Podcast
Questions and Answers
Which statement accurately contrasts upper motor neurons (UMNs) and lower motor neurons (LMNs)?
Which statement accurately contrasts upper motor neurons (UMNs) and lower motor neurons (LMNs)?
- UMNs use acetylcholine as their primary neurotransmitter, unlike LMNs which use glutamate.
- UMNs transmit motor impulses from the brain to LMNs, while LMNs transmit impulses to muscles. (correct)
- UMNs are located in the brainstem and spinal cord, while LMNs are in the cerebral cortex.
- UMNs directly innervate muscles, whereas LMNs synapse with interneurons.
Following a motor vehicle accident, a patient exhibits spastic paralysis, increased DTRs, and a positive Babinski sign. Where is the most probable location of the lesion?
Following a motor vehicle accident, a patient exhibits spastic paralysis, increased DTRs, and a positive Babinski sign. Where is the most probable location of the lesion?
- Cerebellum
- Basal ganglia
- Upper motor neuron (correct)
- Lower motor neuron
What is a key difference between the signs of upper motor neuron (UMN) and lower motor neuron (LMN) lesions?
What is a key difference between the signs of upper motor neuron (UMN) and lower motor neuron (LMN) lesions?
- UMN lesions result in disuse atrophy, unlike LMN lesions which lead to severe atrophy.
- UMN lesions typically present with flaccid paralysis, while LMN lesions present with spastic paralysis.
- UMN lesions involve increased muscle tone, whereas LMN lesions involve decreased muscle tone. (correct)
- UMN lesions show fasciculations, while LMN lesions do not.
Which of the following best describes the term 'paresis' in the context of motor tract lesions?
Which of the following best describes the term 'paresis' in the context of motor tract lesions?
What is the clinical significance of the Babinski sign?
What is the clinical significance of the Babinski sign?
In the context of spinal cord injuries (SCIs), what is characteristic of muscle spasms related to cutaneous stimuli?
In the context of spinal cord injuries (SCIs), what is characteristic of muscle spasms related to cutaneous stimuli?
Which of the following best describes 'clonus'?
Which of the following best describes 'clonus'?
What is the underlying mechanism of the clasp-knife response observed in some patients with motor disorders?
What is the underlying mechanism of the clasp-knife response observed in some patients with motor disorders?
Which term refers to abnormally high resistance to passive stretch that increases with faster movement?
Which term refers to abnormally high resistance to passive stretch that increases with faster movement?
What is a key characteristic of rigidity that differentiates it from spasticity?
What is a key characteristic of rigidity that differentiates it from spasticity?
A patient presents with rigid extension of the upper and lower limbs. Which term best describes this condition?
A patient presents with rigid extension of the upper and lower limbs. Which term best describes this condition?
Which condition is commonly associated with lower motor neuron (LMN) disorders?
Which condition is commonly associated with lower motor neuron (LMN) disorders?
Cell bodies of lower motor neurons (LMNs) are located in which area of the spinal cord?
Cell bodies of lower motor neurons (LMNs) are located in which area of the spinal cord?
What is the function of gamma motor neurons?
What is the function of gamma motor neurons?
Which of the following describes the role of the Golgi tendon organ (GTO)?
Which of the following describes the role of the Golgi tendon organ (GTO)?
What is a characteristic of a reflex response?
What is a characteristic of a reflex response?
Which type of reflex involves direct communication between a sensory and motor neuron, bypassing an interneuron?
Which type of reflex involves direct communication between a sensory and motor neuron, bypassing an interneuron?
What is the purpose of using Electromyography (EMG) in diagnostic studies?
What is the purpose of using Electromyography (EMG) in diagnostic studies?
What is the primary function of motor tracts?
What is the primary function of motor tracts?
Which of the following is a key characteristic of the anterior corticospinal tract?
Which of the following is a key characteristic of the anterior corticospinal tract?
The lateral corticospinal tract is responsible for which of the following functions?
The lateral corticospinal tract is responsible for which of the following functions?
Which of the following describes the rubrospinal tract?
Which of the following describes the rubrospinal tract?
What is the primary function of the tectospinal tract?
What is the primary function of the tectospinal tract?
Where does the reticulospinal tract originate?
Where does the reticulospinal tract originate?
What is the primary function of the vestibulospinal tracts?
What is the primary function of the vestibulospinal tracts?
Which statement best describes the function of the medial vestibulospinal tract?
Which statement best describes the function of the medial vestibulospinal tract?
What is the role of the muscle spindle in muscle function?
What is the role of the muscle spindle in muscle function?
Given a scenario where a patient displays fasciculations, which of the following can be inferred?
Given a scenario where a patient displays fasciculations, which of the following can be inferred?
How does the function of the medial pathways compare to the lateral pathways in the context of motor control?
How does the function of the medial pathways compare to the lateral pathways in the context of motor control?
