Podcast
Questions and Answers
What is a common consequence of dysphagia?
What is a common consequence of dysphagia?
- Decreased food availability
- Improved immune function
- Increased hydration
- Significant weight loss (correct)
Which factor can contribute to the development of esophageal disorders?
Which factor can contribute to the development of esophageal disorders?
- Regular meals
- Balanced diet
- Derangement of the swallowing mechanism (correct)
- Consistent hydration
What is the primary aim in managing dysphagia?
What is the primary aim in managing dysphagia?
- Ordering extensive diagnostic tests
- Encouraging a high-fiber diet
- Assessing the nature of the swallowing problem (correct)
- Utilizing nutritional supplements only
Which of the following is a major gastrointestinal condition?
Which of the following is a major gastrointestinal condition?
What can lead to acute esophagitis?
What can lead to acute esophagitis?
What is a potential result of gastrointestinal disorders related to malabsorption?
What is a potential result of gastrointestinal disorders related to malabsorption?
Which of the following is NOT classified as a disorder of the esophagus?
Which of the following is NOT classified as a disorder of the esophagus?
What is a common treatment goal for managing patients with esophagitis?
What is a common treatment goal for managing patients with esophagitis?
Which dietary recommendation is NOT appropriate for someone with acute esophagitis?
Which dietary recommendation is NOT appropriate for someone with acute esophagitis?
What is a common symptom of Gastroesophageal Reflux Disorder (GERD)?
What is a common symptom of Gastroesophageal Reflux Disorder (GERD)?
Which factor is NOT a known cause of GERD?
Which factor is NOT a known cause of GERD?
Which of the following complications can arise from prolonged GERD?
Which of the following complications can arise from prolonged GERD?
What is one objective of nutritional care for patients with GERD?
What is one objective of nutritional care for patients with GERD?
Which dietary change is recommended for managing GERD?
Which dietary change is recommended for managing GERD?
What lifestyle change could potentially worsen GERD symptoms?
What lifestyle change could potentially worsen GERD symptoms?
Which of the following foods should be avoided by someone suffering from esophagitis?
Which of the following foods should be avoided by someone suffering from esophagitis?
Flashcards
Dysphagia
Dysphagia
Difficulty swallowing. Often leads to reduced food intake.
Esophagitis
Esophagitis
Inflammation of the esophagus. Can be caused by caustic substances or repeated vomiting.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD)
A condition characterized by the backward flow of stomach acid into the esophagus.
Hiatal hernia
Hiatal hernia
Signup and view all the flashcards
Malabsorption
Malabsorption
Signup and view all the flashcards
GI Disorders
GI Disorders
Signup and view all the flashcards
Upper GI Disorders
Upper GI Disorders
Signup and view all the flashcards
Lower GI Disorders
Lower GI Disorders
Signup and view all the flashcards
GERD
GERD
Signup and view all the flashcards
GERD Symptoms
GERD Symptoms
Signup and view all the flashcards
GERD Causes
GERD Causes
Signup and view all the flashcards
GERD Complications
GERD Complications
Signup and view all the flashcards
GERD Treatment: Diet
GERD Treatment: Diet
Signup and view all the flashcards
GERD Nutritional Goals
GERD Nutritional Goals
Signup and view all the flashcards
GERD Impact
GERD Impact
Signup and view all the flashcards
Study Notes
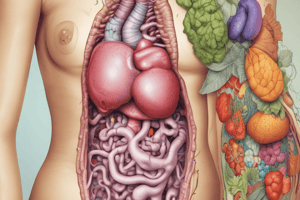
Medical Therapeutic Nutrition 1: Nutritional Management of Gastrointestinal Disorders
- GI Disorders Effects: Malabsorption, discomfort with eating, anorexia, impaired intake, and food intolerances.
Major GI Tract Conditions
- Upper GI: Diarrhea, vomiting, dyspepsia (gastric indigestion), peptic and duodenal ulcers, constipation, abdominal pain, irritable bowel, hemorrhoids, anal fissure, dysphagia, hernia.
