Podcast
Questions and Answers
Which of the following pain patterns is MOST indicative of cancer in the musculoskeletal system?
Which of the following pain patterns is MOST indicative of cancer in the musculoskeletal system?
- Pain that is proportionate to mechanical findings
- Constant, progressive pain not relieved by rest (correct)
- Pain that is relieved by changes in position
- Pain that decreases with rest
A patient presents with a painful arc between 70-120 degrees abduction, positive Hawkins-Kennedy and Neer's tests, and pain with internal rotation and overhead reaching. What condition is MOST likely?
A patient presents with a painful arc between 70-120 degrees abduction, positive Hawkins-Kennedy and Neer's tests, and pain with internal rotation and overhead reaching. What condition is MOST likely?
- Impingement Syndrome (correct)
- Adhesive Capsulitis
- Rotator Cuff Tear
- Shoulder Labral Tear (SLAP)
A patient over 50 years old reports a gradual onset of stiffness and pain in the shoulder, made worse with movement and a progressive loss of function, particularly when reaching overhead or behind the back. Which condition is MOST consistent with this presentation?
A patient over 50 years old reports a gradual onset of stiffness and pain in the shoulder, made worse with movement and a progressive loss of function, particularly when reaching overhead or behind the back. Which condition is MOST consistent with this presentation?
- Osteoarthritis (OA) (correct)
- Rotator Cuff Tear
- Shoulder Labral Tear (SLAP)
- Adhesive Capsulitis
Which assessment tool is BEST suited to assess the psychosocial risk factors that may contribute to chronic pain disability in a patient?
Which assessment tool is BEST suited to assess the psychosocial risk factors that may contribute to chronic pain disability in a patient?
A patient with musculoskeletal pain also reports fever, excessive sweating, and nausea. These findings are MOST indicative of:
A patient with musculoskeletal pain also reports fever, excessive sweating, and nausea. These findings are MOST indicative of:
Loss of smell (anosmia) can result from damage to which cranial nerve?
Loss of smell (anosmia) can result from damage to which cranial nerve?
A patient presents with vertical diplopia that worsens when looking down, such as when reading on stairs. Which cranial nerve is MOST likely affected?
A patient presents with vertical diplopia that worsens when looking down, such as when reading on stairs. Which cranial nerve is MOST likely affected?
The Babinski test assesses for lesions affecting which area?
The Babinski test assesses for lesions affecting which area?
Which statement BEST describes the PRIMARY mechanism of action of Myasthenia Gravis?
Which statement BEST describes the PRIMARY mechanism of action of Myasthenia Gravis?
A patient presents with tremor, rigidity, and bradykinesia. Which of the following conditions is MOST likely?
A patient presents with tremor, rigidity, and bradykinesia. Which of the following conditions is MOST likely?
Which of the following is a common EARLY symptom reported by individuals with Multiple Sclerosis (MS)?
Which of the following is a common EARLY symptom reported by individuals with Multiple Sclerosis (MS)?
What is the PRIMARY mechanism by which antidepressants alleviate symptoms of depression and mood disorders?
What is the PRIMARY mechanism by which antidepressants alleviate symptoms of depression and mood disorders?
Which category of antidepressants is MOST likely to cause significant sedation, potentially impairing patient adherence to therapy?
Which category of antidepressants is MOST likely to cause significant sedation, potentially impairing patient adherence to therapy?
A patient taking MAO inhibitors needs to be cautious of foods that affect catecholamine levels due to the risk of a hypertensive crisis. Which of the following foods should they AVOID?
A patient taking MAO inhibitors needs to be cautious of foods that affect catecholamine levels due to the risk of a hypertensive crisis. Which of the following foods should they AVOID?
Which of the following is a common adverse effect of benzodiazepines, especially relevant to consider in older adults?
Which of the following is a common adverse effect of benzodiazepines, especially relevant to consider in older adults?
Which of the following adverse effects is MOST associated with long-term use of sedative-hypnotics like benzodiazepines?
Which of the following adverse effects is MOST associated with long-term use of sedative-hypnotics like benzodiazepines?
A patient is prescribed warfarin for long-term management of atrial fibrillation. What PRIMARY adverse side effect requires diligent monitoring?
