Podcast
Questions and Answers
Which of the following factors does NOT directly influence the energy manifested on the vessel wall due to the heart's pumping action?
Which of the following factors does NOT directly influence the energy manifested on the vessel wall due to the heart's pumping action?
- Shear stress
- Vessel diameter (correct)
- Tensile stress
- Blood pressure
Which statement accurately describes the relationship between blood vessel radius and resistance to blood flow, as described by the Poiseuille law?
Which statement accurately describes the relationship between blood vessel radius and resistance to blood flow, as described by the Poiseuille law?
- Resistance is directly proportional to the radius.
- Resistance is directly proportional to the fourth power of the radius.
- Resistance is inversely proportional to the square of the radius.
- Resistance is inversely proportional to the fourth power of the radius. (correct)
In the context of vascular physiology, what is the primary factor influencing the regulation of vascular resistance, particularly in arterioles?
In the context of vascular physiology, what is the primary factor influencing the regulation of vascular resistance, particularly in arterioles?
- Blood pressure
- Vessel radius (correct)
- Blood viscosity
- Vessel length
How does polycythemia affect blood flow, according to its influence on hematocrit value?
How does polycythemia affect blood flow, according to its influence on hematocrit value?
What effect do plasma proteins, specifically immunoglobulins, have on blood flow?
What effect do plasma proteins, specifically immunoglobulins, have on blood flow?
Turbulent blood flow is characterized by which of the following?
Turbulent blood flow is characterized by which of the following?
Which condition is most likely to cause a change from laminar to turbulent blood flow?
Which condition is most likely to cause a change from laminar to turbulent blood flow?
What is the effect of decreased arterial compliance on pulse pressure, assuming stroke volume remains constant?
What is the effect of decreased arterial compliance on pulse pressure, assuming stroke volume remains constant?
When arterial compliance is low, how does this affect cardiac work for the same cardiac output (CO)?
When arterial compliance is low, how does this affect cardiac work for the same cardiac output (CO)?
Compared to arteries, veins are known to be how many times more compliant?
Compared to arteries, veins are known to be how many times more compliant?
What happens to venous compliance when venous tone increases due to sympathetic stimulation?
What happens to venous compliance when venous tone increases due to sympathetic stimulation?
What is the effect of increased wall tension on distending pressure in a thin-walled viscus, according to the Law of Laplace?
What is the effect of increased wall tension on distending pressure in a thin-walled viscus, according to the Law of Laplace?
According to the Law of Laplace, how can thin-walled capillaries withstand high pressures?
According to the Law of Laplace, how can thin-walled capillaries withstand high pressures?
What is the most accurate calculation of Mean Arterial Pressure (MAP)?
What is the most accurate calculation of Mean Arterial Pressure (MAP)?
How does an increase in heart rate affect diastolic time and, subsequently, mean arterial pressure (MAP)?
How does an increase in heart rate affect diastolic time and, subsequently, mean arterial pressure (MAP)?
What is the effect of increased stroke volume on arterial blood pressure?
What is the effect of increased stroke volume on arterial blood pressure?
How does atherosclerosis-induced decreased arterial compliance affect systolic and diastolic blood pressure?
How does atherosclerosis-induced decreased arterial compliance affect systolic and diastolic blood pressure?
How does age-related loss of elasticity in blood vessels affect arterial blood pressure (ABP)?
How does age-related loss of elasticity in blood vessels affect arterial blood pressure (ABP)?
How does the effect of gravity change the ABP while standing, for every 1 cm below the heart?
How does the effect of gravity change the ABP while standing, for every 1 cm below the heart?
Which of the following best describes the 'Traube-Hering waves'?
Which of the following best describes the 'Traube-Hering waves'?
What is the primary function of veins related to blood volume?
What is the primary function of veins related to blood volume?
Which of the following parameters has a normal value of 0-2 mm Hg?
Which of the following parameters has a normal value of 0-2 mm Hg?
What is most likely indicated by decreased Central Venous Pressure (CVP)?
What is most likely indicated by decreased Central Venous Pressure (CVP)?
What is the effect of gravity on venous pressure in the head veins when standing?
What is the effect of gravity on venous pressure in the head veins when standing?
In the context of venous return, what does the 'pressure gradient for venous return' refer to?
In the context of venous return, what does the 'pressure gradient for venous return' refer to?
What happens to venous return when right atrial pressure (RAP) equals mean systemic filling pressure (MSFP)?
