Podcast
Questions and Answers
What is a distinguishing feature of the mollicutes group?
What is a distinguishing feature of the mollicutes group?
- Lack of a definite cell wall (correct)
- Presence of a rigid cell wall
- Resistance to osmotic lysis
- Sensitivity to penicillin
Which mycoplasma is most commonly associated with atypical pneumonia in humans?
Which mycoplasma is most commonly associated with atypical pneumonia in humans?
- Mycoplasma hominis
- Mycoplasma genitalium
- Mycoplasma pneumoniae (correct)
- Mycoplasma mycoides
What potential complication is associated with the use of an IUCD for more than one year?
What potential complication is associated with the use of an IUCD for more than one year?
- Chronic pelvic pain
- Endometritis (correct)
- Uterine cancer
- Ectopic pregnancy
What is the appearance of colonies developed by mollicutes on solid culture media?
What is the appearance of colonies developed by mollicutes on solid culture media?
What is the recommended initial treatment approach for infections caused by mollicutes, given their resistance profile?
What is the recommended initial treatment approach for infections caused by mollicutes, given their resistance profile?
What is a characteristic feature of Actinomycetes?
What is a characteristic feature of Actinomycetes?
Which disease is primarily associated with Actinomyces israelii?
Which disease is primarily associated with Actinomyces israelii?
What is the standard treatment for Actinomycosis?
What is the standard treatment for Actinomycosis?
Which of the following is an incorrect statement about Nocardia species?
Which of the following is an incorrect statement about Nocardia species?
How does Nocardia typically infect humans?
How does Nocardia typically infect humans?
What type of bacteria is Mycoplasma pneumoniae classified as?
What type of bacteria is Mycoplasma pneumoniae classified as?
What is the primary ecological niche for Nocardia species?
What is the primary ecological niche for Nocardia species?
Which of the following is NOT a characteristic of aerobic actinomycetes?
Which of the following is NOT a characteristic of aerobic actinomycetes?
What is the primary mechanism by which Mycoplasma pneumoniae attaches to the respiratory epithelium?
What is the primary mechanism by which Mycoplasma pneumoniae attaches to the respiratory epithelium?
Which of the following clinical manifestations is least associated with Mycoplasma infections?
Which of the following clinical manifestations is least associated with Mycoplasma infections?
What best describes the growth characteristics of Mycoplasma pneumoniae?
What best describes the growth characteristics of Mycoplasma pneumoniae?
During Mycoplasma pneumoniae infection, what is the role of CARDS toxin?
During Mycoplasma pneumoniae infection, what is the role of CARDS toxin?
Which age group is most commonly affected by Mycoplasma pneumoniae infections?
Which age group is most commonly affected by Mycoplasma pneumoniae infections?
What type of pneumonia is primarily caused by Mycoplasma pneumoniae?
What type of pneumonia is primarily caused by Mycoplasma pneumoniae?
How is Mycoplasma pneumoniae commonly transmitted between individuals?
How is Mycoplasma pneumoniae commonly transmitted between individuals?
In what condition is the Mycoplasma pneumoniae infection underestimated due to its similarity to other illnesses?
In what condition is the Mycoplasma pneumoniae infection underestimated due to its similarity to other illnesses?
Which of the following is a consequence of M.pneumonia infection affecting epithelial cells?
Which of the following is a consequence of M.pneumonia infection affecting epithelial cells?
What is the duration of pathogen harboring in individuals recovered from Mycoplasma infection?
What is the duration of pathogen harboring in individuals recovered from Mycoplasma infection?
What is the primary method used to conclusively identify Mycoplasma pneumoniae?
What is the primary method used to conclusively identify Mycoplasma pneumoniae?
Which statement accurately describes L-forms of bacteria?
Which statement accurately describes L-forms of bacteria?
What distinguishes pleuropneumonia-like organisms (PPLO) from other bacteria?
What distinguishes pleuropneumonia-like organisms (PPLO) from other bacteria?
What is a significant characteristic of Mycoplasma and L-forms regarding their cellular structure?
What is a significant characteristic of Mycoplasma and L-forms regarding their cellular structure?
In what way does multiplication of bacteria without a rigid cell wall differ from typical bacteria?
In what way does multiplication of bacteria without a rigid cell wall differ from typical bacteria?
What is the key feature of T-strains in mycoplasmas?
What is the key feature of T-strains in mycoplasmas?
What is a common environmental condition that can lead to the formation of L-forms?