A patient is prescribed warfarin for long-term management of atrial fibrillation. What PRIMARY adverse side effect requires diligent monitoring?
Tardive dyskinesia, characterized by repetitive, involuntary movements, is a potential irreversible side effect associated with which class of medications?
Tardive dyskinesia, characterized by repetitive, involuntary movements, is a potential irreversible side effect associated with which class of medications?
A patient taking levodopa for Parkinson's disease experiences end-of-dose akinesia. Which of the following BEST describes this phenomenon?
A patient taking levodopa for Parkinson's disease experiences end-of-dose akinesia. Which of the following BEST describes this phenomenon?
Which medication is used to treat severe spasticity regardless of the location or the pathology causing the spasticity, by acting directly on skeletal muscle cells?
Which medication is used to treat severe spasticity regardless of the location or the pathology causing the spasticity, by acting directly on skeletal muscle cells?
During a patient interview, which of the following elements is MOST crucial during the 'Subjective Examination' phase?
During a patient interview, which of the following elements is MOST crucial during the 'Subjective Examination' phase?
Which component of a patient interview is MOST associated with identifying potential barriers to recovery?
Which component of a patient interview is MOST associated with identifying potential barriers to recovery?
In the context of minor traumatic brain injury (mTBI), what is the MOST important consideration regarding the risk of re-injury?
In the context of minor traumatic brain injury (mTBI), what is the MOST important consideration regarding the risk of re-injury?
Which of the following is MOST characteristic of an 'open head injury'?
Which of the following is MOST characteristic of an 'open head injury'?
Caffeine's primary effect on the body is BEST described as:
Caffeine's primary effect on the body is BEST described as:
Flashcards
MSK Cancer Pain Pattern
MSK Cancer Pain Pattern
Constant, progressive pain, not relieved by rest or position changes, especially at night.
Impingement Syndrome
Impingement Syndrome
Painful arc between 70-120° abduction; positive Hawkins-Kennedy & Neer's tests.
Rotator Cuff Tear
Rotator Cuff Tear
Painful arc (60-120° abduction); weakness, positive Empty Can, Drop Arm tests.
Adhesive Capsulitis
Adhesive Capsulitis
Signup and view all the flashcards
Osteoarthritis (OA) of Shoulder
Osteoarthritis (OA) of Shoulder
Signup and view all the flashcards
Shoulder Labral Tear (SLAP)
Shoulder Labral Tear (SLAP)
Signup and view all the flashcards
Tendinopathy (Shoulder)
Tendinopathy (Shoulder)
Signup and view all the flashcards
Bursitis (Shoulder)
Bursitis (Shoulder)
Signup and view all the flashcards
Hip Fracture
Hip Fracture
Signup and view all the flashcards
Osteoarthritis (OA) of Hip
Osteoarthritis (OA) of Hip
Signup and view all the flashcards
Rheumatoid Arthritis (RA) of Hip
Rheumatoid Arthritis (RA) of Hip
Signup and view all the flashcards
Hip Bursitis
Hip Bursitis
Signup and view all the flashcards
Hip Impingement (FAI)
Hip Impingement (FAI)
Signup and view all the flashcards
Hip Dislocation
Hip Dislocation
Signup and view all the flashcards
Pain Catastrophizing Scale
Pain Catastrophizing Scale
Signup and view all the flashcards
Oswestry Disability Questionnaire (ODI)
Oswestry Disability Questionnaire (ODI)
Signup and view all the flashcards
SCOFF Questionnaire
SCOFF Questionnaire
Signup and view all the flashcards
McGill Pain Scale
McGill Pain Scale
Signup and view all the flashcards
OMPSQ-10
OMPSQ-10
Signup and view all the flashcards
OSPRO-YF
OSPRO-YF
Signup and view all the flashcards
Anxiety Disorder
Anxiety Disorder
Signup and view all the flashcards
Panic Disorder
Panic Disorder
Signup and view all the flashcards
CN III (Oculomotor nerve) function
CN III (Oculomotor nerve) function
Signup and view all the flashcards
Test for Clonus
Test for Clonus
Signup and view all the flashcards
Babinski Test
Babinski Test
Signup and view all the flashcards
Study Notes
- "disorder of" is abbreviated as d/o and also known as "______ disorder".
