Podcast
Questions and Answers
What is the primary pathogenesis of Multiple Sclerosis?
What is the primary pathogenesis of Multiple Sclerosis?
- Autoimmune destruction of neurons
- Mitochondrial dysfunction and oxidative stress
- Immune-mediated inflammation and demyelination (correct)
- Viral infection of the central nervous system
Which of the following is a risk factor for developing Multiple Sclerosis?
Which of the following is a risk factor for developing Multiple Sclerosis?
- History of traumatic brain injury
- Family history of Multiple Sclerosis (correct)
- Low socioeconomic status
- Obesity
What is the typical age range for the initial symptoms of Multiple Sclerosis to appear?
What is the typical age range for the initial symptoms of Multiple Sclerosis to appear?
- 10-20 years of age
- 20-40 years of age (correct)
- 40-60 years of age
- 60-80 years of age
What is the most common type of Multiple Sclerosis?
What is the most common type of Multiple Sclerosis?
What is the primary difference between Relapsing Remitting (RRMS) and Secondary Progressive (SPMS) Multiple Sclerosis?
What is the primary difference between Relapsing Remitting (RRMS) and Secondary Progressive (SPMS) Multiple Sclerosis?
What is the characteristic feature of Primary Progressive (PPMS) Multiple Sclerosis?
What is the characteristic feature of Primary Progressive (PPMS) Multiple Sclerosis?
What percentage of people diagnosed with relapsing MS develop secondary progressive MS?
What percentage of people diagnosed with relapsing MS develop secondary progressive MS?
Which type of MS is generally associated with a better prognosis?
Which type of MS is generally associated with a better prognosis?
What is the association between high lesion load on MRI early in the disease and long-term disability?
What is the association between high lesion load on MRI early in the disease and long-term disability?
Which of the following is a cause of pseudo-relapse in MS?
Which of the following is a cause of pseudo-relapse in MS?
What is the typical presentation of optic neuritis in MS?
What is the typical presentation of optic neuritis in MS?
What is the purpose of oligoclonal IgG bands in CSF analysis?
What is the purpose of oligoclonal IgG bands in CSF analysis?
What is the goal of disease-modifying therapies in MS?
What is the goal of disease-modifying therapies in MS?
What is the approach to medication selection in MS?
What is the approach to medication selection in MS?
What is the recommendation for DMTs during pregnancy in MS?
What is the recommendation for DMTs during pregnancy in MS?
What is the effect of pregnancy on MS relapse rates?
What is the effect of pregnancy on MS relapse rates?
Which of the following signs is commonly associated with Upper Motor Neuron (UMN) lesions in patients with ALS?
Which of the following signs is commonly associated with Upper Motor Neuron (UMN) lesions in patients with ALS?
What is the primary purpose of Electromyography (EMG) in the evaluation of ALS patients?
What is the primary purpose of Electromyography (EMG) in the evaluation of ALS patients?
What is the estimated average increase in survival time associated with the use of Riluzole in ALS patients?
What is the estimated average increase in survival time associated with the use of Riluzole in ALS patients?
Which of the following criteria is used to evaluate the presence of Upper and Lower Motor Neuron signs in ALS patients?
Which of the following criteria is used to evaluate the presence of Upper and Lower Motor Neuron signs in ALS patients?
What is the primary goal of Symptomatic Therapies in the management of ALS patients?
What is the primary goal of Symptomatic Therapies in the management of ALS patients?
Which of the following is a characteristic feature of Gullain-Barré Syndrome?
Which of the following is a characteristic feature of Gullain-Barré Syndrome?
What is the primary pathophysiological mechanism of Myasthenia Gravis?
What is the primary pathophysiological mechanism of Myasthenia Gravis?
What is the most common cause of acute flaccid paralysis in healthy infants and children?
What is the most common cause of acute flaccid paralysis in healthy infants and children?
Which of the following is a characteristic feature of Amyotrophic Lateral Sclerosis (ALS)?
Which of the following is a characteristic feature of Amyotrophic Lateral Sclerosis (ALS)?
Which of the following is a potential antecedent to Gullain-Barré Syndrome?
Which of the following is a potential antecedent to Gullain-Barré Syndrome?
What is the primary goal of management in Gullain-Barré Syndrome?