What is a common environmental condition that can lead to the formation of L-forms?
Which statement is FALSE regarding Mycoplasma pneumoniae compared to L-forms?
Which statement is FALSE regarding Mycoplasma pneumoniae compared to L-forms?
What are the conditions that can lead to bacteria becoming L-forms?
What are the conditions that can lead to bacteria becoming L-forms?
What is a distinguishing factor of the cell membranes in mycoplasmas?
What is a distinguishing factor of the cell membranes in mycoplasmas?
What structural feature distinguishes mycoplasmas from typical bacteria?
What structural feature distinguishes mycoplasmas from typical bacteria?
Which staining method would be ineffective in identifying mycoplasmas due to their cell wall structure?
Which staining method would be ineffective in identifying mycoplasmas due to their cell wall structure?
What is the typical diameter range of mycoplasmas?
What is the typical diameter range of mycoplasmas?
Which antibiotic is ineffective against mycoplasmas due to their lack of a cell wall?
Which antibiotic is ineffective against mycoplasmas due to their lack of a cell wall?
What type of environment do most mycoplasmas require for growth?
What type of environment do most mycoplasmas require for growth?
Which unique characteristic is associated with Mycoplasma pneumoniae's mode of movement?
Which unique characteristic is associated with Mycoplasma pneumoniae's mode of movement?
What component is crucial for the growth and survival of mycoplasmas?
What component is crucial for the growth and survival of mycoplasmas?
Which toxin is produced by Mycoplasma pneumoniae that is associated with respiratory diseases?
Which toxin is produced by Mycoplasma pneumoniae that is associated with respiratory diseases?
How does the plasma membrane of mycoplasmas compare to that of animal cells?
How does the plasma membrane of mycoplasmas compare to that of animal cells?
Which of the following statements is true regarding the genetic material of mycoplasmas?
Which of the following statements is true regarding the genetic material of mycoplasmas?
Flashcards
Actinomycetes
Actinomycetes
Elongated, branching, slow-growing gram-positive rods that are often found in the oral and intestinal flora. They can cause chronic cellulitis and draining sinuses.
Actinomycosis
Actinomycosis
A disease caused by Actinomycetes characterized by chronic cellulitis and the formation of draining sinuses. Most infections are caused by A. israelii.
Nocardia
Nocardia
A genus of aerobic actinomycetes that are gram-positive, branching, filamentous bacteria. They are slow-growing, poorly stained, and can cause a variety of infections.
Nocardia asteroides complex
Nocardia asteroides complex
Signup and view all the flashcards
Nocardia farcinica
Nocardia farcinica
Signup and view all the flashcards
Nocardia: Ecology & Epidemiology
Nocardia: Ecology & Epidemiology
Signup and view all the flashcards
Nocardia: Transmission
Nocardia: Transmission
Signup and view all the flashcards
Nocardia: Treatment & Prevention
Nocardia: Treatment & Prevention
Signup and view all the flashcards
What are Mycoplasmas?
What are Mycoplasmas?
Signup and view all the flashcards
Why are Mycoplasmas resistant to some antibiotics?
Why are Mycoplasmas resistant to some antibiotics?
Signup and view all the flashcards
What is the unique structure of Mycoplasmas?
What is the unique structure of Mycoplasmas?
Signup and view all the flashcards
How did Mycoplasmas evolve?
How did Mycoplasmas evolve?
Signup and view all the flashcards
What is the PPO?
What is the PPO?
Signup and view all the flashcards
How large are Mycoplasmas?
How large are Mycoplasmas?
Signup and view all the flashcards
Describe the shape of Mycoplasmas.
Describe the shape of Mycoplasmas.
Signup and view all the flashcards
How does Gram staining affect Mycoplasmas?
How does Gram staining affect Mycoplasmas?
Signup and view all the flashcards
What is the terminal organelle?
What is the terminal organelle?
Signup and view all the flashcards
What toxin does Mycoplasma pneumoniae produce?
What toxin does Mycoplasma pneumoniae produce?
Signup and view all the flashcards
What is Mycoplasma pneumoniae?
What is Mycoplasma pneumoniae?
Signup and view all the flashcards
How does Mycoplasma pneumonia infect the respiratory system?
How does Mycoplasma pneumonia infect the respiratory system?
Signup and view all the flashcards
What is 'walking pneumonia'?
What is 'walking pneumonia'?
Signup and view all the flashcards
How does Mycoplasma pneumoniae infection spread?
How does Mycoplasma pneumoniae infection spread?
