Podcast
Questions and Answers
The hypothalamic-pituitary-testicular axis is regulated by a negative feedback loop. Which hormone(s) primarily inhibit the secretion of GnRH from the hypothalamus?
The hypothalamic-pituitary-testicular axis is regulated by a negative feedback loop. Which hormone(s) primarily inhibit the secretion of GnRH from the hypothalamus?
- Inhibin
- Luteinizing Hormone (LH)
- Testosterone (correct)
- Follicle-Stimulating Hormone (FSH)
The testes perform two main reproductive functions. Which of the following best describes these functions?
The testes perform two main reproductive functions. Which of the following best describes these functions?
- Oogenesis and folliculogenesis
- Spermatogenesis and steroidogenesis (correct)
- Steroidogenesis and oogenesis
- Spermatogenesis and oogenesis
What is the primary role of Sertoli cells within the seminiferous tubules?
What is the primary role of Sertoli cells within the seminiferous tubules?
- Storage of mature sperm
- Secretion of luteinizing hormone
- Support and nourishment of developing sperm (correct)
- Testosterone production
Why is proper regulation of testicular temperature critical for male fertility?
Why is proper regulation of testicular temperature critical for male fertility?
In the testes, Leydig cells and Sertoli cells work cooperatively, in a similar manner to what cells in the ovaries?
In the testes, Leydig cells and Sertoli cells work cooperatively, in a similar manner to what cells in the ovaries?
A 32-year-old male presents with infertility, chronic sinusitis, and bronchiectasis. Which genetic disorder is most likely responsible for these symptoms?
A 32-year-old male presents with infertility, chronic sinusitis, and bronchiectasis. Which genetic disorder is most likely responsible for these symptoms?
Which of the following can still cause infertility even when a male has a normal number of sperm?
Which of the following can still cause infertility even when a male has a normal number of sperm?
Which hormone directly stimulates Leydig cells to produce testosterone?
Which hormone directly stimulates Leydig cells to produce testosterone?
Elevated levels of FSH stimulate Sertoli cells, which leads to testosterone's aromatization into what?
Elevated levels of FSH stimulate Sertoli cells, which leads to testosterone's aromatization into what?
What is the function of Androgen-Binding Protein (ABP) secreted by Sertoli cells?
What is the function of Androgen-Binding Protein (ABP) secreted by Sertoli cells?
SSBG has a high binding affinity to testosterone, so most of the testosterone in the blood is bound. What approximate percentage of testosterone is biologically active?
SSBG has a high binding affinity to testosterone, so most of the testosterone in the blood is bound. What approximate percentage of testosterone is biologically active?
How does testosterone contribute to male secondary sex characteristics during puberty?
How does testosterone contribute to male secondary sex characteristics during puberty?
Testosterone is converted into what enzyme in the target cells?
Testosterone is converted into what enzyme in the target cells?
Following their production in the seminiferous tubules, how long do sperm need to pass through the epididymis to develop the capability of motility?
Following their production in the seminiferous tubules, how long do sperm need to pass through the epididymis to develop the capability of motility?
Where are sperm stored in the testes?
Where are sperm stored in the testes?
The seminal vesicles contribute significantly to the composition of semen by secreting which of the following substances?
The seminal vesicles contribute significantly to the composition of semen by secreting which of the following substances?
What constituents are secreted by the prostate gland?
What constituents are secreted by the prostate gland?
Once ejactulated, what is sperm's lifespan at body temperature?
Once ejactulated, what is sperm's lifespan at body temperature?
The sensory input that initiates the male sexual act involves which nerve and spinal cord structures?
The sensory input that initiates the male sexual act involves which nerve and spinal cord structures?
What is the primary role of nitric oxide (NO) in achieving an erection?
What is the primary role of nitric oxide (NO) in achieving an erection?
Erectile dysfunction caused by vascular disease can be successfully treated with what?
Erectile dysfunction caused by vascular disease can be successfully treated with what?
The reflex centers of the spinal cord emit what kind of impulses to cause emission?
The reflex centers of the spinal cord emit what kind of impulses to cause emission?
What combination of fluids makes up semen?
What combination of fluids makes up semen?
During the stages of the male sexual act, the filling of the internal urethra triggers a feeling of fullness. What nerves send the signals?
During the stages of the male sexual act, the filling of the internal urethra triggers a feeling of fullness. What nerves send the signals?
Damage to the preoptic nucleus may lead to a decrease in what hormone?
Damage to the preoptic nucleus may lead to a decrease in what hormone?
Flashcards
Hypothalamic-Pituitary-Testicular Axis
Hypothalamic-Pituitary-Testicular Axis
Controls male reproduction; involves hypothalamus, pituitary, and testes.