What is the primary goal of management in Gullain-Barré Syndrome?
Which of the following is a characteristic feature of the M-F variant of Gullain-Barré Syndrome?
Which of the following is a characteristic feature of the M-F variant of Gullain-Barré Syndrome?
What is the prognosis for most patients with Myasthenia Gravis?
What is the prognosis for most patients with Myasthenia Gravis?
What is the primary difference between the Ocular and Generalized types of Myasthenia Gravis?
What is the primary difference between the Ocular and Generalized types of Myasthenia Gravis?
What is the average onset age for Amyotrophic Lateral Sclerosis (ALS)?
What is the average onset age for Amyotrophic Lateral Sclerosis (ALS)?
Flashcards are hidden until you start studying
Study Notes
Multiple Sclerosis (MS)
Burden on Patients with MS (PwMS)
- Wide range of symptoms, including loss of vision, ataxia, tremor, bowel incontinence, urinary incontinence, generalized pain, fatigue, memory and learning problems, depression, and anxiety
- Initial symptoms often appear between 20 and 40 years of age
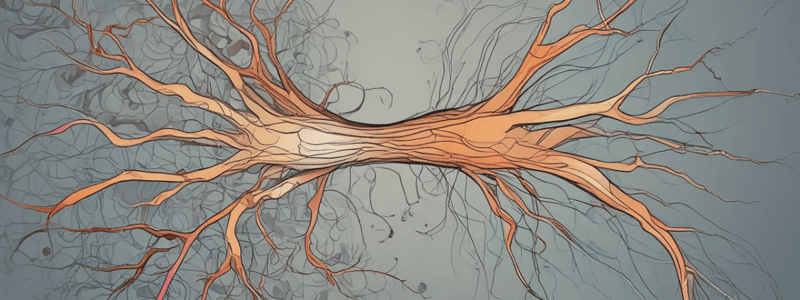
Pathophysiology
- Etiology: Unknown
- Pathogenesis: Central Nervous System (CNS) immune-mediated inflammation and demyelination, along with axonal degeneration
Risk Factors
- Genetic: Family History, Specific Genes (HLA-DRB1), Caucasian, Female
- Environmental: Ambient UV Radiation, Dietary (Vitamin D), Infectious (EBV), Tobacco Use
Types of MS
- Relapsing (RRMS)
- Most common type
- Characterized by relapses (symptoms getting worse) followed by recovery (remission)
- Disability doesn't worsen between relapses, but can worsen after each relapse
- Secondary Progressive (SPMS)
- Have increasing disability, but no relapses
- Typically occurs 15-20 years after diagnosis
- Primary Progressive (PPMS)
- Neurologic functions worsen steadily from the beginning
- No symptom flare-ups (relapses) and no recovery (remission)
Prognosis
- Relapsing course is generally associated with a better prognosis than a progressive course
- High lesion load on MRI early in the disease is associated with greater long-term disability
- Psychosocial stress has been linked to an increased risk of relapse and pseudo-relapse
Clinical Features
- History: Single episode or multiple episodes of neurological impairment, separated by a period of time with less or no symptoms
- Neurocognitive: Cognitive impairment
- Motor - Somatic: Spasticity, Weakness, Tremor
- Motor - Autonomic: Sexual Dysfunction, Overactive Bladder, Underactive Bladder
- Sensory: Visual Impairment, Trigeminal Neuralgia, Sensory Disturbance
- Other: Fatigue, Seizure, Lhermitte's Sign, Uhthoff Phenomenon
Relapse, Remission, & Pseudo-Relapse
- Pseudo-Relapse: Caused by infectious, metabolic, physiologic stress, or psychosocial stress
- Relapse: Characterized by new symptoms or worsening of existing symptoms
- Remission: Symptom improvement or recovery
Optic Neuritis
- One of the initial MS events
- Pathogenesis: Inflammatory demyelination of the optic nerve
- Clinical Features: Painful, monocular visual loss, often with papillitis
- Long-term: Relative afferent pupillary defect, color desaturation, optic atrophy
- Diagnostic Studies: Ophthalmologic examination, MRI brain and optic nerves
- Management: High dose steroids
- Prognosis: MS presenting symptom in 15-20% of patients, often with complete visual improvement
Transverse Myelitis
- General: Idiopathic, often post-infectious
- Secondary to multiple sclerosis, neuromyelitis optica, and acute disseminated encephalomyelitis
- Pathogenesis: Inflammatory demyelination of the spinal cord
- Clinical Features: Rapid onset, weakness, sensory alterations, and bowel/bladder dysfunction
- Diagnostic Studies: MRI brain and spine, CSF for markers of secondary causes
- Management: High dose steroids