During a physical examination, a patient's resistance to passive movement remains constant, regardless of the speed of force application. What type of muscle tone abnormality is most likely present?
During a physical examination, a patient's resistance to passive movement remains constant, regardless of the speed of force application. What type of muscle tone abnormality is most likely present?
Which of the following best correlates with the term 'myoplasticity' in the context of motor tract lesions?
Which of the following best correlates with the term 'myoplasticity' in the context of motor tract lesions?
Why is somatosensory information utilized to prepare for movement (feedforward)?
Why is somatosensory information utilized to prepare for movement (feedforward)?
What is the role of calcium ions ($Ca^{2+}$) in muscle contraction?
What is the role of calcium ions ($Ca^{2+}$) in muscle contraction?
What is the role of Acetylcholine (Ach) in muscle contraction?
What is the role of Acetylcholine (Ach) in muscle contraction?
During muscle contraction, when do the actin slides relative to the myosin?
During muscle contraction, when do the actin slides relative to the myosin?
What is the significance of the H Zone during muscle relaxation?
What is the significance of the H Zone during muscle relaxation?
Flashcards
Skeletal muscle properties
Skeletal muscle properties
Skeletal muscle has the properties of being excitable, contractile, extensile, and elastic.
Acetylcholine (ACh)
Acetylcholine (ACh)
A neurotransmitter released from synaptic vesicles, exciting the skeletal muscle fiber.
Excitation-Contraction Coupling
Excitation-Contraction Coupling
ACh binding triggers an action potential along the sarcolemma and T-tubules, stimulating the sarcoplasmic reticulum to release Ca2+.
Role of Calcium in Muscle Contraction
Role of Calcium in Muscle Contraction
Signup and view all the flashcards
Upper Motor Neurons (UMN)
Upper Motor Neurons (UMN)
Signup and view all the flashcards
Lower Motor Neurons (LMN)
Lower Motor Neurons (LMN)
Signup and view all the flashcards
Hemiplegia
Hemiplegia
Signup and view all the flashcards
Paraplegia
Paraplegia
Signup and view all the flashcards
Tetraplegia
Tetraplegia
Signup and view all the flashcards
Babinski's Sign
Babinski's Sign
Signup and view all the flashcards
Clonus
Clonus
Signup and view all the flashcards
Clasp-Knife Response
Clasp-Knife Response
Signup and view all the flashcards
Muscle Tone
Muscle Tone
Signup and view all the flashcards
Rigidity
Rigidity
Signup and view all the flashcards
Lower Motor Neurons
Lower Motor Neurons
Signup and view all the flashcards
Alpha Motor Neurons
Alpha Motor Neurons
Signup and view all the flashcards
Gamma Motor Neurons
Gamma Motor Neurons
Signup and view all the flashcards
Golgi Tendon Organ
Golgi Tendon Organ
Signup and view all the flashcards
Reflexes
Reflexes
Signup and view all the flashcards
Reflex Arc
Reflex Arc
Signup and view all the flashcards
Monosynaptic Reflex
Monosynaptic Reflex
Signup and view all the flashcards
Polysynaptic Reflex
Polysynaptic Reflex
Signup and view all the flashcards
Rubrospinal Tract
Rubrospinal Tract
Signup and view all the flashcards
Tectospinal Tract
Tectospinal Tract
Signup and view all the flashcards
Lateral Corticospinal Tract
Lateral Corticospinal Tract
Signup and view all the flashcards
Study Notes
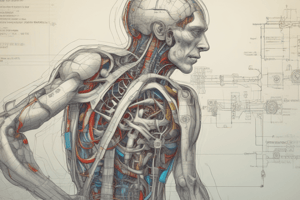
- Motor systems involve the structures in the nervous system responsible for controlling movement
- Dana McPhee PT, MS, NCS and Megan Slayton, PT, DPT, NCS are credited for the presentation
- It was created for the SFCC PTA/OTA Program, Winter 2023
Spinal Cord Anatomy Review
- The dorsal horns of the spinal cord contain sensory information.
- The ventral horns contain motor neurons.
- Ascending pathways relay sensory information to the brain.
- Descending pathways transmit motor commands from the brain to the spinal cord.
Muscle Anatomy
- Skeletal muscle is excitable, contractile, extensible, and elastic
- Muscle fiber contains myofibrils.
- Myofibrils contain sarcomeres delineated by Z lines.
- Sarcomeres which are composed of actin and myosin myofilaments
- Muscle contraction occurs through the sliding of actin relative to myosin.
Muscle Contraction Steps
- A nerve impulse reaches the neuromuscular junction, causing the release of acetylcholine (ACh).
- ACh diffuses across the synaptic cleft, opening Na+ channels in the muscle membrane.
- Na+ entry depolarizes the muscle cell.
