Podcast
Questions and Answers
What is the primary digestive function of the liver?
What is the primary digestive function of the liver?
- Metabolism of carbohydrates
- Filtration of blood
- Production of bile (correct)
- Storage of vitamins
Which component is NOT found in bile?
Which component is NOT found in bile?
- Bile salts
- Cholesterol
- Amino acids (correct)
- Bile pigments
What role do bile salts play in digestion?
What role do bile salts play in digestion?
- Neutralize stomach acid
- Break down carbohydrates
- Store vitamins
- Emulsify fats (correct)
Where is bile stored before its release into the digestive system?
Where is bile stored before its release into the digestive system?
What is the nature of bile in terms of pH?
What is the nature of bile in terms of pH?
Which structure primarily facilitates the process of neutralizing acidity in the duodenum?
Which structure primarily facilitates the process of neutralizing acidity in the duodenum?
What triggers the release of pancreatic enzymes in the duodenum?
What triggers the release of pancreatic enzymes in the duodenum?
What are the three main subdivisions of the small intestine?
What are the three main subdivisions of the small intestine?
What is the length of the duodenum?
What is the length of the duodenum?
Which of the following secretions is stimulated by the arrival of acidic chyme in the duodenum?
Which of the following secretions is stimulated by the arrival of acidic chyme in the duodenum?
What process occurs inside the epithelial cells after the formation of monoglycerides and free fatty acids?
What process occurs inside the epithelial cells after the formation of monoglycerides and free fatty acids?
What is formed when triglycerides aggregate and are coated with lipoprotein?
What is formed when triglycerides aggregate and are coated with lipoprotein?
How do chylomicrons exit the epithelial cells?
How do chylomicrons exit the epithelial cells?
What prevents chylomicrons from crossing the basement membrane of capillaries?
What prevents chylomicrons from crossing the basement membrane of capillaries?
What is the primary role of the large intestine?
What is the primary role of the large intestine?
Which vitamins does the large intestine primarily absorb?
Which vitamins does the large intestine primarily absorb?
What role do beneficial bacteria in the large intestine play?
What role do beneficial bacteria in the large intestine play?
What components make up the structure of the large intestine?
What components make up the structure of the large intestine?
What type of cells in the pancreas are responsible for secreting insulin?
What type of cells in the pancreas are responsible for secreting insulin?
Which of the following is NOT a secretion produced by the acinar cells of the pancreas?
Which of the following is NOT a secretion produced by the acinar cells of the pancreas?
Which of the following hormones is secreted by the alpha cells of the pancreas?
Which of the following hormones is secreted by the alpha cells of the pancreas?
What is the primary function of the duct cells in the pancreas?
What is the primary function of the duct cells in the pancreas?
Which enzyme is inhibited by the brush border enzymes in the intestinal mucosa?
Which enzyme is inhibited by the brush border enzymes in the intestinal mucosa?
How do the pancreatic acinar cells contribute to digestion?
How do the pancreatic acinar cells contribute to digestion?
What is the main role of pancreatic proteases in digestion?
What is the main role of pancreatic proteases in digestion?
Which structure in the pancreas serves as a source for endocrine secretions?
Which structure in the pancreas serves as a source for endocrine secretions?
What part of the small intestine predominantly absorbs bile salts and vitamin B12?
What part of the small intestine predominantly absorbs bile salts and vitamin B12?
Which mechanism is primarily responsible for the absorption of monoglycerides and free fatty acids in the small intestine?
Which mechanism is primarily responsible for the absorption of monoglycerides and free fatty acids in the small intestine?
What role do bile salts play during the digestion of dietary fats?
What role do bile salts play during the digestion of dietary fats?
Which of the following is NOT absorbed by the duodenum and jejunum?
Which of the following is NOT absorbed by the duodenum and jejunum?
What is the primary function of pancreatic lipase in fat digestion?
What is the primary function of pancreatic lipase in fat digestion?
How are triglycerides initially prepared for digestion in the small intestine?
How are triglycerides initially prepared for digestion in the small intestine?
What occurs when micelles approach the absorptive epithelial surface of the small intestine?
What occurs when micelles approach the absorptive epithelial surface of the small intestine?
Why is the absorption of calcium and iron in the small intestine unique?
Why is the absorption of calcium and iron in the small intestine unique?
Flashcards
Duodenum
Duodenum
The first 10 inches of the small intestine, where digestion begins.
Hepatopancreatic region
Hepatopancreatic region
The duodenum receives bile and pancreatic juice through the common bile duct and main pancreatic duct.
CCK action
CCK action
The presence of fatty chyme in the duodenum triggers the release of cholecystokinin (CCK), which stimulates the release of bile and pancreatic enzymes.
Secretin action
Secretin action
Signup and view all the flashcards
Pancreatic functions
Pancreatic functions
Signup and view all the flashcards
What is the Liver?