Pain Patterns for Cancer in the MSK System
- Constant, progressive pain is not relieved by rest or changes in position.
- Night pain worsens despite repositioning; this is a red flag for malignancy.
- Pain is disproportionate to mechanical findings, without a known mechanism of injury (MOI) but with severe pain.
- Unexplained weight loss, fatigue, or history of cancer may accompany MSK pain.
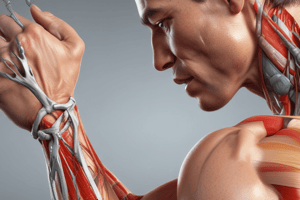
Common Hip and Shoulder Pathologies
Shoulder - Impingement Syndrome
- Painful arc occurs during 70-120° abduction.
- Hawkins-Kennedy and Neer's tests are positive.
- Pain is present with internal rotation and overhead reaching.
Shoulder - Rotator Cuff Tears
- A painful arc occurs during 60-120° abduction.
- Weakness with difficulty lifting objects is present.
- Empty Can, Drop Arm, and Infraspinatus tests are positive.
- A complete tear causes significant weakness, making it difficult to lift the arm.
Shoulder - Adhesive Capsulitis
- Range of motion (ROM) is severely limited in all directions, especially external rotation (ER) and abduction (ABD).
- Pain occurs at rest and at night.
Shoulder - Osteoarthritis (OA)
- Typically affects adults > 50 years.
- Gradual onset of stiffness and pain occurs.
- Pain is present with movement, especially ER and ABD.
- Progressive loss of function causes difficulty reaching overhead or behind the back.
Shoulder - Shoulder Labral Tear (SLAP)
- Pain occurs with overhead activity.
- Possible shoulder instability is present.
Shoulder - Tendinopathy (overuse)
- Pain is present with overhead activities, reaching behind the back.
- Tenderness occurs over rotator cuff tendons (especially supraspinatus).
- Weakness is present with resisted movements like the Empty Can and Infraspinatus tests.
- Painful arc occurs between 60°-120° abduction.
Shoulder - Bursitis
- Pain is present at rest and with movement, especially abduction.
- Tenderness is present over the subacromial space.
- A painful arc is present.
- Bursitis may coexist with rotator cuff tendinopathy.
Shoulder - Fracture
- Severe pain, swelling, and bruising occur.
- Deformity is present if the fracture is displaced.
- The range of motion (ROM) is limited due to pain.
Hip - Osteoarthritis (OA)
- Typically affects adults > 50 years.
- Pain occurs with weight-bearing.
- Morning stiffness lasts <30 minutes and worsens with activity, relieved by rest.
- Progressive loss of ROM occurs, especially internal rotation and flexion.
- Antalgic gait and possible Trendelenburg sign occur due to weak abductors.
Hip - Rheumatoid Arthritis (RA)
- Typically has onset in adults aged 30-60 years.
- Pain occurs with weight-bearing.
- Morning stiffness lasts >1 hour and improves with movement.
Hip - Hip Bursitis (Greater Trochanteric Pain Syndrome)
- More common in women than men.
- Lateral hip pain occurs.
- Pain worsens with lying on the affected side, walking, stairs, and prolonged standing.
- Tenderness is present over the greater trochanter.
- Pain is present with resisted abduction.
Hip - Hip Impingement (Femoroacetabular Impingement "FIA")
- Typically affects young active adults.
- Groin pain occurs with flexion and internal rotation limitations.
- Pain is present with hip flexion, internal rotation, and prolonged sitting.
- The C-sign (hand cupping hip to describe deep pain) is present.
- The FADIR test (hip flexion, adduction, internal rotation reproduces pain) is positive.
Hip - Hip Dysplasia
- More common in females and is a congenital condition.
- A shallow acetabulum leads to hip instability.
- Frequent subluxations or dislocations occur.
- Clicking or catching sensation occurs in the hip.
- Worsening pain occurs with weight-bearing and activity.
- The FABER and log roll tests are positive.
Hip - Hip Dislocation (trauma related)
- Severe pain is present.
- Inability to bear weight occurs.
- The leg appears shortened and rotated: posterior dislocation results in internal rotation, while anterior dislocation results in external rotation.