- T-tubules transmit impulses to the sarcoplasmic reticulum, releasing Ca2+ ions.
- Ca2+ binds to troponin, exposing actin binding sites.
- Myosin binds to actin, forming cross-bridges.
- ATP is used to facilitate cross-bridge movement and subsequent actin strand pulling.
- Another ATP molecule is used for the recovery stroke which is responsible for the bend, attach and pull.
- When the action potential ceases, Ca2+ is pumped back into the sarcoplasmic reticulum, and tropomyosin covers the binding sites, preventing further myosin binding.
Sliding Filament Model
- Active sites on actin are exposed, allowing myosin heads to bind
- Myosin heads bend, pulling thin filaments
- Each head releases, binds to the next active site, and pulls again
- Action results in entire myofibril shortening
Upper vs. Lower Motor Neurons
- Upper motor neurons (UMNs) located in the cerebral cortex or brainstem, transmit motor impulses to the lower motor neurons. UMNs use glutamate
- Lower motor neurons (LMNs) located in the brainstem and spinal cord, transmit impulses from the UMNs to the muscles. LMNs use acetylcholine
- UMN damage results in Spastic paralysis, Increased DTR's, Pathological reflex present, Fasciculations absent
- LMN damage results in Flaccid paralysis, Severe atrophy, Absent DTR's, Absent pathological reflex, Fasciculations present
Motor Tract Lesions
- Signs of motor tract lesions include paresis/paralysis, abnormal reflexes, myoplasticity, abnormal muscle tone, loss of fractionated movements, and abnormal muscle synergies
- Hemiplegia is weakness on one side of the body
- Paraplegia affects the body below the arms
- Tetraplegia affects all four limbs
- Paresis in MT lesions from inadequate MN facilitation
- Paralysis occurs in muscles below a complete spinal cord lesion
Abnormal Cutaneous Reflexes
- Babinski's sign is extension of the great toe with fanning of other toes
- Test by stroking the lateral sole firmly
- Muscle stretch hyperreflexia, clonus, and clasp-knife response are common abnormal reflexes in chronic SCI
Clonus
- Clonus is involuntary, repeating, rhythmic muscle contractions
- Unsustained clonus fades after a few beats
- Sustained clonus is pathologic in origin, activates oscillating neural networks due to a MT control lack in the spinal cord
Clasp-Knife Response
- Clasp-knife response occurs when a paretic muscle is slowly stretched and resistance drops notably
- A change in resistance akin to a pocketknife opening resistance
- Type II afferents elicit the clasp-knife response
Muscle Tone Assessment
-
Muscle tone is assessed via PROM
-
Resistance to passive stretch in a resting muscle
-
Potential findings include:
- Hypotonia
- Hypertonia
- Spasticity
- Rigidity
- Modified Ashworth Scale
Abnormal Muscle Tone
- Resistance to stretch in resting muscle
- Muscle tone categorized on a continuum
- Resistance ranges from flaccid through normal to hypertonic to rigidity
- Velocity-dependent hypertonia is referred to as spasticity
Rigidity
- Resistance to passive movement
- Remains constant regardless of speed
- Velocity-dependent hypertonia
- Decerebrate rigidity: Rigid extension of upper limbs
- Decorticate rigidity: Flexed upper limbs, extended neck/lower limbs, plantarflexion
Disorders of Motor Neurons
- Lower motor neuron disorders include trauma, metabolic disorders (alcohol, diabetic neuropathy), myasthenia gravis, polio, Guillain-Barré, brachial plexus injury, carpal tunnel syndrome, multiple sclerosis, coma.
- Upper motor neuron disorders include amyotrophic lateral sclerosis, multiple sclerosis, cerebral vascular accident, cerebral palsy, tumors, trauma, infections, hypoxia.
Lower Motor Neurons
- The only neurons to convey signals to muscle spindle fibers
- Cell bodies in ventral horn
- Axons leave SC at ventral nerve root
- Neurons projecting to a single muscle form a motor pool
Motor Neurons
- Motor neurons in the medial ventral horn innervate muscles of the neck & back (axial & proximal)
- Motor neurons in the lateral ventral horn innervate distal muscles
- Motor neurons in the anterior ventral horn innervate extensor muscle groups
- Motor neurons in the posterior ventral horn innervate flexor muscle groups
Alpha and Gamma Motor Neurons
- MNs have large cell bodies and large myelinated axons
- Innervate extrafusal skeletal muscle, responsible for muscle contraction
- Medium sized. myelinated axons
- Project to intrafusal fibers in the muscle spindle
- Gamma motor neurons innervate what???