Signup and view all the flashcards
What are the symptoms of Mycoplasma pneumonia?
What are the symptoms of Mycoplasma pneumonia?
Signup and view all the flashcards
How does Mycoplasma pneumonia cause damage to the respiratory system?
How does Mycoplasma pneumonia cause damage to the respiratory system?
Signup and view all the flashcards
What is unusual about the duration of Mycoplasma pneumoniae infection?
What is unusual about the duration of Mycoplasma pneumoniae infection?
Signup and view all the flashcards
Who is most susceptible to Mycoplasma pneumonia?
Who is most susceptible to Mycoplasma pneumonia?
Signup and view all the flashcards
Is there a specific season for Mycoplasma pneumonia?
Is there a specific season for Mycoplasma pneumonia?
Signup and view all the flashcards
How is Mycoplasma pneumonia diagnosed and treated?
How is Mycoplasma pneumonia diagnosed and treated?
Signup and view all the flashcards
Perianal Actinomycosis
Perianal Actinomycosis
Signup and view all the flashcards
Kidney, Ureter, and Bladder (KUB) Infections
Kidney, Ureter, and Bladder (KUB) Infections
Signup and view all the flashcards
Pelvic Actinomycosis
Pelvic Actinomycosis
Signup and view all the flashcards
Diagnosis of Actinomycosis
Diagnosis of Actinomycosis
Signup and view all the flashcards
Mollicutes (Mycoplasmas)
Mollicutes (Mycoplasmas)
Signup and view all the flashcards
Mycoplasma pneumoniae infection
Mycoplasma pneumoniae infection
Signup and view all the flashcards
Nucleic Acid Probes for M. pneumoniae
Nucleic Acid Probes for M. pneumoniae
Signup and view all the flashcards
L-forms of bacteria
L-forms of bacteria
Signup and view all the flashcards
Difference between L-forms and Mycoplasma
Difference between L-forms and Mycoplasma
Signup and view all the flashcards
Pleuropneumonia-like organisms (PPLO)
Pleuropneumonia-like organisms (PPLO)
Signup and view all the flashcards
T-strains of Mycoplasma
T-strains of Mycoplasma
Signup and view all the flashcards
Multiplication of Mycoplasma
Multiplication of Mycoplasma
Signup and view all the flashcards
Antibiotic Resistance in Mycoplasma
Antibiotic Resistance in Mycoplasma
Signup and view all the flashcards
Morphological diversity of Mycoplasma
Morphological diversity of Mycoplasma
Signup and view all the flashcards
Lack of sterols in Mycoplasma
Lack of sterols in Mycoplasma
Signup and view all the flashcards
Study Notes
Microbiology Lecture 13: Actinomycetes, Mycoplasma, and Cell Wall-Defective Bacteria
- Lecture covers Actinomycetes, norcardiosis, actinomycetoma, Mycoplasma, and cell wall-defective bacteria.
Actinomycetes
- Elongated Gram-positive rods
- Branching morphology
- Slow growth (4-10 days)
- Microaerophilic or strictly anaerobic
- Source: oral/intestinal endogenous flora
- Disease: chronic cellulitis, draining sinuses
- Lesion: composed of inflammatory sinuses that discharge to the surface
- Major cause: Actinomyces israelii
Actinomycosis
- Part of normal intestinal microflora
- Endogenous infection; growth requires displacement into tissue (surgery, trauma, etc.)
