibits mucociliary clearance, exacerbating their condition.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.