Pain Scale Measures
- Pain Catastrophizing Scale: assesses negative cognitive-affective responses to pain (rumination, magnification, helplessness) in chronic pain patients, predicting disability and guiding psychological interventions.
- Oswestry Disability Questionnaire (ODI): measures low back pain symptoms, severity, and impact on functional activities, assessing disability in lumbar spine patients and tracking progress in physical therapy.
- SCOFF Questionnaire: detects eating disorders by raising suspicion in patients with sudden weight loss, excessive dieting, or disordered eating signs.
- McGill Pain Scale: assesses qualitative and quantitative aspects of pain (sensory, affective, evaluative) in chronic pain syndromes, differentiating between nociceptive and neuropathic pain and monitoring pain over time..
- OMPSQ-10 (Örebro Musculoskeletal Pain Screening Questionnaire): screens for psychosocial risk factors contributing to chronic pain disability, identifies high-risk acute musculoskeletal pain patients, and guides intervention planning.
- OSPRO-YF (Optimal Screening for Prediction of Referral and Outcome - Yellow Flag tool): assesses psychosocial factors ("yellow flags") influencing pain recovery in musculoskeletal pain conditions, guiding multidisciplinary interventions for psychological or behavioral health support.
Constitutional Signs and Symptoms
- Not MSK-related, indicating a systemic issue.
- Include fever, diaphoresis (excessive sweating), sweats, nausea, vomiting, diarrhea, pallor, dizziness/syncope, fatigue/weakness, and weight loss.
Mental/Personality Disorders
Anxiety d/o
- Generalized emotional state of fear and apprehension is associated with heightened physiologic arousal (elevated heart rate, sweat gland activity).
- Anxiety can amplify pain perception.
Panic d/o
- Sudden, unprovoked, intense anxiety with physical symptoms lasts a few minutes to less than 2 hours.
- Marked dyspnea, tachycardia or palpitations, headaches, dizziness, paresthesia, choking or smothering feelings, nausea, bloating, feelings of fear and panic are associated with it.
- Recurrent sleep panic attacks (not nightmares) occur in about 30% of individuals.
Depression
- Morbid sadness, dejection, or melancholy distinguishes it from grief (normal response to loss).
Bipolar d/o
- Cyclical mood swings include mania (high energy, elevated mood, decreased sleep) and depression.
- Type I involves severe manic episodes.
- Type II is characterized by distinct periods of depression.
Obsessive-compulsive d/o
- Involves obsessions and repetitive compulsions.
- Major depression is common in half of OCD cases.
Delusional d/o
- Delusions of potential harm without bizarre behaviors.
Schizophrenia d/o
- Distorted thinking, reactions, and perceptions of reality.
Brief psychotic d/o
- Related to life stressors and short duration.
Schizo-affective d/o
- Combines both a mood disorder and schizophrenia and is chronic.
Borderline personality d/o
- Pervasive instability of identity, interpersonal relationships, and mood.
- People with BPD have stormy and unpredictable ways of relating, affecting more women than men.
Passive-aggressive personality d/o
- (Renamed Negativistic Personality Disorder).
- Involves passive resistance to social expectations and demands.
Cranial Nerves
- CN I (Olfactory): Smell (sensory); damage leads to loss of smell (anosmia), usually unilateral.
- CN II (Optic): Vision (sensory); damage leads to vision loss (blindness, visual field defects), afferent pupillary defect.
- CN III (Oculomotor): Eye movement (SR, IR, MR, IO), pupillary constriction, eyelid elevation; damage leads to ptosis (drooping eyelid), dilated pupil (mydriasis), eye down & out, diplopia.
- CN IV (Trochlear): Eye movement (SO – down & in); damage leads to vertical diplopia (worse with downward gaze), head tilt to compensate.
- CN V (Trigeminal): Sensation to face (V1, V2, V3), muscles of mastication; damage leads to loss of facial sensation, weak jaw movement, jaw deviates to affected side.
- CN VI (Abducens): Eye movement (LR – lateral gaze); damage leads to inability to abduct eye, diplopia.
