Podcast
Questions and Answers
Which of the following male reproductive organs is responsible for producing sperm and testosterone?
Which of the following male reproductive organs is responsible for producing sperm and testosterone?
- Epididymis
- Vas deferens
- Testes (correct)
- Prostate gland
Where do sperm mature and get stored?
Where do sperm mature and get stored?
- Epididymis (correct)
- Seminal vesicles
- Prostate gland
- Vas deferens
Which hormone stimulates the Leydig cells to produce testosterone?
Which hormone stimulates the Leydig cells to produce testosterone?
- Inhibin
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH) (correct)
- Gonadotropin-releasing hormone (GnRH)
What is the process of sperm production called?
What is the process of sperm production called?
Which part of the sperm cell contains the nucleus?
Which part of the sperm cell contains the nucleus?
Which component of semen is responsible for neutralizing the acidity of the female reproductive tract?
Which component of semen is responsible for neutralizing the acidity of the female reproductive tract?
Which of the following structures secretes a clear, alkaline mucus that lubricates the urethra?
Which of the following structures secretes a clear, alkaline mucus that lubricates the urethra?
What is the primary function of the vas deferens?
What is the primary function of the vas deferens?
Which of the following is the external organ that delivers sperm to the female reproductive tract?
Which of the following is the external organ that delivers sperm to the female reproductive tract?
What is the term for low sperm count?
What is the term for low sperm count?
Flashcards
Seminal Vesicles
Seminal Vesicles
Glands producing fluid rich in fructose and prostaglandins to nourish and protect sperm, contributing significantly to semen volume.
Vas Deferens
Vas Deferens
A muscular tube that transports sperm from the epididymis to the ejaculatory duct within the spermatic cord.
Spermatogenesis
Spermatogenesis
The process of sperm production in the seminiferous tubules, involving mitosis, meiosis, and spermiogenesis.
Testosterone
Testosterone
Signup and view all the flashcards
Luteinizing Hormone (LH)
Luteinizing Hormone (LH)
Signup and view all the flashcards
Semen
Semen
Signup and view all the flashcards
Erection
Erection
Signup and view all the flashcards
Ejaculation
Ejaculation
Signup and view all the flashcards
Testes
Testes
Signup and view all the flashcards
Epididymis
Epididymis
Signup and view all the flashcards
Study Notes
- The male reproductive system produces, maintains, and transports sperm cells, the male gametes, to the female reproductive tract.
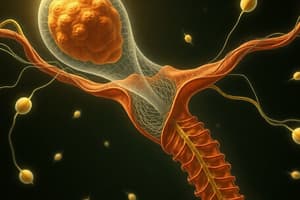
Anatomy
- The major organs include the testes, epididymis, vas deferens, seminal vesicles, prostate gland, bulbourethral glands, and penis.
- Testes: Located within the scrotum, the testes are responsible for producing sperm and testosterone.
- They contain tightly coiled seminiferous tubules, the site of spermatogenesis.
- Interstitial cells (Leydig cells) between the tubules produce testosterone.
- Epididymis: A coiled tube connected to the testis where sperm mature and are stored.
- Sperm spend about two to four weeks in the epididymis, where they gain motility and the ability to fertilize an egg.
- Vas Deferens: A muscular tube that transports sperm from the epididymis to the ejaculatory duct.
- It ascends within the spermatic cord, which also contains blood vessels and nerves.
- Seminal Vesicles: Glands that produce a fluid rich in fructose, prostaglandins, and other substances that nourish and protect sperm.
- This fluid constitutes a significant portion of semen volume.
- Prostate Gland: Surrounds the urethra and produces a milky fluid containing enzymes and zinc that enhance sperm motility and fertilization.
- Bulbourethral Glands (Cowper's Glands): Small glands located near the urethra that secrete a clear, alkaline mucus that lubricates the urethra and neutralizes acidic residues.
- Penis: The external organ that delivers sperm to the female reproductive tract during sexual intercourse.
- It consists of the root, the shaft or body, and the glans penis.
- The glans is covered by the foreskin, or prepuce, which may be removed during circumcision.
- The penis contains three cylindrical masses of erectile tissue: two corpora cavernosa and one corpus spongiosum, which surrounds the urethra.
Hormonal Control
- The hypothalamus, pituitary gland, and testes form a hormonal axis that regulates male reproductive functions.
- Gonadotropin-Releasing Hormone (GnRH): Released by the hypothalamus.
- Stimulates the anterior pituitary to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- Luteinizing Hormone (LH): Stimulates Leydig cells in the testes to produce testosterone.
- Follicle-Stimulating Hormone (FSH): Acts on Sertoli cells in the seminiferous tubules to support spermatogenesis.
- Sertoli cells also produce inhibin, which inhibits FSH secretion.
- Testosterone: The primary male sex hormone, responsible for the development of male secondary sexual characteristics, muscle growth, and maintenance of libido.
- It also has a negative feedback effect on the hypothalamus and anterior pituitary, reducing GnRH, LH, and FSH secretion.
Spermatogenesis
- Spermatogenesis is the process of sperm production that occurs in the seminiferous tubules of the testes.
- It involves three main phases:
- Mitosis: Spermatogonia (diploid stem cells) undergo mitosis to produce more spermatogonia.
- Meiosis: Primary spermatocytes undergo meiosis I to form secondary spermatocytes, which then undergo meiosis II to produce spermatids (haploid cells).
- Spermiogenesis: Spermatids differentiate into mature spermatozoa (sperm cells). This involves the formation of a flagellum (tail) and condensation of the nucleus.
- Each sperm cell consists of a head (containing the nucleus and acrosome), a midpiece (containing mitochondria), and a tail (flagellum) for motility.
- The entire process of spermatogenesis takes approximately 64 to 72 days in humans.
Erection and Ejaculation
- Erection: The enlargement and stiffening of the penis, caused by vasodilation of blood vessels in the erectile tissues (corpora cavernosa and corpus spongiosum).
- Parasympathetic nerves trigger the release of nitric oxide (NO), which relaxes smooth muscle in the penile arteries, allowing increased blood flow.
- The engorgement of erectile tissues compresses the veins, preventing blood from leaving the penis.
- Ejaculation: The expulsion of semen from the male urethra, involving two phases:
- Emission: Sympathetic nerves stimulate peristaltic contractions of the vas deferens, seminal vesicles, and prostate gland, which move semen into the urethra.
- Expulsion: Semen is forcefully expelled from the urethra by contractions of skeletal muscles at the base of the penis.
- After ejaculation, sympathetic stimulation causes vasoconstriction in the penile arteries, reducing blood flow and leading to detumescence (loss of erection).
Semen
- Semen is a mixture of sperm cells and seminal fluid.
- Seminal fluid is produced by the seminal vesicles, prostate gland, and bulbourethral glands.
- It provides nutrients, buffers, and other substances that support sperm viability and motility.
- A typical ejaculate contains 2 to 5 ml of semen, with 20 to 150 million sperm cells per milliliter.
- Semen is slightly alkaline, which helps neutralize the acidic environment of the female reproductive tract.
Male Fertility
- Male fertility depends on several factors, including sperm count, sperm motility, and sperm morphology (shape).
- Low sperm count (oligospermia) or the absence of sperm (azoospermia) can lead to infertility.
- Impaired sperm motility (asthenozoospermia) or abnormal sperm morphology (teratozoospermia) can also reduce fertility.
- Other factors that can affect male fertility include hormonal imbalances, genetic disorders, infections, and environmental toxins.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.