Podcast
Questions and Answers
What is the hallmark morphological finding in microangiopathic hemolytic anemia (MAHA)?
What is the hallmark morphological finding in microangiopathic hemolytic anemia (MAHA)?
- Schistocytes (correct)
- Target cells
- Teardrop cells
- Spherocytes
Which of the following laboratory findings would NOT be expected in a patient with microangiopathic hemolytic anemia (MAHA)?
Which of the following laboratory findings would NOT be expected in a patient with microangiopathic hemolytic anemia (MAHA)?
- Decreased hemoglobin levels
- Elevated serum haptoglobin (correct)
- Increased reticulocyte count
- Elevated serum indirect bilirubin
Which of the following conditions is NOT commonly associated with microangiopathic hemolytic anemia (MAHA)?
Which of the following conditions is NOT commonly associated with microangiopathic hemolytic anemia (MAHA)?
- Hemolytic uremic syndrome (HUS)
- Iron deficiency anemia (correct)
- Disseminated intravascular coagulation (DIC)
- Thrombotic thrombocytopenic purpura (TTP)
In thrombotic thrombocytopenic purpura (TTP), a deficiency in which enzyme is a key pathophysiological factor?
In thrombotic thrombocytopenic purpura (TTP), a deficiency in which enzyme is a key pathophysiological factor?
Which of the following distinguishes hemolytic uremic syndrome (HUS) from thrombotic thrombocytopenic purpura (TTP)?
Which of the following distinguishes hemolytic uremic syndrome (HUS) from thrombotic thrombocytopenic purpura (TTP)?
HELLP syndrome is a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and what other finding?
HELLP syndrome is a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and what other finding?
Which of the following coagulation test results is most indicative of disseminated intravascular coagulation (DIC)?
Which of the following coagulation test results is most indicative of disseminated intravascular coagulation (DIC)?
What is the primary mechanism of red blood cell destruction in traumatic cardiac hemolytic anemia?
What is the primary mechanism of red blood cell destruction in traumatic cardiac hemolytic anemia?
In exercise-induced hemoglobinuria, what is the main cause of red blood cell lysis?
In exercise-induced hemoglobinuria, what is the main cause of red blood cell lysis?
Which of the following red blood cell morphologies is typically ABSENT in exercise-induced hemoglobinuria?
Which of the following red blood cell morphologies is typically ABSENT in exercise-induced hemoglobinuria?
During which stage of the Plasmodium life cycle does the parasite multiply in liver cells?
During which stage of the Plasmodium life cycle does the parasite multiply in liver cells?
Which of the following Plasmodium species can infect red blood cells of all ages, contributing to more severe clinical symptoms?
Which of the following Plasmodium species can infect red blood cells of all ages, contributing to more severe clinical symptoms?
What is the primary mechanism by which P. falciparum causes anemia?
What is the primary mechanism by which P. falciparum causes anemia?
In cerebral malaria caused by P. falciparum, what endothelial receptor does PfEMP1 bind to in the brain microvasculature?
In cerebral malaria caused by P. falciparum, what endothelial receptor does PfEMP1 bind to in the brain microvasculature?
Which tick species is the primary vector for transmitting Babesia microti in the United States?
Which tick species is the primary vector for transmitting Babesia microti in the United States?
What is the primary mechanism of hemolysis in clostridial sepsis caused by Clostridium perfringens?
What is the primary mechanism of hemolysis in clostridial sepsis caused by Clostridium perfringens?
Which bacterium is responsible for causing hemolytic anemia through direct adherence to red blood cells in Bartonellosis?
Which bacterium is responsible for causing hemolytic anemia through direct adherence to red blood cells in Bartonellosis?
Dapsone can cause hemolytic anemia via what pathophysiologic mechanism?
Dapsone can cause hemolytic anemia via what pathophysiologic mechanism?
In extensive burns, what is the primary cause of hemolytic anemia?
In extensive burns, what is the primary cause of hemolytic anemia?
What is the significance of elevated lactate dehydrogenase (LDH) in the context of hemolytic anemia?
What is the significance of elevated lactate dehydrogenase (LDH) in the context of hemolytic anemia?
In which of the following conditions is severe ADAMTS13 deficiency most characteristically observed?
In which of the following conditions is severe ADAMTS13 deficiency most characteristically observed?
A patient presents with microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure, following a recent episode of bloody diarrhea. Which condition is most likely?
A patient presents with microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure, following a recent episode of bloody diarrhea. Which condition is most likely?
A pregnant woman in her third trimester presents with right upper quadrant pain, nausea, vomiting, and hypertension. Her laboratory results show hemolysis, elevated liver enzymes, and low platelets. Coagulation tests are normal. Which condition is most likely?