- Sinus tracts contain pus and sulfur granules
- Little evidence of immunity
- Treatment: Penicillin G
Aerobic Actinomycetes (Genus)
- Aerobic Gram-positive branching filamentous bacteria
- Slow growth (2-3 days)
- Poorly stained
- Subgroups:
- Nocardia
- Actinomadura
- Streptomyces
- Rhodococcus
- Gordonia
- Tsukamurella
- Tropheryma whipplei
Nocardia: History
- Edmond Nocard, 1888
- Aerobic actinomycetes isolated from cattle with bovine farcy
Nocardia: Growth on Blood Agar
- (Image of bacterial growth on blood agar)
Nocardia: Species and Human Infections
- At least 13 species cause human infections
- 7 most important species:
- Nocardia asteroides complex: 80% of noncutaneous; most systemic & CNS nocardiosis
- Nocardia farcinica: Less common, more virulent, more antibiotic-resistant
- Nocardia nova
- Nocardia brasiliensis: Skin, cutaneous, lymphocutaneous
- Nocardia pseudobrasiliensis: Systemic infections, CNS
- Nocardia otitidiscaviarum
- Nocardia transvalensis
Nocardia: Ecology & Epidemiology
- Ubiquitous environmental saprophyte
- Soil, organic matter, water
- Tropical and subtropical regions (Mexico, Central and South America, Africa, India)
- Nearly all cases are sporadic
- Human-to-human transmission not documented
- Animal-to-human transmission not documented
- Outbreaks: Contamination of the hospital environment, solutions, or drug injection equipment
- Occurrence in immunocompromised patients is increased
- Transmission by: Inhalation and Skin
- Risk of pulmonary or disseminated disease is associated with deficient cell-mediated immunity, such as in the following conditions: Alcoholism, Diabetes, Lymphoma, Transplantation, Glucocorticoid therapy, AIDS
Nocardia: Pathogenesis
- Neutralization of oxidants
- Prevention of phagosome-lysosome fusion
- Prevention of phagosome acidification
- Mycolic acid polymers associated with virulence
Nocardia: Clinical Manifestations
- 4 main forms:
- Lymphocutaneous syndrome
- Pulmonary nocardiosis (pneumonia)
- CNS nocardiosis (brain abscess)
- Disseminated disease (Eyes (retina), Skin, Subcutaneous tissue, Kidneys, Joints, Bone, Heart)
Lymphocutaneous Syndrome
- Ubiquitous in soil; inoculation injuries or contaminated abrasions from insect and animal bites
- N. brasiliensis is most common
- N. asteroides is typically self-limited
- Disease duration: Days to months
- Common site: Distal limb
Pulmonary Disease
- Subacute (more acute in immunocompromised); cough with small amounts of thick, purulent sputum; fever, anorexia, weight loss, malaise
- Endobronchial inflammatory mass
- Lung abscess
- Cavitary disease
- Inadequate therapy may lead to progressive fibrotic diseases
- Cerebral imaging is recommended in all cases of pulmonary and disseminated nocardiosis.
CNS Nocardiosis (Brain Abscess)
- Common presentations: insidious presentations mistaken for neoplasia; granulomas & abscesses, often affecting the cerebral cortex, basal ganglia, or midbrain.
- Less commonly, spinal cord or meninges may be affected
- Brain tissue diagnosis in pulmonary nocardiosis may NOT be needed
- Cerebral biopsy: common in immunocompromised patients
Laboratory Diagnosis (Nocardia)
- Gram-positive, beaded, and branching filaments
- Standard blood culture may take 48-hours to several weeks
- Colonies can be grown from sputum from patients with underlying lung disease
- Deep-seated or disseminated disease that fails initial therapy and relapses after therapy warrants an alternative treatment based on susceptibility testing
- Susceptibility to sulfonamide may be crucial in deciding on a treatment or treatment modification
Management (Nocardia): Medication
- Sulfonamides: Mainstay of therapy (N. brasiliensis, N. asteroides complex)
- Severely ill patients with CNS or disseminated infections/immunocompromised patients require additional drugs such as Amikacin and Carbapenem OR 3rd generation cephalosporin.
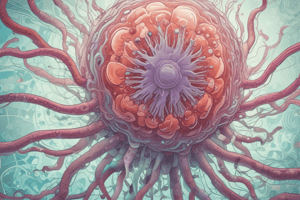
Mycoplasma (Mollicutes)
- Smallest known free-living organisms
- Lack a cell wall
- Not stained by Gram stain; more pleomorphic/plastic than eubacteria
- Staining: Giemsa stain (pleomorphic cocci, rods, spirals, and sometimes as hollow ring forms) ; diameter: 0.15 μ to 0.30 μ
- Genera: Mycoplasma, Ureaplasma, Acholeplasma, Anaeroplasma, Spiroplasma
Mycoplasma: Structure
- Enclosed by a limiting membrane similar to animal cells
- Contain sterols; cytoplasm with ribosomes, but lack mesosomes
- No nuclear membrane
- Some strains have amorphous material on outer membrane, suggesting a capsule
Mycoplasma: Structure (Terminal Organelle)
- Terminal organelle; mediates attachments and gliding motility
- Proteins (P1, P30) responsible for attachment
Mycoplasma: Growth and Replication
- Requires sterols for growth
- Cultivation: Can be grown on laboratory media
- Most are facultatively anaerobic; M. pneumoniae is an exception (aerobic)
- Replication is controversial; replication time: 1-6 hours
Mycoplasma: Toxin Production
- M. pneumoniae produces an ADP-ribosylating toxin: Commonly Associated Respiratory Disease Syndrome (CARDS) toxin
- Lab: Colonies bind red blood cells to agar plate cultures (hemadsorption)
Mycoplasma: Clinical Features
- Also known as Eaton's agent
- Extracellular pathogen
- Attaches to respiratory epithelium by an attachment factor: P1.