- Additional Upper GI conditions: Gallstones, appendicitis, malabsorption syndromes.
- Lower GI conditions: Ulcerative colitis, Crohn's disease, diverticular disease of the colon, diverticulitis, pancreatitis, and liver disease.
- Additional lower GI conditions: Food intolerance.
Disorders of the Esophagus
- E-sophagus: The tube connecting the pharynx to the stomach.
- Disorders: Dysphagia, Esophagitis, Gastroesophageal Reflux (GERD), Hiatal Hernia.
- Causes of Esophageal Disorders: Derangement of swallowing mechanism, obstruction, inflammation, or abnormal sphincter function.
- Dysphagia (CONT): Almost always accompanied by reduced food intake, leading to significant weight loss, compromised immune function, and high risk of dehydration.
Primary Aims of Dysphagia Management
- Assess: The swallowing problem.
- Determine: A safe and adequate feeding route.
- Determine: Appropriate food and fluid texture/consistency.
- Meet: Nutritional needs.
- Ensure: Adequate hydration status.
- Educate: Patient/caretakers.
- Monitor: Progress and ensure continuity of care.
Esophagitis (CONT)
- Causes: Ingesting caustic compounds (often medications like NSAIDs), repeated vomiting (especially self-induced in anorexia/bulimia).
Dietary Recommendations for Acute Esophagitis
- Avoid: Spicy foods (red/black pepper).
- Follow: A bland, soft diet.
- Eat: Small frequent meals.
- Severe: Esophagitis - low-fat liquid diet.
- Avoid: Acidic foods (citrus fruits, soft drinks, tomato) - can cause pain if esophagus is inflamed.
Gastroesophageal Reflux Disorders (GERD)
- Definition: Symptoms of mucosal damage produced by abnormal reflux of gastric contents into the esophagus. (Acid from stomach refluxes up into the esophagus).
- Symptoms: Burning sensation after meals, heartburn, regurgitation, symptoms are aggravated by recumbency/bending over, and relieved by antacids.
- Chronic GERD Symptoms: Substernal pain, belching, esophageal spasm.
Causes of GERD
- Esophageal sphincter weakness.
- Increased pressure within the stomach.
- High pressure from abdominal area (obesity/pregnancy)
- Hiatus hernia.
- Tobacco use.
- Delayed gastric emptying.
- Recurrent vomiting.
Complications of GERD
- Prolonged reflux can result in esophagitis (inflammation), esophageal ulceration, scarring, esophageal strictures, and dysphagia..
- GERD is distressing and its symptoms interfere with sleep, work, and overall quality of life.
- Prolonged/severe reflux can affect esophageal tissues and potentially lead to cancer.
Treatment and Nutritional Intervention of GERD
- Objectives: Prevent esophageal reflux, prevent pain and irritation of inflamed esophageal mucosa, decrease erosive capacity/acidity of gastric secretions.
Dietary Changes to Manage GERD
- Avoid eating several hours before sleep (late at night).
- Avoid large meals, especially desserts high in fat and protein (stimulates acid secretion, slows gastric emptying).
- Eat small frequent meals.
- Avoid drinking liquids with meals; drink between meals.
- Avoid lying down, lifting after large meals.
- Avoid highly spiced foods when inflammation exists.
- Avoid foods/drugs that lower pressure of LES (Dietary fat, alcohol, carminatives).
- Avoid foods that increase gastric acidity (black/red pepper, coffee, alcohol).
- Reduce weight if overweight.
Hiatus Hernia
- Diet therapy: aimed at decreasing symptoms (reflux/esophagitis) in people with reflux.
- Therapy: Similar to GERD and esophagitis.
- Dietary Management: Smaller low-fat meals, avoiding foods that increase gastric secretions.
- Surgery: Not always indicated, medication often controls symptoms.
- Preferred treatment: Diet.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.