Podcast
Questions and Answers
Which of the following processes is directly facilitated by Sertoli cells within the seminiferous tubules?
Which of the following processes is directly facilitated by Sertoli cells within the seminiferous tubules?
- Meiotic division of spermatogonia
- Secretion of testosterone
- Support and nourishment of developing sperm cells (correct)
- Transport of sperm cells to the epididymis
What would be the most likely outcome if the bulbourethral glands failed to secrete their characteristic product?
What would be the most likely outcome if the bulbourethral glands failed to secrete their characteristic product?
- The urethra would not be properly lubricated or neutralized before ejaculation. (correct)
- Sperm would be unable to properly develop within the testes.
- The volume of seminal fluid would significantly decrease.
- The sperm would not be able to survive in the female reproductive tract.
A man experiencing difficulty with erection may be experiencing an issue with which of the following?
A man experiencing difficulty with erection may be experiencing an issue with which of the following?
- Somatic nervous system
- Parasympathetic nervous system (correct)
- Sympathetic nervous system
- Endocrine system
How does the negative feedback mechanism involving testosterone function to maintain hormonal balance in males?
How does the negative feedback mechanism involving testosterone function to maintain hormonal balance in males?
What is the primary role of the fimbriae in the female reproductive system?
What is the primary role of the fimbriae in the female reproductive system?
Which layer of the uterus is shed during mensuration?
Which layer of the uterus is shed during mensuration?
What is the role of human chorionic gonadotropin (hCG) in maintaining a pregnancy?
What is the role of human chorionic gonadotropin (hCG) in maintaining a pregnancy?
Which of the following best describes the composition of semen?
Which of the following best describes the composition of semen?
What is the significance of the cooler temperature maintained within the scrotum for the testes?
What is the significance of the cooler temperature maintained within the scrotum for the testes?
How does the alkaline pH of semen contribute to successful fertilization?
How does the alkaline pH of semen contribute to successful fertilization?
Anabolic steroid abuse can lead to infertility in males because the exogenous testosterone can cause:
Anabolic steroid abuse can lead to infertility in males because the exogenous testosterone can cause:
If the epididymis were blocked, which of the following would be the most likely consequence?
If the epididymis were blocked, which of the following would be the most likely consequence?
Which hormone directly stimulates the Leydig cells to produce testosterone?
Which hormone directly stimulates the Leydig cells to produce testosterone?
The process by which the follicle ruptures and releases the secondary oocyte is known as what?
The process by which the follicle ruptures and releases the secondary oocyte is known as what?
What is the role of prostaglandins, found in the fluid produced by the seminal vesicles?
What is the role of prostaglandins, found in the fluid produced by the seminal vesicles?
Flashcards
Reproductive Systems Function
Reproductive Systems Function
Produce gametes and sex hormones; facilitate fertilization.
Male Reproductive System Function
Male Reproductive System Function
Produce & deliver sperm.
Testes Function
Testes Function
Produce sperm and testosterone.
Epididymis Function
Epididymis Function
Signup and view all the flashcards
Vas Deferens Function
Vas Deferens Function
Signup and view all the flashcards
Seminal Vesicles Function
Seminal Vesicles Function
Signup and view all the flashcards
Prostate Gland Function
Prostate Gland Function
Signup and view all the flashcards
Bulbourethral Glands Function
Bulbourethral Glands Function
Signup and view all the flashcards
Penis Function
Penis Function
Signup and view all the flashcards
FSH Function (Males)
FSH Function (Males)
Signup and view all the flashcards
LH Function (Males)
LH Function (Males)
Signup and view all the flashcards
Female Reproductive System Function
Female Reproductive System Function
Signup and view all the flashcards
Ovaries Function
Ovaries Function
Signup and view all the flashcards
Fallopian Tubes Function
Fallopian Tubes Function
Signup and view all the flashcards
Uterus Function
Uterus Function
Signup and view all the flashcards
Study Notes
- The male and female reproductive systems facilitate sexual reproduction
- These systems produce gametes and sex hormones, enabling fertilization
Male Reproductive System
- The primary function is to produce and deliver sperm to the female reproductive tract
- Key organs include: testes, epididymis, vas deferens, seminal vesicles, prostate gland, bulbourethral glands, and penis
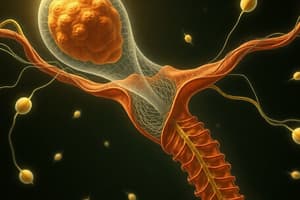
Testes
- The testes (testicles) are the primary male reproductive organs
- They produce sperm and testosterone
- They reside within the scrotum, which maintains a cooler temperature optimal for sperm production
- Each testis contains seminiferous tubules, the site of spermatogenesis (sperm production)
- Interstitial cells (Leydig cells) located between the seminiferous tubules produce testosterone
- Sertoli cells within the seminiferous tubules support and nourish developing sperm cells
- Spermatogenesis involves meiosis, reducing the chromosome number from diploid (46) to haploid (23) in sperm cells
- The process takes approximately 64-72 days
Epididymis
- A coiled tube on the posterior surface of each testis
- It serves as a storage and maturation site for sperm
- Sperm spend approximately 2-3 weeks in the epididymis, developing the ability to swim and fertilize an egg
Vas Deferens
- The vas deferens (ductus deferens) is a muscular tube that transports sperm from the epididymis to the ejaculatory duct