- CN VII (Facial): Facial expression, taste (anterior 2/3 tongue), salivation, lacrimation; damage leads to facial droop, loss of taste (anterior 2/3), hyperacusis.
- CN VIII (Vestibulocochlear): Hearing & balance; damage leads to hearing loss, vertigo, nystagmus, balance issues.
- CN IX (Glossopharyngeal): Taste (posterior 1/3 tongue), pharyngeal sensation, swallowing; damage leads to loss of gag reflex, dysphagia, impaired taste (posterior 1/3).
- CN X (Vagus): Swallowing, phonation, parasympathetic function; damage leads to hoarseness, uvula deviates away from lesion, dysphagia.
- CN XI (Spinal Accessory): Sternocleidomastoid & trapezius movement; damage leads to weak shoulder shrug, difficulty turning head.
- CN XII (Hypoglossal): Tongue movement; damage leads to tongue deviates toward lesion, dysarthria.
Neurological Tests
- Test for Clonus: Assesses for upper motor neuron (UMN) dysfunction by quickly dorsiflexing the ankle or extending the wrist and holding it; a positive test shows rhythmic, involuntary, sustained muscle contractions (>3-5 beats indicate pathology).
- Babinski Test: Evaluates UMN lesion affecting the corticospinal tract by stroking the sole of the foot from heel to toes; a positive test shows toe extension (big toe dorsiflexion) and fanning of toes (normal in infants 0-24 months, abnormal in adults).
- Rinne Test: Differentiates conductive vs. sensorineural hearing loss by striking a tuning fork, placing it firmly on the mastoid process until sound stops, then moving vibrating tines near the ear canal; normal is air conduction (AC) > bone conduction (BC), conductive hearing loss is BC > AC (suggests middle ear pathology), and sensorineural hearing loss shows AC > BC but both are reduced in perception.
- Weber Test: Identifies unilateral hearing loss by striking a tuning fork and pressing the stem firmly on the top center of the patient's head; normal sound heard equally in both ears, conductive hearing loss lateralizes to the affected ear, and sensorineural hearing loss lateralizes to the unaffected ear.
- Romberg Test: Assesses proprioception and balance. Patients stand with feet together, arms at sides, eyes open for 20-30 seconds, then eyes closed for 20-30 seconds; a positive test shows increased sway or loss of balance with eyes closed.
- Deep Tendon Reflexes (DTR): Assess reflex arc integrity and UMN/LMN function. Key reflexes include Biceps (C5-C6), Brachioradialis (C6), Triceps (C7), Patellar (L3-L4), and Achilles (S1-S2); Hyperreflexia indicates UMN lesion, and Hyporeflexia indicates LMN lesion.
- Rapid Hand/Foot Movements: Assess cerebellar function (coordination, motor planning) by rapidly alternating supination/pronation (hands) or rapid tapping on the ground (feet); a positive test is Dysdiadochokinesia (inability to perform smooth, rhythmic movements).
Neurodegenerative Diseases
Alzheimer's Disease
- Breakdown of brain cell processes, amyloid accumulation, high amyloid plaque, disruptions in neurotransmitters with cholinergic abnormalities. Presentation includes loss of older memories, social difficulty, mood swings, sleep/eating/sexual disorders, delusions, agitation, violence, loss of smell/taste, decreased appetite, incontinence.
- 40-60% of individuals with late-onset AD experience psychotic symptoms like hallucinations, delusions, and dramatic verbal, emotional or physical outbursts.
Parkinson's Disease
- Degeneration of dopamine-producing cells in basal ganglia (idiopathic or genetic link). Presentation: tremor, rigidity, akinesia/bradykinesia, slowed lip/tongue movements, impoverished movement, stooped posture, narrow base of support, short shuffling steps, lessened arm swing, difficulty initiating walking/turning, slowness of gait ("freezing" or "festinating gait").
Parkinsonism (Umbrella term)
- From drug-induced Parkinsonism blocking dopamine metabolism. Presentation: includes Parkinson's and bilateral onset of bradykinesia; symptoms resolve when drugs are discontinued.