What happens to venous return when right atrial pressure (RAP) equals mean systemic filling pressure (MSFP)?
What is the effect of venoconstriction, caused by sympathetic stimulation, on mean systemic filling pressure (MSFP)?
What is the effect of venoconstriction, caused by sympathetic stimulation, on mean systemic filling pressure (MSFP)?
How do the muscular pump and thoracic pump mechanisms aid venous return?
How do the muscular pump and thoracic pump mechanisms aid venous return?
What characterizes 'point A' under steady-state conditions in the interaction between cardiac factors and peripheral vascular factors in the control of cardiac output?
What characterizes 'point A' under steady-state conditions in the interaction between cardiac factors and peripheral vascular factors in the control of cardiac output?
During muscular exercise, what is the initial effect of sympathetic stimulation on the heart rate?
During muscular exercise, what is the initial effect of sympathetic stimulation on the heart rate?
What directly causes the shift of the venous return curve 'up and to the right' during exercise?
What directly causes the shift of the venous return curve 'up and to the right' during exercise?
What is the primary function of ISF in the capillaries?
What is the primary function of ISF in the capillaries?
What is the cause of intermittent capillary blood flow?
What is the cause of intermittent capillary blood flow?
According to Starling forces, what happens at the arteriolar end of a muscle capillary?
According to Starling forces, what happens at the arteriolar end of a muscle capillary?
What is the primary mechanism that helps lymphatic drainage?
What is the primary mechanism that helps lymphatic drainage?
Which of the following reactions, when stroking the skin lightly, indicates the contraction of precapillary sphincters, resulting in empty capillaries?
Which of the following reactions, when stroking the skin lightly, indicates the contraction of precapillary sphincters, resulting in empty capillaries?
According to the material, what is the direct effect of low blood pH (acidosis) on arteriolar smooth muscles in working tissues?
According to the material, what is the direct effect of low blood pH (acidosis) on arteriolar smooth muscles in working tissues?
What role does nitric oxide (NO) play in vascular smooth muscle cells?
What role does nitric oxide (NO) play in vascular smooth muscle cells?
Which of the following conditions is associated with a deficiency in nitric oxide (NO) production?
Which of the following conditions is associated with a deficiency in nitric oxide (NO) production?
Endothelin-1 secretion is increased by all of the following stimuli EXCEPT:
Endothelin-1 secretion is increased by all of the following stimuli EXCEPT:
The activation of β2 receptors in blood vessels of skeletal muscles by circulating catecholamines results in:
The activation of β2 receptors in blood vessels of skeletal muscles by circulating catecholamines results in:
What is the effect of increased levels of the natriuretic peptide hormones on blood volume and blood pressure?
What is the effect of increased levels of the natriuretic peptide hormones on blood volume and blood pressure?
Plasma kallikrein is activated by active factor XIIa where?
Plasma kallikrein is activated by active factor XIIa where?
If cerebral ischemia and fainting occur, and a treatment plan includes 'implantation of permanent artificial cardiac pacemaker', which syndrome is more more likely present?
If cerebral ischemia and fainting occur, and a treatment plan includes 'implantation of permanent artificial cardiac pacemaker', which syndrome is more more likely present?
Flashcards
Blood Pressure
Blood Pressure
Force per unit area exerted perpendicular to a surface; measured in mm Hg; tends to distend the blood vessel.
Tensile Stress
Tensile Stress
Force per unit area, a circumferential force resulting from attractions between molecules in the vessel wall, counterbalancing the distending effect of pressure.
Shear Stress
Shear Stress
Tangential drag force produced by blood moving across the endothelial surface, about 20-40 dyne/cm² in large arteries which induce changes in gene expression.