A pregnant woman in her third trimester presents with right upper quadrant pain, nausea, vomiting, and hypertension. Her laboratory results show hemolysis, elevated liver enzymes, and low platelets. Coagulation tests are normal. Which condition is most likely?
What is the primary reason for the absence of protein C activation in patients with cerebral malaria caused by P. falciparum?
What is the primary reason for the absence of protein C activation in patients with cerebral malaria caused by P. falciparum?
Which of the following is LEAST likely to cause a microcytic anemia?
Which of the following is LEAST likely to cause a microcytic anemia?
A patient presents with fatigue, pallor, and dark urine after taking dapsone for a pre-existing condition. Peripheral blood smear shows evidence of hemolysis but no schistocytes. Which of the following is the most likely mechanism of hemolysis?
A patient presents with fatigue, pallor, and dark urine after taking dapsone for a pre-existing condition. Peripheral blood smear shows evidence of hemolysis but no schistocytes. Which of the following is the most likely mechanism of hemolysis?
What virulence mechanism is common to both Clostridium perfringens and Plasmodium falciparum with regard to the development of anemia?
What virulence mechanism is common to both Clostridium perfringens and Plasmodium falciparum with regard to the development of anemia?
Which of the following is the most difficult to treat?
Which of the following is the most difficult to treat?
What shared morphological feature most clearly differentiates traumatic cardiac hemolytic anemia from Bartonellosis?
What shared morphological feature most clearly differentiates traumatic cardiac hemolytic anemia from Bartonellosis?
Flashcards
Extrinsic Hemolytic Anemia
Extrinsic Hemolytic Anemia
Anemia where red blood cells are normal but an external condition causes premature hemolysis.
ADAMTS13
ADAMTS13
Enzyme that regulates the size of von Willebrand factor (VWF) by cleaving ultralong VWF multimers.
Eclampsia
Eclampsia
Life-threatening complication of hypertensive pregnancy disorders causing sudden seizures.
Preeclampsia
Preeclampsia
Signup and view all the flashcards
Microangiopathic Hemolytic Anemia (MAHA)
Microangiopathic Hemolytic Anemia (MAHA)
Signup and view all the flashcards
Schistocytes
Schistocytes
Signup and view all the flashcards
Hemolytic Uremic Syndrome (HUS)
Hemolytic Uremic Syndrome (HUS)
Signup and view all the flashcards
Thrombotic Thrombocytopenic Purpura (TTP)
Thrombotic Thrombocytopenic Purpura (TTP)
Signup and view all the flashcards
HELLP Syndrome
HELLP Syndrome
Signup and view all the flashcards
Disseminated Intravascular Coagulation (DIC)
Disseminated Intravascular Coagulation (DIC)
Signup and view all the flashcards
Traumatic Cardiac Hemolytic Anemia
Traumatic Cardiac Hemolytic Anemia
Signup and view all the flashcards
Exercise-Induced Hemoglobinuria
Exercise-Induced Hemoglobinuria
Signup and view all the flashcards
Sporozoites
Sporozoites
Signup and view all the flashcards
Merozoites
Merozoites
Signup and view all the flashcards
Gametocytes
Gametocytes
Signup and view all the flashcards
Sequestration
Sequestration
Signup and view all the flashcards
Cerebral Malaria
Cerebral Malaria
Signup and view all the flashcards
PfEMP1
PfEMP1
Signup and view all the flashcards
Babesiosis
Babesiosis
Signup and view all the flashcards
Clostridial Sepsis
Clostridial Sepsis
Signup and view all the flashcards
Bartonellosis
Bartonellosis
Signup and view all the flashcards
Drug/Chemical-Induced Hemolysis
Drug/Chemical-Induced Hemolysis
Signup and view all the flashcards
Thermal Injury (Burns)
Thermal Injury (Burns)
Signup and view all the flashcards
Study Notes
- Extrinsic hemolytic anemia occurs when normal red blood cells (RBCs) are prematurely destroyed by conditions outside the RBCs.
- Extrinsic hemolytic anemia is divided into nonimmune and immune causes.
- Nonimmune causes usually involve physical or mechanical injury to RBCs.
- Immune hemolytic anemia is mediated by antibodies, complement, or both.
- ADAMTS13 is an enzyme that regulates the size of von Willebrand factor (VWF) by cleaving ultralong VWF multimers (ULVWF) into shorter segments.
- Eclampsia is a life-threatening pregnancy complication with sudden seizures when no other neurological causes exist.
- Preeclampsia is a pregnancy condition with high blood pressure (hypertension) and high levels of protein in the urine (proteinuria).