Multiple Sclerosis (MS)
- Autoimmune, demyelinating disorder with plaques in CNS. Types include Primary Progressive (steady progression), Progressive Relapsing (worsening with relapses), Relapse Remitting (relapses with remissions; 80-85% of individuals), and Secondary Progressive (progressive worsening). Presentation: sensory changes, paresthesia/dysesthesia, motor loss, ataxia, vision loss, speech/swallowing difficulties, sensory disturbances, autonomic/cognitive dysfunction, mood disturbances, visual blurring, diplopia, weakness, balance problems, fatigue (mid-afternoon), and motor weakness. Spasticity (90% of MS), spasms/weakness of facial muscles, dysarthria, dysphagia, pain (50%), depression, and cognitive decline (50%) are some signs.
Myasthenia Gravis
- Autoimmune disorder affecting the neuromuscular junction, blocking acetylcholine receptors. Presentation: muscle weakness (especially extremities), diplopia, speech/chewing difficulties.
Amyotrophic Lateral Sclerosis (ALS)
- Unknown cause involving motor neuron degeneration/scarring, UMN and LMN lesions, lateral and sclerosis terms identify the disease. Presentation: Tonic Atrophy, Pseudobulbar Palsy (corticobulbar tract damage), and Progressive Bulbar Palsy (cranial nerve nuclei involvement, swallowing/chewing/facial weakness).
Components of Patient Interviews
- Components include demographics, occupation/role in society, social history, MOI, history of current condition, date of onset, chief complaint/current symptom Description, 24-Hour Symptom Pattern, stated functional impairments, current medications, diagnostic testing, prior treatments, prior level of function (PLOF)/activity level, past medical history (PMH)/past surgical history, yellow flags/psychosocial remarks, contextual factors, and stated goals.
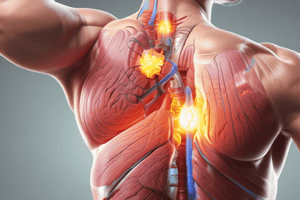
Indications and Side Effects of Drugs
Antidepressants
- Indications: alleviate symptoms of depression and mood disorders (GAD, panic disorder, OCD, PTSD), effective for chronic pain syndromes (neuropathic pain, fibromyalgia, chronic low back pain). - SSRIs generally well-tolerated with low risk of cardiovascular and anticholinergic effects. - TCAs cause sedation, potentially impair patient adherence, and strong anticholinergic properties can cause confusion, delirium, dry mouth, constipation, urinary retention, and tachycardia. - MAO Inhibitors often lead to CNS excitation (restlessness, irritability, agitation, sleep loss) and hypertension crisis.
Opioids
- Indications: effective for moderate-to-severe, constant pain, surgery, trauma, myocardial infarction, and cancer, general anesthesia (short-term), cough suppression, diarrhea control, alleviate panic/anxiety (shortness of breath in pulmonary edema). Side effects: sedation, mental slowing, drowsiness, fall risk, euphoria, respiratory depression, orthostatic hypotension, nausea/vomiting, severe constipation, tolerance, dependence, overdose, and death.
Benzodiazepines
- Indications: treat acute anxiety, offer anticonvulsant properties, skeletal muscle relaxation
- Side effects include psychomotor impairment and drowsiness
Anticoagulant drugs
- Heparin, warfarin, direct thrombin inhibitors, factor Xa inhibitors. Heparin comes in Unfractionated Heparin (UFH) and Low-Molecular-Weight Heparin (LMWH) forms. Indications: treat venous thrombosis (DVT)/thromboembolism (PE), prophylactically for high-risk individuals (surgical procedures, joint replacement, heart valve replacement, inactive periods), reduce stroke risk in atrial fibrillation, prevent recurrent ischemic stroke, CAD (PCI, or stent placement), and acute myocardial infarction.
- Adverse Effects: Heparin-induced Thrombocytopenia (HIT), bleeding risk (bruising, GI bleeding, intracranial hemorrhage), and monitor long-term warfarin therapy with prothrombin time and INR to ensure clotting ability.
Antiplatelet drugs
- Aspirin, Adenosine Diphosphate (ADP) Receptor Blockers, Glycoprotein Ilb-Illa Receptor Blockers.
- Indications: prevent arterial clots (coronary artery occlusion, MI, cerebral infarction, ischemic stroke, TIA).