Poiseuille's Law
Poiseuille's Law
Signup and view all the flashcards
Effect of radius
Effect of radius
Signup and view all the flashcards
Vascular Compliance
Vascular Compliance
Signup and view all the flashcards
Arterial Compliance
Arterial Compliance
Signup and view all the flashcards
Venous Compliance
Venous Compliance
Signup and view all the flashcards
Law of LaPlace
Law of LaPlace
Signup and view all the flashcards
Systolic Pressure
Systolic Pressure
Signup and view all the flashcards
Diastolic Pressure
Diastolic Pressure
Signup and view all the flashcards
Mean Arterial Pressure (MAP)
Mean Arterial Pressure (MAP)
Signup and view all the flashcards
Factors Determining ABP
Factors Determining ABP
Signup and view all the flashcards
Central Venous Pressure (CVP)
Central Venous Pressure (CVP)
Signup and view all the flashcards
Venous Return
Venous Return
Signup and view all the flashcards
Mean Systemic Filling Pressure (MSFP)
Mean Systemic Filling Pressure (MSFP)
Signup and view all the flashcards
Muscle Pump
Muscle Pump
Signup and view all the flashcards
Point A
Point A
Signup and view all the flashcards
Autoregulation
Autoregulation
Signup and view all the flashcards
Myogenic Autoregulation
Myogenic Autoregulation
Signup and view all the flashcards
Vasomotion Cycle
Vasomotion Cycle
Signup and view all the flashcards
Nitric Oxide (NO)
Nitric Oxide (NO)
Signup and view all the flashcards
Endothelin-1
Endothelin-1
Signup and view all the flashcards
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Atrial natriuretic peptide (ANP)
Atrial natriuretic peptide (ANP)
Signup and view all the flashcards
Vasomotor Area
Vasomotor Area
Signup and view all the flashcards
Arterial Baroreceptors
Arterial Baroreceptors
Signup and view all the flashcards
Baroreceptor Reflex
Baroreceptor Reflex
Signup and view all the flashcards
Normal Vasomotor Oscillations of ABP
Normal Vasomotor Oscillations of ABP
Signup and view all the flashcards
Shivering reflex
Shivering reflex
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Circulatory Shock
Circulatory Shock
Signup and view all the flashcards
Compensatory mechanisms to hemorrhage *
Compensatory mechanisms to hemorrhage *
Signup and view all the flashcards
Hypovolemic shock
Hypovolemic shock
Signup and view all the flashcards
Neurogenic shock
Neurogenic shock
Signup and view all the flashcards
Study Notes
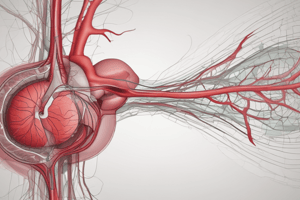
- Vascular medicine is the study of blood vessels and how they work.
Mechanical Forces Acting on Blood Vessel
- Energy from the hearts pumping action is on the vessel wall in 3 forms.
- Blood pressure is the force per unit area, in a direction perpendicular to the surface.
- The force tends to distend the blood vessel and is measured in mm Hg.
- 1 mm Hg is equal to 0.133 kPa, and Pascal (Pa) is Newton/m².
- Tensile stress is force per unit area (Newton/m2), resulting from attraction between molecules in the vessel wall.
- This counterbalances the distending effect of pressure.
- Shear stress is tangential drag force made by blood moving across the endothelial surface.
- The shear stress is 20-40 dyne/cm² in large arteries.
- Over extended time, changes in shear stress produce marked changes in gene expression in endothelial cells.
- Endothelial cells and extra-cellular matrix (ECM) transmit pressure and shear stress to regulate the function of vascular smooth muscle cells through changing gene expression.
Poiseuille Law: Vascular Resistance
- States the relation between flow in a tube (F), viscosity of the fluid (n), length of the tube (L), and radius (r).
- Flow (amount of blood flow crossing the ventricle/unit time) is the same as cardiac output, which amounts to blood pumped into the aorta/minute.
- Flow is directly proportional to effective perfusion pressure/“pressure gradient (ΔΡ)” (P₁ — Р2).
- Flow is inversely proportional to resistance of the vessel to blood flow (R), with the relation F=ΔP÷R
- Resistance to blood flow depends on vessel radius (r), blood viscosity (n), and vessel length (L).
- Radius has the relation R ∝ 1/r⁴.
- Viscosity has a relation R ∝ n.
- Length has the relation R∝L.
- Radius, mainly in arterioles, dictates regulation of resistance.
- A 20% increase in radius leads to a 50% decrease in resistance, while flow is doubled.
- Viscosity relies mainly on hematocrit value.
- Polycythemia causes increase in hematocrit and in resistance to blood flow.
- The increase in plasma proteins, such as immunoglobulins, has a minor effect on viscosity and blood flow.
- Elasticity of blood vessels has effect on pressure, increased pressure distends vessel, increases radius, and decreases resistance.
- The same pressure gradient results in higher flow in elastic vessels than rigid ones.
- Total peripheral resistance (TPR) in systemic circulation calculates as CO = [mean arterial pressure (MAP) - right atrial pressure or central venous pressure (CVP)]/TPR.