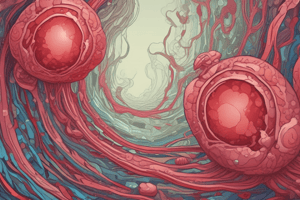
Microangiopathic Hemolytic Anemia (MAHA)
- Microangiopathic Hemolytic Anemia (MAHA) involves RBC fragmentation and thrombocytopenia from mechanical destruction in the vasculature.
- RBCs are fragmented in small blood vessels due to turbulence caused by microthrombi or damaged endothelium.
- Fragmentation creates schistocytes, which are irregularly shaped RBC fragments.
- Fragmented RBCs undergo intravascular hemolysis.
- The spleen clears rigid fragments through extravascular processes.
Clinical Laboratory Findings
- Decreased hemoglobin and hematocrit
- Increased reticulocyte count
- Elevated serum indirect (unconjugated) bilirubin
- Increased lactate dehydrogenase (LD) activity
- Low serum haptoglobin
- Elevated urine urobilinogen
- Presence of schistocytes (RBC fragments) on a peripheral blood smear
- Typically shows thrombocytopenia
MAHA associations
- MAHA is common in thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), and disseminated intravascular coagulation (DIC).
- Urgent intervention is needed to address the underlying cause of MAHA
Thrombotic Thrombocytopenic Purpura
- Thrombotic thrombocytopenic purpura (TTP): Characterized by microangiopathic hemolytic anemia, severe thrombocytopenia, and elevated serum LD activity.
- Pathophysiology: Severe deficiency of ADAMTS13 leads to accumulation of ultra-large von Willebrand factor (ULVWF) multimers, promoting platelet adhesion and microthrombi formation.
- Clinical Symptoms: Abrupt onset of MAHA and thrombocytopenia, potential neurologic dysfunction, fever, and renal failure.
- Laboratory Findings: Anemia, thrombocytopenia, schistocytes on blood smear, reticulocytosis, normal coagulation tests, increased LD and bilirubin, decreased haptoglobin, and varying levels of ADAMTS13 deficiency.
Hemolytic Uremic Syndrome
- Hemolytic uremic syndrome (HUS): Characterized by microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure due to glomerular microvasculature damage.
Pathophysiology
- Thrombocytopenia: Decreased platelet count due to consumption in microthrombi formation.
- Acute Renal Failure: Caused by damage to the glomerular microvasculature in the kidneys
HUS Types:
- Stx-HUS induced by Shiga toxin-producing bacteria (e.g., E. coli O157:H7) following gastroenteritis.
- Atypical HUS (aHUS): Caused by dysregulation of the complement pathway, not linked to diarrhea, and may have genetic or autoimmune origins.
- MAHA, thrombocytopenia, and acute renal failure.
Clinical Features
- Symptoms: Symptoms of MAHA, mild-to-moderate thrombocytopenia, acute renal failure signs (elevated creatinine, proteinuria, hematuria, urinary casts).
Laboratory Findings
- Hemolysis Evidence: Schistocytes, elevated LD and bilirubin, decreased haptoglobin.
- Thrombocytopenia: Platelet count mildly to moderately decreased.
- Renal Dysfunction: Elevated serum creatinine and abnormal urinalysis.
- ADAMTS13 Levels: Normal.
HELLP Syndrome
- HELLP Syndrome is a complication in pregnancy, comprising hemolysis, elevated liver enzymes, and low platelet count, typically in the third trimester.
Pathophysiology
- Endothelial dysfunction, platelet activation, and microvascular injury lead to hemolysis, liver damage, and thrombocytopenia.
- Symptoms: Symptoms of MAHA, right upper quadrant or epigastric pain, nausea, vomiting, headache, hypertension, and proteinuria.
- Laboratory Findings: Thrombocytopenia, anemia with schistocytes, elevated LD and bilirubin, elevated liver enzymes (AST, ALT), and normal coagulation tests.
Disseminated Intravascular Coagulation (DIC)
Pathophysiology
- Widespread activation of the hemostatic system leads to fibrin thrombi formation in the microvasculature and consumption of platelets and coagulation factors.
- Secondary activation of fibrinolysis contributes to bleeding.
Result
- Obstruction of the microvasculature causes organ ischemia.
Clinical Features
- Symptoms: Vary based on dominant process (thrombosis vs. bleeding), organ ischemia, petechiae, ecchymoses, gastrointestinal or mucosal bleeding.
Laboratory Findings
- Decreased platelet count.
- Schistocytes on a peripheral smear (in approximately 50% of cases).
- Prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT).
- Decreased fibrinogen level.