- Interacts with glycoprotein receptors on epithelial cell surface
- Ciliostasis is followed by epithelial cell destruction.
Mycoplasma Pneumonia: Clinical Features
- Low infectious dose
- Walking pneumonia
- Frequently confused with virus infection (primary atypical clinical manifestations)
- Tracheobronchitis
- Pharyngitis (use differential diagnosis from strep throat)
Mycoplasma Infections: Spread
- Worldwide; all ages
- Transmission by droplets of nasopharyngeal secretions
- Important in military personnel
- Epidemics: Intervals of 4-6 years
- Retained by pathogens in recovered patients; common in 5-15-year-old adolescents/teenagers more than in older groups of patients
- Infections in children under 6 months are uncommon
- No seasonal incidence
Mycoplasma: Clinical Manifestations
- Generalized aches and pains
- Fever (usually 102°F)
- Cough (frequently, non-productive)
- Sore throat (nonexudative pharyngitis)
- Headache/myalgias
- Chills, but not rigors
- Nasal congestion with coryza
- Earache
- General malaise
Mycoplasma: Pathogenesis
- Infection involves the trachea, bronchi, and bronchioles (peribronchiolar tissues)
- M. pneumoniae initially attaches to cilia and microvilli of cells lining bronchial epithelium
- Attachment mediated by protrusion associated proteins (e.g., P1, P30); other proteins bind to extracellular matrix (e.g., fibronectin)
- CARDS toxin interferes with ciliary action, leading to nuclear vacuolization and fragmentation of tracheal epithelial cells
- Inflammation and desquamation of affected mucosa
Radiological Presentation
- Variable presentation on CXR; commonly presents as bilateral lower lobe consolidation with small pleural effusions
- Initially, as partly mottled, partly node-like peribronchial opacities with gradual development to involve whole segments or lobes
Mycoplasma: Immunity
- Incomplete immunity
- Re-infection may occur
- Clinical presentation appears more severe in older children
- Many clinical manifestations likely caused by immune response; not due to organism invasion
Urethritis
- Half of urethral infections are not caused by Chlamydia or N. gonorrhoeae
- Causes: Mycoplasma hominis and Ureaplasma
- Diagnosis through culturing (fried egg colonies on medium containing sterols), serology (complement fixation tests, hemagglutination)
Laboratory Diagnosis (Mycoplasma)
- Culture techniques: Mycoplasma from specimen (sputum, mucous membrane) inoculated in liquid/solid media with serum, yeast extract, and penicillin to inhibit contaminating bacteria
- Cultural Characteristics: Lack a cell wall, but grow on solid media as small, transparent colonies (fried-egg appearance). Growth period; 2 days-several weeks
Serology Diagnosis (Mycoplasma)
- Complement fixation
- Hemagglutination (cold agglutinin test, positive for M. pneumoniae (Primary Atypical) Pneumonia; agglutination of human O group erythrocytes at 4°C, reversible at 37°C.
- Hemabsorption & B-hemolysis of guinea pig red blood cells
Identification (Mycoplasma)
- Conclusive identification through staining colonies with fluorescein-labeled antibody
Mycoplasma Nucleic Acid Probes
- Specific recombinants to oligonucleotide sequences found exclusively in M. pneumoniae
L-forms
- Some bacteria readily form variants that can replicate as filterable protoplasmic elements lacking a cell wall– called L-forms
- L-forms formation may occur when cell wall synthesis is impaired by antibiotic treatment or high salt concentration.
L-Forms vs Mycoplasma
- L-Forms: Contain a rigid cell wall at least at one stage in life cycle; lack sterols in cytoplasmic membrane
- Mycoplasma: No cell wall; contain sterols in cytoplasm membrane
Pleuropneumonia-like organisms (PPLO)
- Many organisms with similar morphological characteristics and cultural properties
- Common reference: As PPLO.
- A group of Mycoplasmas create extremely small colonies (T-strains) on agar plates
Multiplication (Mycoplasma)
- Replication pattern differs due to the absence of a rigid cell wall; replication of typical bacteria starts with formation of a well-defined septum
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.