Podcast
Questions and Answers
Medullary thyroid cancer (MTC) originates from which type of thyroid cell?
Medullary thyroid cancer (MTC) originates from which type of thyroid cell?
- Oxyphil cells
- Hurthle cells
- Follicular cells
- Parafollicular C cells (correct)
Which biochemical marker is highly sensitive for MTC and correlates with tumor burden?
Which biochemical marker is highly sensitive for MTC and correlates with tumor burden?
- Thyroxine (T4)
- Thyroglobulin
- Triiodothyronine (T3)
- Calcitonin (correct)
What genetic mutation is commonly associated with MTC?
What genetic mutation is commonly associated with MTC?
- RET proto-oncogene (correct)
- KRAS
- EGFR
- BRAF
What is the standard surgical treatment for localized MTC?
What is the standard surgical treatment for localized MTC?
Which of the following is a common site for MTC metastasis?
Which of the following is a common site for MTC metastasis?
In the context of MTC, what does MEN stand for?
In the context of MTC, what does MEN stand for?
Which imaging technique is typically the first-line for evaluating thyroid nodules?
Which imaging technique is typically the first-line for evaluating thyroid nodules?
What symptom is associated with increased calcitonin secretion due to MTC?
What symptom is associated with increased calcitonin secretion due to MTC?
Flashcards
Annual screening
Annual screening
Includes neck ultrasound, serum calcitonin, and CEA levels for cancer monitoring.
Prognosis of MTC
Prognosis of MTC
10-year survival for sporadic MTC is around 75%, worse in familial cases.
MEN 2A
MEN 2A
Classical variant of MEN 2, characterized by 100% MTC, ~50% pheochromocytoma, and primary hyperparathyroidism.
MEN 2B
MEN 2B
Signup and view all the flashcards
RET mutations
RET mutations
Signup and view all the flashcards
Medullary Thyroid Cancer (MTC)
Medullary Thyroid Cancer (MTC)
Signup and view all the flashcards
Sporadic MTC
Sporadic MTC
Signup and view all the flashcards
Familial MTC
Familial MTC
Signup and view all the flashcards
RET proto-oncogene
RET proto-oncogene
Signup and view all the flashcards
Calcitonin as a marker
Calcitonin as a marker
Signup and view all the flashcards
Total thyroidectomy
Total thyroidectomy
Signup and view all the flashcards
Tyrosine Kinase Inhibitors (TKIs)
Tyrosine Kinase Inhibitors (TKIs)
Signup and view all the flashcards
Symptoms of MTC
Symptoms of MTC
Signup and view all the flashcards
Study Notes
Medullary Thyroid Cancer (MTC)
- MTC is a neuroendocrine tumor originating from C cells in the thyroid, producing calcitonin. Unlike other thyroid cancers, it's more aggressive.
- It occurs sporadically in about 75% of cases, or as part of familial syndromes like MEN 2A and 2B.
- Originates from neural crest-derived C cells producing calcitonin, which serves as a tumor marker.
- Associated with RET proto-oncogene mutations.
- Metastasizes commonly to cervical and mediastinal lymph nodes, lungs, liver, and bones.
- Typical presentation includes a neck mass (often firm and painless), dysphagia (difficulty swallowing), hoarseness, diarrhea (due to calcitonin), flushing (due to vasoactive peptides), and potential endocrine symptoms.
- MEN 2A can present with hyperparathyroidism and pheochromocytoma, while MEN 2B includes marfanoid habitus, mucosal neuromas, and pheochromocytoma.
Diagnostic Evaluation of MTC
- Biochemical Markers: Serum calcitonin (highly sensitive, correlating with tumor burden), carcinoembryonic antigen (CEA) often elevated in advanced disease, RET proto-oncogene mutation testing is crucial for hereditary cases.
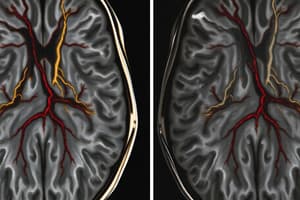
- Imaging: Thyroid ultrasound (first-line), fine-needle aspiration (FNA) with calcitonin staining for confirmation, CT/MRI for metastases (especially for suspected widespread disease), PET-CT (advanced cases), and MIBG/Octreotide scan (other neuroendocrine tumors).
Management of MTC
- Surgical Treatment (Localized): Total thyroidectomy with central lymph node dissection standard. Prophylactic thyroidectomy in MEN2. Lateral neck dissection for positive nodes.
- Adjuvant Treatment (Metastatic/Advanced): Targeted therapy (tyrosine kinase inhibitors like cabozantinib/vandetinib for progressive disease), radiation therapy (palliation for unresectable/metastatic), calcitonin monitoring post-surgery (residual/recurrence), and annual screening (neck ultrasound, serum calcitonin, CEA).
Prognosis of MTC
- Sporadic MTC: ~75% 10-year survival.
- Familial MTC (MEN 2A/2B): Poorer prognosis for MEN 2B (early onset, aggressive).
- Prognosis dependent on stage: Localized disease (good) vs. metastatic disease (poor).
Multiple Endocrine Neoplasia (MEN)
- MEN syndromes are autosomal dominant disorders of genes controlling cell growth in multiple endocrine organs.
MEN 2 (RET-Related)
- MTC is the hallmark of MEN 2.
MEN 2A
- MTC (100%)
- Pheochromocytoma (~50%): Potentially life-threatening hypertension.
- Primary hyperparathyroidism (~20-30%): Often parathyroid hyperplasia.
- RET mutations in specific exons (10, 11, 13, 14, 15, 16).
MEN 2B
- MTC (aggressive, early-onset, 100%)
- Pheochromocytoma (~50%)
- Marfanoid habitus, mucosal neuromas (lips, tongue, eyelids, GI).
- No hyperparathyroidism.
- RET mutations (exons 15, 16), M918T mutation associated with worse prognosis.
- Prophylactic thyroidectomy at a young age.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.