- Ascends through the spermatic cord, containing blood vessels, nerves, and muscles
- It passes through the inguinal canal and into the pelvic cavity
Seminal Vesicles
- Located on the posterior surface of the bladder
- Produce a viscous, alkaline fluid containing fructose, prostaglandins, and other substances that nourish and protect sperm
- Contributes roughly 60-70% of semen volume
Prostate Gland
- A walnut-sized gland inferior to the bladder
- Secretes a milky, slightly acidic fluid with enzymes, zinc, and other substances that enhance sperm motility and viability
- Prostatic fluid makes up about 20-30% of semen volume
Bulbourethral Glands
- The bulbourethral glands (Cowper's glands) are small glands inferior to the prostate gland
- Secretes a clear, alkaline mucus that lubricates the urethra and neutralizes acidic urine residue before ejaculation
Semen
- A mixture of sperm and seminal fluids from the testes, seminal vesicles, prostate gland, and bulbourethral glands
- The average ejaculate volume is approximately 2-5 ml, containing 20-150 million sperm per ml
- The alkaline pH of semen assists in neutralizing the acidic environment of the female vagina, protecting sperm
Penis
- The male copulatory organ, delivering sperm to the female reproductive tract
- Consists of the root, body (shaft), and glans penis (head)
- The body contains three cylindrical masses of erectile tissue: two corpora cavernosa and one corpus spongiosum
- The corpus spongiosum surrounds the urethra and forms the glans penis
- During sexual arousal, erectile tissues fill with blood, causing an erection
- Erection is controlled by the parasympathetic nervous system
- Ejaculation is controlled by the sympathetic nervous system, involving the propulsion of semen from the urethra
Hormonal Control in Males
- Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the anterior pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
- FSH stimulates Sertoli cells in the seminiferous tubules to support spermatogenesis
- LH stimulates Leydig cells in the testes to produce testosterone
- Testosterone promotes spermatogenesis, the development of secondary sexual characteristics, and libido
- Testosterone also has negative feedback effects on GnRH, FSH, and LH secretion, maintaining hormone balance
Female Reproductive System
- The primary function is to produce eggs, provide a site for fertilization, support fetal development, and facilitate childbirth
- Key organs include: ovaries, fallopian tubes, uterus, vagina, and mammary glands
Ovaries
- The primary female reproductive organs
- Responsible for producing eggs (ova) and female sex hormones (estrogen and progesterone)
- Located in the pelvic cavity, one on each side of the uterus
- Each ovary contains ovarian follicles, which consist of an oocyte (immature egg) surrounded by follicle cells
- Oogenesis (egg production) begins before birth, with primary oocytes arrested in prophase I of meiosis
- At puberty, hormonal changes stimulate some primary oocytes to continue meiosis
- Typically, one oocyte matures each month and is released during ovulation
- Ovulation involves the release of a secondary oocyte from a mature follicle
- After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone and estrogen
- Should fertilization not occur, the corpus luteum degenerates into the corpus albicans
Fallopian Tubes
- The fallopian tubes (uterine tubes or oviducts) transport the egg from the ovary to the uterus
- Fimbriae are finger-like projections that surround the ovary, helping to capture the released egg
- Fertilization typically occurs in the ampulla, the widest part of the fallopian tube
- The fertilized egg (zygote) is transported to the uterus for implantation
Uterus
- A hollow, muscular organ where a fertilized egg implants and develops
- Located in the pelvic cavity, between the bladder and the rectum
- Consists of three layers: the perimetrium (outer serous layer), the myometrium (middle muscular layer), and the endometrium (inner mucosal layer)
- The endometrium undergoes cyclical changes in response to hormones, preparing for implantation
- Endometrium layers: the stratum functionalis (shed during menstruation) and the stratum basalis (regenerates the functionalis layer)
- The cervix is the narrow lower portion of the uterus that connects to the vagina
Vagina
- A fibromuscular tube that extends from the cervix to the outside of the body
- Functions as the female copulatory organ, the birth canal, and the passageway for menstrual flow
- The vaginal wall contains rugae (folds) that allow it to stretch during childbirth
- The hymen is a thin membrane that partially covers the vaginal opening
Mammary Glands
- Modified sweat glands that produce milk to nourish a newborn infant
- Located in the breasts and consist of lobules containing alveoli, which secrete milk
- Milk is transported through ducts to the nipple
- Milk production is stimulated by the hormone prolactin, and milk ejection is stimulated by the hormone oxytocin
Hormonal Control in Females
- Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the anterior pituitary gland to release FSH and LH
- FSH stimulates the growth of ovarian follicles and estrogen production
- LH triggers ovulation and stimulates the formation of the corpus luteum
- Estrogen promotes the development of secondary sexual characteristics, regulates the menstrual cycle, and prepares the endometrium for implantation
- Progesterone, primarily secreted by the corpus luteum, helps maintain the endometrium during pregnancy
- If fertilization occurs, the developing embryo secretes human chorionic gonadotropin (hCG), which maintains the corpus luteum and prevents menstruation
- Estrogen and progesterone have negative feedback effects on GnRH, FSH, and LH secretion, maintaining hormone balance
- During menopause, the ovaries cease to function, resulting in decreased estrogen and progesterone levels and the cessation of menstruation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.