- Maintain the sensitivity of the muscle spindle throughout the normal range of muscle length
- Responsible for Proprioception
- Action results in Isometric mm contraction
Muscle Spindle vs. Golgi Tendon Organ
- Muscle spindles are small spindle-shaped sensory organs sensing length changes and lengthening rate
- Golgi tendon organs are sensory organs in the muscle-tendon unit sensing muscle tension changes
- During contraction, muscle spindles contract
- Golgi tendon organs however do not contract
- Muscle spindle protective function results in the Stretch reflex and reciprocal inhibition
- Golgi tendon organs leads to Autogenic inhibition
- Differentiated muscle fibers are held in a connective tissue sac
- Golgi tendon organs are braided collagen strands which are encapsulated
Golgi Tendon Organ
- GTO's Autogenic inhibition results in inhibition within same muscle stimulated
- Reciprocal Inhibition creates inhibition within functional opposing muscle
Reflex Characteristics
- Reflexes are rapid, preprogrammed, involuntary responses.
- Reflexes require a stimulus, and are always the same.
- Reflexes are a survival mechanism
Reflex Arc
- The neural pathway is responsible for generating the response
- Stimulus activates receptor
- Nerve signal propagated via sensory neuron to SC
- Signal processed in integration center by interneurons
- Signal propagated by motor neuron to effector
- Effector responds
Monosynaptic vs. Polysynaptic Reflexes
- Monosynaptic reflexes have direct communication between sensory & motor neurons (e.g., stretch reflex)
- Polysynaptic reflexes have interneurons facilitating sensory-motor communication (e.g., withdrawal reflex)
Involuntary Muscle Contractions
- Muscle cramps
- Fasciculations
- Myoclonus
- Fibrillations
- Tremors
- Movements related to BG dysfunction
Motor Neuron Lesions
- Interrupting MNs signal reduces/prevents muscle contraction
- Damage to MNs caused by trauma, demyelinating diseases (GBS), infection, or chronic neuropathy (DM)
Diagnostic Studies
- Nerve conduction studies
- Useful as a diagnostic tool
- Can differentiate between dysfunction at different sites
- the nerve
- neuromuscular junction
- the muscle
- Electromyography (EMG):
- Useful as a diagnostic tool
- Can differentiate denervated muscle from myopathy
Motor Tracts
- Arise in cerebral cortex or brainstem
- Axons travel in descending tracts to synapse with MNs/interneurons in brainstem/spinal cord
- Cerebellum/BG are key in adjusting motor tract activity
- Classified according to the location of synapse
Descending Tracts
- They control movement, muscle tone, spinal reflexes, spinal autonomic functions, and sensory transmission modulation.
- They are divided into pyramidal (corticospinal) and extrapyramidal tracts (rubrospinal, vestibulospinal, reticulospinal, tectospinal).
- Each descending tract contains two interconnecting neurons
- First-order motor neurons originate in the cerebral cortex/brainstem and travel down the spinal cord, synapsing in the anterior gray horn.
- Second-order neurons travel from the spinal cord to skeletal muscles.
- There are two main pathways for cortex/brainstem to control movement: medial and lateral.
- Medial pathways control axial and proximal muscles, while lateral pathways control distal extremity muscles
Reticulospinal Tract
- Begins in the reticular formation
- Facilitates bilateral motor neurons innervating postural & gross limb movement muscles
- Coordinates movement of proximal muscles during walking
- Involved in anticipatory postural adjustments & reaching
- Creates a pathway for neck reflexes to respond to visual/auditory input
Vestibulospinal Tract
- Lateral vestibulospinal tract
- Lateral vestibular nuclei respond to gravity from vestibular apparatus I- psilateral motor neurons facilitate extensors, inhibiting ipsilateral motor neurons to flexors
- Excites extensor muscles of trunk and proximal anti-gravity muscles
- Maintains person's COG within BOS
- Medial vestibulospinal tract
- Medial vestibular nuclei get info about head movement positions from the vestibular apparatus
- Projects bilaterally to cervical & thoracic spinal cord
- Impacts Motor neurons to control neck/upper back muscles
Rubrospinal Tract
- Non-pyramidal route
- Motor cortex & cerebellum which influence spinal motor actiivity
- Originates in the Red nucleus and ends at levels of the spinal cord
- Controls tone of limb flexor muscles
- Has an important role in a number of body reflexes
Tectospinal Tract
- Aka colliculospinal tract
- Originates in superior colliculus, crosses, descends in brainstem
- Mediates reflex postural movements of head/neck, in response to visual/auditory stimuli directing eyes/head towards objects in visual field
Anterior Corticospinal Tract
- Originated in the cerebral cortex, fiber tracts do not cross to the pyramidal dessucation
- Contralateral with spinal cord, terminate in that side of the Spinal cord
- Controls axial and proximal muscles of the neck and trunk
Lateral Corticospinal Tract
- Originates in cerebral cortex: premotor, primary motor, and supplementary motor areas
- Fibers cross in pyramidal decussation
- Synapses onto neurons to control muscles of extremities
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.