- TPR is derived from the formula TPR = MAP – CVP / CO = (90 – 0) / 5 = 18 mmHg/L/min.
- Resistance of pulmonary circulation (PulR) calculates as PulR = [mean pulmonary pressure (MPP)- left atrial pressure (LAP)]/COP = (15 – 8) / 5 = 1.4 mmHg/L/min.
Velocity of Blood Flow
- Velocity is inversely proportional to vascular cross-sectional area.
- The aorta cross-sectional area is 2.5 cm², with a velocity of 0.5 m/sec.
- Total cross-sectional area of capillaries is 2500 cm² (1000 times that of the aorta), with a velocity = 0.5 mm/sec (1/1000 of that of the aorta).
Types of Blood Flow Inside Vessels
- Two types of blood flow inside the vessels include laminar and turbulent.
- Laminar (streamline) flow is a normal flow in vessels, occurring in layers and is silent.
- Velocity is stationary in the thin layer of blood in contact with the wall and is highest at the center of the vessel.
- Turbulent flow is flow in varying directions, resulting in eddy currents and sound (murmurs), it has a greater resistance than laminar flow.
- Laminar flow changes to turbulent flow when:
- There is increased blood flow to a certain critical velocity.
- The blood has decreased viscosity (anemia).
- There is sudden change in vessel diameter.
- The flow makes sharp turn in direction.
- The blood passes over the rough area of the blood vessel.
Vascular Compliance
- C = ΔV/ΔP, representing the ratio between change in blood volume and in pressure.
- Is depicted by the graph slope, compliance is higher at lower volumes and vessels become stiffer and harder to distend at higher values of volume.
- Total systemic arterial compliance is dictated by the aorta and major branches.
- Decreased arterial compliance due to increased sympathetic tone or atherosclerosis which increases the change of pressure for same arterial blood volume..
- Arterial compliance:
- Converts intermittent flow in the aorta to continuous flow in peripheral vessels.
- Recoil of arteries during diastole pushes blood forward.
- Minimizes increase in systolic pressure and decrease in diastolic pressure.
- Cardiac work = pressure x volume.
- Low compliance requires greater pressure and work for the same volume (CO).
Venous Compliance
- Veins are 24 times compliant as arteries.
- Allows accommodation of greater volumes versus arteries for the same pressure, or reservoir vessels.
- Volume and pressure relate as veins are normally partially collapsed at low volumes.
- In this state, large increases in volume result in very little increase in pressure and very high compliance.
- Veins turn cylindrical without stretching their walls.
- At higher volume, further volume increases result in marked pressure increases and low compliance.
- Venous compliance is dictated by venous tone.
- Increased venous tone (sympathetic) decreases venous compliance, shifting the volume/pressure relationship down and to the right.
- 84% of blood is in the systemic circulation/16% is in the heart and lungs.
- 64% of total blood volume is in the veins.
- 13%, arteries.
- 7%, arterioles and capillaries.
- 7%, heart.
- 9%, pulmonary vessels.
Law of La Place
- States the relation between wall tension, distending pressure, and radius of hollow viscus.
- In a sphere: P = 2T/r.
- In a cylinder as blood vessel: P = T/r.
- In a thin-walled asymmetric viscus: P = T (1/r₁ + 1/r₂).
- Significance:
- Determines tension generated in vessel wall, to balance the distending effect of pressure.
- Calculates the pressure generated during ventricular contraction based on the level of wall tension.
- Applications:
- Thin-walled capillaries withstand high pressure, the tension being small relative to small radius.
- Dilated ventricles (increased radius) in heart diseases generate more contraction tension to generate the same intraventricular pressure (needed normally to open semilunar valve since P = T/r).
Pressure in Various Parts of the Circulation
- Arterial pressure (Aorta): 120/80 mm Hg, with a mean of 90 mm Hg.
- Systemic capillaries: 35 mm Hg at the arteriolar end and 15 mm Hg at the venous end. The average "functional” capillary pressure is 25 mm Hg, allowing sufficient exchange across capillary wall.
- Systemic veins: 8-12 mm Hg in small peripheral veins and 5-6 mm Hg in large abdominal veins.
- Pulmonary arterial pressure: 25/8 mm Hg, with a mean of 16 mm Hg.
- Mean pulmonary capillary pressure: is only 10 mm Hg. A low value prevents filtration of fluid from pulmonary capillaries into lung alveoli.
