Podcast
Questions and Answers
What is the difference between the cell wall of Chlamydia and a typical Gram-negative bacterium?
What is the difference between the cell wall of Chlamydia and a typical Gram-negative bacterium?
- Chlamydia has a different inner membrane structure
- Chlamydia has an outer membrane only
- Chlamydia has a thicker peptidoglycan layer
- Chlamydia lacks a peptidoglycan layer (correct)
Why is azithromycin the drug of choice for treating Chlamydia genital infections?
Why is azithromycin the drug of choice for treating Chlamydia genital infections?
- It inhibits the synthesis of peptidoglycan
- It is not affected by the lack of peptidoglycan and penicillin-binding proteins (correct)
- It targets the bacterial cell wall
- It inhibits protein synthesis in Chlamydia
What is the characteristic of Chlamydia growth in a cell culture?
What is the characteristic of Chlamydia growth in a cell culture?
- It forms colonies on a plate
- It can be grown in a typical bacterial culture medium
- It grows in a reticulate body structure (correct)
- It is visible to the naked eye
Why are molecular tests preferred for diagnosing Chlamydia infections?
Why are molecular tests preferred for diagnosing Chlamydia infections?
What is the characteristic of Chlamydia genital infections in women?
What is the characteristic of Chlamydia genital infections in women?
What is the reason for reviewing the choice of molecular target for Chlamydia testing?
What is the reason for reviewing the choice of molecular target for Chlamydia testing?
What is the primary reason why Chlamydia cannot be grown on a plate?
What is the primary reason why Chlamydia cannot be grown on a plate?
What is the significance of the reticulate bodies in a cell culture?
What is the significance of the reticulate bodies in a cell culture?
Why does Chlamydia not stain with Gram stain despite being Gram-negative?
Why does Chlamydia not stain with Gram stain despite being Gram-negative?
What is the primary difference between Chlamydia and gonorrhoea genital infections?
What is the primary difference between Chlamydia and gonorrhoea genital infections?
Why are two drugs used to treat both gonorrhoea and Chlamydia?
Why are two drugs used to treat both gonorrhoea and Chlamydia?
What is the primary reason for reviewing the choice of molecular target for Chlamydia testing?
What is the primary reason for reviewing the choice of molecular target for Chlamydia testing?
Flashcards are hidden until you start studying
Study Notes
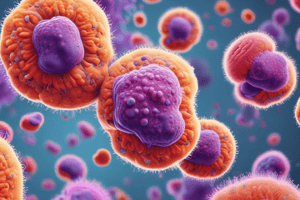
Chlamydia and Gonorrhoea
- Chlamydia is an intracellular bacteria, whereas Gonorrhoea is non-intracellular but becomes intracellular to avoid the immune system.
- Chlamydia cannot be grown on a plate, but can be cultured in cell culture, similar to a virus.
- Chlamydia has a typical Gram-negative cell wall with an inner membrane and outer membrane, but lacks peptidoglycan, which is important for the Gram stain reaction.
- Chlamydia infection is similar to Gonorrhoea, but lacks purulent material and instead presents with mucoid discharge.
- Symptoms of Chlamydia infection include little to no symptoms, but can cause mild inflammation in the cervix, conjunctions, and follicular symptoms (feeling like sand in the eye).
Treatment and Testing
- Azithromycin is the drug of choice for treating Chlamydia and Gonorrhoea infections.
- Penicillin binding proteins are lacking in Chlamydia, making beta-lactam antibiotics ineffective.
- Molecular testing is the preferred method for diagnosing Chlamydia, as it requires cells for growth.
- Testing can be performed on First void urine samples, but the choice of molecular target needs to be reviewed as mutant strains may result in negative molecular tests.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.