- Prognosis: MS presenting symptom in 5-10% of patients, often with partial recovery
Diagnostic Studies
- Magnetic Resonance Imaging (MRI): MS most commonly involves cerebral hemispheres, periventricular regions
- Cerebrospinal Fluid Analysis:
- Description: Clear, Colorless
- Cell Count: Usually < 5/mm3, Rarely > 50/mm3
- Protein: Normal or slightly elevated (rarely > 100/dL)
- Glucose: Normal
- IgG Index: Elevated
- Oligoclonal IgG Bands >4
- Optic Coherence Testing: Measures retinal nerve thickness, used in patient with recurrent optic neuritis and normal MRI, or differentiating NMSOD from MS
Management
- Relapsing:
- Acute Inflammation: High dose corticosteroids
- Disease-Modifying Therapy: Immunomodulation or immunosuppression
- Associated Neurological Symptoms: Treatments vary
- Progressive:
- Acute Inflammation: High dose corticosteroids
- Disease-Modifying Therapy: Immunomodulation or immunosuppression
- Associated Neurological Symptoms: Treatments vary
- No cure, but the disease is manageable with lifelong treatment
- Continuous decision-making process for treatment, considering patient preferences, efficacy, safety profile, side effects, route of administration, and cost
Gullain-Barré Syndrome
- Most common cause of acute flaccid paralysis in healthy infants and children
- Neuromuscular emergency
- Pathophysiology: immune-mediated demyelination or axon injury leading to dysfunction of peripheral nerves
- Potential antecedents: infection, immunization, surgery, trauma, bone marrow transplant, and systemic disorders
- Clinical features: 4 phases, progressive, mostly symmetric, motor > sensory impairment, distal to proximal
- Evaluation: Brighton criteria, NCS, CSF, MRI neuroaxis, and M-F variant
- Management: inpatient, plasmapheresis, intravenous immunoglobulin, mechanical ventilation assistance
- Prognosis: most experience continued progression for up to two weeks, followed by a plateau phase, and then gradual recovery
Myasthenia Gravis
- Bimodal onset: 30 and 50
- Pathophysiology: autoimmune destruction of acetylcholine receptors on the surface of skeletal muscles
- Clinical features: insidious onset, fluctuating, muscle weakness, fatigability, axial and limb muscles, cranial nerves, and respiration
- Symptoms improve with rest
- Ocular type: ptosis, EOM weakness
- Lambert-Eaton type: proximal weakness, can be associated with cancer
- Evaluation: antibody testing, serum AChR antibodies, ice pack test, and CT or MRI of chest for thymoma
- Management: cholinesterase inhibition, pyridostigmine, immunotherapy, prednisone, and IVIG or plasmapheresis
- Prognosis: maximal extent at 3 years in majority of patients, course may be progressive or relapsing-remitting
Amyotrophic Lateral Sclerosis (ALS)
- Average onset: 56-63 years
- Pathophysiology: neurodegenerative, protein accumulation, oxidative stress, inflammation, death of upper and lower motor neurons
- Genetic factors, including mutations, sporadic (90%)
- Clinical features: upper limb, lower limb, bulbar, cognitive changes, no sensory symptoms, upper motor neuron and lower motor neuron findings
- Upper motor neuron findings: increased muscle tone, spasticity, hyperactive deep tendon reflexes, pathologic reflexes
- Lower motor neuron findings: decreased muscle tone, muscle atrophy, fasciculations, reduced or absent deep tendon reflexes
- Pseudobulbar affect: episodic, sudden uncontrollable and inappropriate laughing or crying
- Evaluation: upper and lower motor neuron signs in 3 regions, electromyography, denervation, genetic testing
- Management: goals of care, slow disease progression, maintain function, safety, comfort, two types of therapies (disease modifying and symptomatic)
- Disease modifying therapies: riluzole, oral therapy, prolongs survival by an average of 2 months, may improve quality of life
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.