What is the Liver?
Signup and view all the flashcards
What is Bile?
What is Bile?
Signup and view all the flashcards
What is Fat Emulsification?
What is Fat Emulsification?
Signup and view all the flashcards
What is Enterohepatic Circulation of Bile Salts?
What is Enterohepatic Circulation of Bile Salts?
Signup and view all the flashcards
How is Bile Release Controlled?
How is Bile Release Controlled?
Signup and view all the flashcards
Pancreas Functions
Pancreas Functions
Signup and view all the flashcards
What do duct cells secrete?
What do duct cells secrete?
Signup and view all the flashcards
What do acinar cells secrete?
What do acinar cells secrete?
Signup and view all the flashcards
What are the islets of Langerhans?
What are the islets of Langerhans?
Signup and view all the flashcards
What do beta cells secrete?
What do beta cells secrete?
Signup and view all the flashcards
What do alpha cells secrete?
What do alpha cells secrete?
Signup and view all the flashcards
How are pancreatic enzymes activated?
How are pancreatic enzymes activated?
Signup and view all the flashcards
What is the hepatic portal circulation?
What is the hepatic portal circulation?
Signup and view all the flashcards
What are the main sites of absorption in the small intestine?
What are the main sites of absorption in the small intestine?
Signup and view all the flashcards
What does the ileum primarily absorb?
What does the ileum primarily absorb?
Signup and view all the flashcards
What happens during carbohydrate digestion?
What happens during carbohydrate digestion?
Signup and view all the flashcards
How are carbohydrates absorbed?
How are carbohydrates absorbed?
Signup and view all the flashcards
What occurs during protein digestion?
What occurs during protein digestion?
Signup and view all the flashcards
How are proteins absorbed?
How are proteins absorbed?
Signup and view all the flashcards
What are the main steps in fat digestion?
What are the main steps in fat digestion?
Signup and view all the flashcards
How are fats absorbed?
How are fats absorbed?
Signup and view all the flashcards
Triglyceride Resynthesis
Triglyceride Resynthesis
Signup and view all the flashcards
Chylomicrons
Chylomicrons
Signup and view all the flashcards
Chylomicron Exocytosis
Chylomicron Exocytosis
Signup and view all the flashcards
Large Intestine Function
Large Intestine Function
Signup and view all the flashcards
Vitamin Absorption in the Large Intestine
Vitamin Absorption in the Large Intestine
Signup and view all the flashcards
Gut Microbiota
Gut Microbiota
Signup and view all the flashcards
Short-chain Fatty Acids
Short-chain Fatty Acids
Signup and view all the flashcards
Large Intestine: Key Functions
Large Intestine: Key Functions
Signup and view all the flashcards
Study Notes
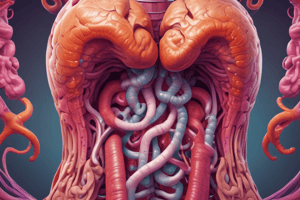
MPharm Programme: The Gastrointestinal System 3
- The week 15 lecture covers the small intestine, its subdivisions, and the hepatopancreatic region.
- The small intestine has three main subdivisions: duodenum, jejunum, and ileum.
- The duodenum plays a crucial role in digestion, as it receives bile and pancreatic juice.
- The hepatopancreatic region is where the common bile duct, the cystic duct, the common hepatic duct, and the pancreatic duct connect.
- The pancreas produces bile and digestive enzymes, including proteases, amylase, and lipase.
- Pancreatic duct cells secrete bicarbonate to neutralize stomach acid.
- The duodenum is the first 10 inches of the small intestine, the primary site of digestion.
- Fatty chyme in the duodenum triggers the release of CCK, a hormone stimulating bile and pancreatic enzyme release.
- Acidic chyme stimulates secretin release, prompting pancreatic bicarbonate release for acid neutralization.
Structure of the Pancreas
- The pancreas has exocrine and endocrine cells.
- Exocrine cells secrete enzymes (e.g., lipase, amylase, proteases) into the duodenum.
- Acinar cells secrete pancreatic juice containing enzymes.
- Duct cells produce bicarbonate to neutralize stomach acid.
- Endocrine cells, located in the islets of Langerhans, secrete hormones insulin and glucagon.
- Insulin regulates blood glucose levels, while glucagon raises them.
Functional Anatomy of Pancreas
- The pancreas's exocrine function involves duct cells secreting bicarbonate, ensuring proper pH conditions for enzyme action in the small intestine.
- Duct cells secrete aqueous bicarbonate solution.
- Acinar cells release pancreatic juice containing enzymes such as proteases, amylase, and lipase.
- The endocrine function within islets of Langerhans involves beta cells (insulin secretion) and alpha cells (glucagon secretion).
Secretions of the Pancreas
- The pancreas releases bicarbonate (NaHCO3) to neutralize acids into the duodenum
- Acinar cells secrete digestive enzymes
- Hormones like insulin and glucagon are released by the endocrine function.