- Elevated D-dimer
Key Diagnostic Differentiators
- DIC is distinguished from other microangiopathies like HELLP syndrome or TTP by certain factors
- Prolonged coagulation times (PT, aPTT).
- Decreased fibrinogen.
- Elevated D-dimer.
- TTP: Distinguished by severe ADAMTS13 deficiency and neurologic symptoms; normal coagulation tests.
- HUS: Primarily involves renal failure, with typical cases often following bloody diarrhea (e.g., Stx-HUS).
- HELLP Syndrome: Occurs exclusively in pregnancy, with unique elevated liver enzymes and normal coagulation studies.
Traumatic Cardiac Hemolytic Anemia
Pathophysiology
- Mechanical hemolysis due to turbulent blood flow through or around prosthetic cardiac valves or damaged cardiac valves.
- RBCs are mechanically fragmented, producing schistocytes.
- Severe hemolysis can occur with paravalvular leaks in prosthetic valves and chronic urinary hemoglobin loss may lead to iron deficiency anemia.
Laboratory Features
- Blood Smear: Presence of schistocytes.
- Hemolysis Markers: Elevated serum lactate dehydrogenase (LD) and indirect bilirubin, increased free plasma hemoglobin, and decreased serum haptoglobin.
- Reticulocyte Count: Elevated.
- Platelet Count: Typically within the reference interval.
Exercise-Induced Hemoglobinuria
Pathophysiology
- Caused by mechanical trauma from repetitive physical impact.
- RBC lysis occurs due to stress on the membrane, oxidative damage, or alterations in cytoskeletal proteins during strenuous exercise.
Laboratory Features
- Hemolysis Markers: Elevated free plasma hemoglobin, decreased serum haptoglobin, and presence of hemoglobinuria after exercise.
- Peripheral Blood Smear: Schistocytes are absent except in rare cases.
- Reticulocyte Count: Slightly increased.
Plasmodium Life Cycle
Mosquito to Human
- An infected Anopheles mosquito bites a human, injecting sporozoites into the bloodstream.
Liver Stage
- Sporozoites travel to the liver and invade liver cells, multiplying into merozoites.
- Liver cells burst, releasing merozoites into the blood.
Blood Stage
- Merozoites infect red blood cells (RBCs).
- Developing through stages: Ring form → Trophozoite → Schizont.
- Schizonts release new merozoites, continuing the infection cycle.
Human to Mosquito
- When another mosquito bites the infected human, it ingests gametocytes.
- Gametocytes develop into gametes in the mosquito, undergo sexual reproduction, and eventually form sporozoites again
Specific Plasmodium
- P. vivax & P. ovale can only invade reticulocytes
- P. malariae can only invade older RBCs
- P. vivax requires Duffy antigens for RBC invasion
- P. falciparum & P. knowlesi can invade cells of all ages
P. falciparum Infection
Anemia
- The adherence of Infected RBCs to endothelial cells in the microvasculature in places such as the liver or spleen.
- Direct destruction of infected RBCs during the parasite's life cycle.
- Inflammation can suppress erythropoiesis in the bone marrow, exacerbating the anemia
- Chronic hemolysis can lead to iron depletion, further contributing to anemia.
Neurologic Manifestations
- Infected RBCs obstructing blood flow occurs
- Binding leads to obstruction of blood flow, disrupting oxygen delivery to brain tissues.
- Inflammatory Response: Cytokine release from endothelial cells and immune cells contributes to local inflammation and endothelial dysfunction.
- Microvascular Obstruction: Leads to cerebral ischemia, edema, and neurologic symptoms such as seizures, confusion, and coma.
Hemolytic Anemia: Pathophysiology, Labs and Morphology
Babesiosis
- Hemolytic anemia caused by Babesia that occurs due to parasitemia, splenic RBC destruction and systemic response.
Clostridial Sepsis
- Caused by Clostridium perfringens, which produces toxins that hydrolyze RBC membrane phospholipids, leading to hemolysis.
- Causes hemolysis and severe anemia occur
Bartonellosis
- Caused by Bartonella bacilliformis, which adheres to RBCs, leading to destruction.
- Progresses in two stages: acute hemolysis and Verruga Peruana (chronic cutaneous lesions).
Drugs, Chemicals, and Venoms
- Drugs, chemicals, and venoms can either disrupt the RBC membrane, trigger complement-mediated lysis, or initiate DIC, leading to hemolysis.
Thermal Injury (Burns)
- Extensive burns cause direct thermal damage to RBC membranes, leading to hemolysis.
- Elevated hemolysis markers (e.g., LDH, bilirubin).
- Hemoglobinuria and darkened urine may be observed in severe cases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.