- Adverse Effects: increased bleeding risk, alerting for any unexplained or heavy bleeding or hemorrhage symptoms (sudden joint/back pain or headaches), unusual gum bleeding, frequent nosebleeds, heavier menstrual bleeding, and bruises.
- Aspirin can cause gastric irritation or ulcers and renal and liver toxicity at high doses.
Antipsychotic drugs
- Treat schizophrenia (e.g., Haloperidol and Abilify); adverse effects include abnormal movement patterns, tardive dyskinesia, and other extrapyramidal tract symptoms that may be irreversible.
Levodopa
- Used with Carbidopa for Parkinson's disease treatment; adverse side effects include nausea/vomiting, arrhythmias, orthostatic hypotension, psychotic symptoms, depression, anxiety, confusion, impulsiveness, dyskinesias, diminished response and fluctuations in response, and end-of-dose akinesia, on-off phenomenon.
Sedative hypnotics
- Treat sleep issues and anxiety. Benzodiazepines potentiate GABA inhibitory effects in CNS; Nonbenzodiazepines potentiate GABA at low doses and global inhibition at high doses. - Adverse Effects: anterograde amnesia, dizziness, confusion, and prone to tolerance and dependence.
Cholinergics
- Treat Myasthenia Gravis, Alzheimer's Disease, Glaucoma, Postoperative GI, and Urinary Atony. Adverse effects mimic exaggerated parasympathetic activity, GI distress (nausea, vomiting, diarrhea, abdominal cramping), increased salivation, bronchoconstriction, bradycardia, and difficulty in visual accommodation.
Types and Indications for Anticoagulant and Antiplatelet Meds
- Anticoagulants: Heparin, Warfarin, Direct Thrombin Inhibitors, Factor Xa Inhibitors. Antiplatelet Drugs: Aspirin, ADP Receptor Blockers, Glycoprotein IIb/IIIa Receptor Blockers, Others. Why: History of stroke, heart attack, or blood clots (DVT/PE), atrial fibrillation (stroke prevention), mechanical heart valve (Warfarin), post-surgery (hip/knee replacements), coronary stents, and peripheral artery disease.
Classes of Opioids
- Strong (full/pure) Agonists: severe pain (Morphine, Fentanyl, Hydromorphone, etc.)
- Mild-to-Moderate (partial) Agonists: moderate pain (Codeine, Hydrocodone, Oxycodone, Propoxyphene)
- Mixed Agonists-Antagonists: analgesia with less respiratory depression (Nalbuphine, Pentazocine, Buprenorphine)
- Antagonists: reverse opioid overdose and treat opioid use disorder (Naloxone/Naltrexone).
Caffeine and Alcohol on the Body Effects
Caffeine
- CNS stimulant, appears to keep people from slowing down
- Binds with receptors that normally receive adenosine, overriding the switch that turns it down -High consumption or withdrawal from caffeinated items can cause headaches, fatigue, joint pain, and irritability
Alcohol
- Can mimic or exacerbate cognitive change linked w/ normal aging and Alzheimer's disease
- Reduces restful sleep
-Virtual elimination of restful sleep
- Heavy drinking linked with increasing risk of cancer
Types of TBI
Traumatic Brain Injury (TBI)
- negative affect on brain that results from external force.
mTBI (Minor Traumatic Brain Injury)
- Concussion, relatively short time, or no loss of consciousness.
- Distractibility, headache, memory, fatigue, personality changes, and decreased control of emotions.
- Protocols, for re-injury post the injury-return to School, etc.
Medical Types
- Open Head: injury to the breached mininges due to brain exposure.
- Closed Head:injury to the breach inside mininges but the are left in tact.
- Peneatrating Injury: vessels vascular damage, etc.
Muscle Relaxants
Baclofen
- Centrally acting, Stimulates GABA-B receptor pathways Orally and intrathecally for chronic and severe body spasticity Indication: Cerebrovascular accidents S/E- Drowsiness, dizziness etc Abruptly: w/ Fever, Confusion Delerium
Botox
- Administered: Via shots Indication: Spasticity S/E :
- Acts directly on skeletal muscle cells
- Binds to Ryanodine Type-1 receptor and prevents calcium release-reducing muscle contraction
- Generalized muscle weakness: Severe hepatoxocity
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.