Arterial Blood Pressure
- Systolic pressure= maximum pressure during systole in the aorta and large arteries, average 120 mmHg (90-140 mmHg).
- Diastolic pressure= minimum pressure during diastole, average 80 mmHg (60-90 mmHg).
- Pulse pressure= difference between systolic pressure and diastolic pressure, average 30-50 mmHg.
- Mean arterial pressure (MAP)=average pressure throughout cardiac cycle, average 90 mmHg.
- MAP = Diastolic pressure + 1/3 Pulse pressure = 90 mmHg.
- MAP is closer to Diastolic pressure because systole is shorter than diastole.
- Increased HR leads to a shorter cardiac cycle, shorter diastolic time, and increased MAP (near to mean true arithmetic).
Factors That Determine ABP
- MAP – Central venous pressure (CVP) = cardiac output (CO) × TPR.
- МАР = (CO × TPR) + CVP.
- MABP = (SV × HR × TPR) + CVP.
- Stroke volume (SV): Increased SV leads to increased Systolic pressure > diastolic pressure, leading to increased pulse pressure.
- Heart rate (HR): Increased HR leads to decreased diastolic time for ABP drop, leading to diastolic pressure > Systolic pressure, leading to decreased pulse pressure.
- Total peripheral resistance: Increased TPR leads to increased diastolic pressure, which is greater than Systolic pressure, leading to decreased pulse pressure.
- Arterial compliance: Decreased compliance due to atherosclerosis leads to increased systolic pressure due to decreased ability to expand and accommodate SV. -Decreases diastolic pressure is due to decreased recoil and increased pulse pressure. Central venous pressure: Increased CVP leads to increased МАР.
Physiologic Variations
- ABP increases with age due to loss of vessel elasticity.
- Sex:
- Before menopause, females have less ABP than males of the same age.
- After menopause, ABP increases in females due to hormonal changes.
- Race: races may have higher ABP & incidence of hypertension
- Emotions: Stress leads to increased sympathetic activation which can increase ABP
- Exercise:
- Dynamic exercise (alternating contractions and relaxations ): Moderate increases in systolic pressure occurs.
- Diastolic pressure decreases or is unchanged.
- Static exercise (continuous constant muscle contraction): Marked increases in systolic and diastolic pressures.
- Circadian rhythm relates ABP to normal persons working at daytime, in early morning ABP reaches peak sympathetic. -ABP touches highs at midnight due to lowest sympathetic levels. -Variations between 15 and 25 mmHg -Occurs opposite night-workers
- Gravity: measuring Each 1 cm below measurement of the heart increases ABP by 0.77 mmHg and each 1cm above is lowered ABP by 0.77.
- Respiration:
- "Traube-Hering waves": ABP fluctuates with the respiratory cycle, decreasing during inspiration and increasing during expiration.
- Variation range from 4-6 mmHg during resting breathing.
- Can reach 20 mmHg during deep breathing, which happens because during inspiration, the pulmonary vascular bed expands leading to a reversed SV, CO, ABP.
- Vasomotor waves (Mayer waves): oscillation ABP / 10 sec. range from 10 to 40 mmHg (or ever more) caused by "reflex oscillation" of one or more neural control mechanisms.
Functions of Veins
- Veins serve as blood reservoirs (capacity vessels): hold significant blood amounts with small pressure changes - 200 ml increase only increase 1mmGH pressure.
- Large compliant venous system. Specific blood reservoirs are cutaneous veins, large abdominal, hepatic, and spleen.
- Transport Vessels: with little resistance, faster than capillary flow, but slower than arterial flow (25% of velocity in aorta)
Venous Pressures
- Central Venous Pressure (CVP)- represents a Right Atrial Pressure with a Normal value of 0-2 mm Hg which balances the VR & heart pumping ability - Main filling force for ventricular, gradient difference for VR = 6 - 8 mmHg. -Also Indexes the blood volume- decreases by losing blood and increases it due to right-sided Heart Failure (↑CVP).
Peripheral venous pressure
- Determined from two factors (Sympathetic stimulation): BV Volume and Venous Compliance, which happens due to heart failure(CO decreasing increase BV and pressure ) . Vice Versa with Hemmorage, increased sympathetic stimulation tones the veins and increases its venous pressures.
- Effects of gravity alter venous pressure in upright positions, by applying 0.77 mg for cm height which causes varicose veins, whereas the head the pressure diminishes causing neck vein collapes
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.