Hormonal Control of Pancreatic Exocrine Secretion
- Acidic chyme in the duodenum triggers secretin release, stimulating pancreatic duct cells to release bicarbonate.
- Fatty or protein chyme in the duodenum triggers CCK, enhancing pancreatic acinar cell enzyme secretion.
Activation of Pancreatic Enzymes
- Inactive enzyme precursors, like trypsinogen, are activated in the duodenum by enteropeptidase.
- Trypsin activates other enzymes via a cascade reaction.
- Trypsin inhibitors control the activation.
The Liver & Hepatic Portal Circulation
- The liver processes nutrients from the digestive tract.
- The hepatic artery carries oxygenated blood to the liver.
- The hepatic portal vein carries deoxygenated blood containing digested nutrients from the digestive tract to the liver.
- Blood exits the liver via the hepatic vein.
The Liver
- The liver is the largest gland in the body.
- It is composed of plates of hepatocytes, specialized liver cells.
- The main digestive function of the liver is bile production.
- Bile emulsifies fats.
- Bile consists of bile salts, bile pigments, cholesterol, neutral fats, phospholipids, and electrolytes.
- Bile is stored in the gallbladder and released into the small intestine as needed.
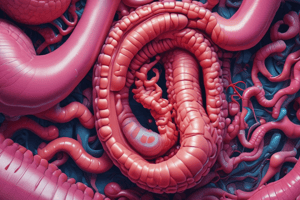
Fat Emulsification by Bile Salts
- Bile salts emulsify fats, increasing the surface area for lipase action.
- Bile salts have hydrophilic (water-loving) and hydrophobic (water-fearing) regions, allowing them to coat fat droplets.
Control of Bile Release
- Cholecystokinin (CCK) stimulates gallbladder contraction and relaxes the hepatopancreatic sphincter.
- Acidic, fatty chyme stimulates the release of CCK and secretin.
- Vagal stimulation causes weak gallbladder contractions.
- Bile salts and secretin stimulate liver.
Enterohepatic Circulation of Bile Salts
- Bile salts are reabsorbed and recycled.
- Approximately 95% of bile salts are reclaimed.
- The remainder is excreted and lost in the feces.
Digestion & Absorption in the Small Intestine
- This section outlines the processes of carbohydrate, protein, and fat digestion and absorption in the duodenum and jejunum.
- Water and electrolytes are freely absorbed
Absorption in Small Intestine
- The duodenum and jejunum are the main sites for nutrient absorption, absorbing carbohydrates, proteins, fats, vitamins, and water.
- Calcium and iron absorption is regulated based on the body's needs.
- The ileum absorbs bile salts, vitamin B12, electrolytes, and water.
Carbohydrate, Protein & Fat Digestion
- Enzymes for carbohydrate, protein, and fat digestion are discussed.
- Specific enzymes such as amylase, proteases, and lipases break down these nutrients into smaller components.
Carbohydrate Digestion
- Dietary carbohydrates are broken down into monosaccharides.
- Salivary and pancreatic amylase break down polysaccharides into disaccharides.
- Enzymes like maltase, sucrase, and lactase convert disaccharides into monosaccharides.
- These monosaccharides are then absorbed.
Carbohydrate Absorption
- Glucose and galactose are absorbed via active transport (symport with Na+).
- Fructose is absorbed via facilitated diffusion.
- Monosaccharides are absorbed into blood stream.
Protein Digestion
- Dietary proteins are initially broken down into smaller peptides by proteases like pepsin.
- Pancreatic proteases further digest peptides into amino acids and dipeptides/tripeptides.
- Aminopeptidases break down peptides into single amino acids.
Protein Absorption
- Amino acids are absorbed via active transport or facilitated diffusion mechanisms.
- Small peptides can also be absorbed in certain cases using H+ cotransport.
Fat Digestion and Absorption
- Bile salts emulsify dietary fat.
- Pancreatic lipase breaks down triglycerides into fatty acids and monoglycerides.
- These products form micelles, which carry them to the intestinal lining.
- Fatty acids and monoglycerides are absorbed and reassembled into triglycerides.
- Chylomicrons encapsulate the triglycerides and transport them into the lymphatic system.
Iron Absorption
- Dietary iron is absorbed in the ferrous form or as heme.
- Ferrous iron enters cells mediated by divalent metal transporter 1.
- Absorbed iron can be transported into blood by membrane protein ferroportin.
- Stored iron is in the form of ferritin.
- Unused iron is lost in the feces.
The Large Intestine
- The large intestine (colon, cecum, appendix, rectum) is primarily a drying and storage organ.
- It absorbs water, electrolytes, and several B vitamins, vitamin K, and folic acid.
- It houses beneficial bacteria that aid in producing vitamin K and folic acid and producing short-chain fatty acids.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.