Identical Hypothalamic Areas
Identical Hypothalamic Areas
The hypothalamic areas controlling testicular function, ovaries.
GnRH Function
GnRH Function
Stimulates GnRH receptors to secrete LH & FSH.
Hypogonadism
Hypogonadism
Signup and view all the flashcards
Dual Function of Testes
Dual Function of Testes
Signup and view all the flashcards
Seminiferous Tubules
Seminiferous Tubules
Signup and view all the flashcards
Sertoli cells
Sertoli cells
Signup and view all the flashcards
Leydig cells
Leydig cells
Signup and view all the flashcards
Testes Location
Testes Location
Signup and view all the flashcards
Leydig and Sertoli cells
Leydig and Sertoli cells
Signup and view all the flashcards
Kartagener Syndrome
Kartagener Syndrome
Signup and view all the flashcards
Sperm Morphology effect
Sperm Morphology effect
Signup and view all the flashcards
Luteinizing Hormone
Luteinizing Hormone
Signup and view all the flashcards
Follicle-stimulating hormone
Follicle-stimulating hormone
Signup and view all the flashcards
Growth Hormone
Growth Hormone
Signup and view all the flashcards
Cholesterol Transport
Cholesterol Transport
Signup and view all the flashcards
LH Receptors
LH Receptors
Signup and view all the flashcards
Blood-Testis Barrier
Blood-Testis Barrier
Signup and view all the flashcards
Sertoli Cell Testosterone
Sertoli Cell Testosterone
Signup and view all the flashcards
Testosterone Functions
Testosterone Functions
Signup and view all the flashcards
Dihydrotestosterone
Dihydrotestosterone
Signup and view all the flashcards
Sperm Maturation
Sperm Maturation
Signup and view all the flashcards
Seminal Vesicles
Seminal Vesicles
Signup and view all the flashcards
Prostate Gland
Prostate Gland
Signup and view all the flashcards
Semen Composition:
Semen Composition:
Signup and view all the flashcards
Study Notes
- Lecture #29 focuses on male reproductive physiology.
Hypothalamic-Pituitary-Testicular Axis
- Hypothalamic areas controlling the testes are identical to those regulating the ovaries.
- GnRH (gonadotropin-releasing hormone) is secreted into the hypophyseal portal system, binding to anterior pituitary gonadotropes.
- GnRH stimulates GnRH receptors to secrete the peptide hormones Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH).
- Inability of the hypothalamus to secrete normal amounts of GnRH can cause hypogonadism.
- Frohlich's syndrome, also known as hypothalamic eunuchism, involves the inability to secrete normal amounts of GnRH alongside with the abnormality of the feeding center of the hypothalamus, causing the person to overeat.
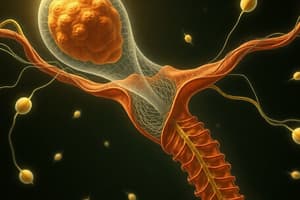
Testicular functions
- The testes perform two key functions: spermatogenesis (sperm production) and steroidogenesis (steroid hormone production).
- Sperm production occurs in the seminiferous tubules.
- Seminiferous tubules are comprised of germ cells and Sertoli cells.
- Sertoli cells provide a supportive and secretory role in spermatogenesis.
- Leydig cells produce testosterone.
- Testes are located outside of the body to keep the temperature a few degrees cooler than normal body temperature for sperm production.
- Dartos and cremaster muscles position the scrotum for optimal temperature regulation.
- The pampiniform plexus cools arterial blood entering the scrotum.
- Testicular endocrine functions reside in Leydig and Sertoli cells.
- Leydig and Sertoli cells work cooperatively in synthesizing testosterone.
Kartagener Syndrome
- Rare genetic disorder, affecting 1:32,000 live births, is also known as "Primary Cilia Dyskinesia"
- Symptoms: infertility, chronic sinusitis, and bronchiectasis
Sperm Morphology and Motility
- A normal number of sperm does not guarantee fertility.
- A person is likely to be infertile if their sperm are morphologically abnormal or nonmotile.
Hormonal Factors Stimulating Spermatogenesis
- In the interstitium of the testes, Leydig cells secrete testosterone, which is essential for growth and division of the testicular germinal cells.
- The anterior pituitary gland secretes luteinizing hormone, stimulating the Leydig cells to secrete testosterone.
- The anterior pituitary gland secretes follicle-stimulating hormone, stimulating the Sertoli cells
- Conversion of the spermatids to sperm will not occur without the stimulation of the Sertoli cells from the follicle-stimulating hormone (FSH).
- Sertoli cells stimulated by FSH produce estrogens from testosterone.
- Growth hormone is necessary for controlling the background metabolic functions of the testes and promotes early division of the spermatogonia; absence causes infertility.
Leydig Cells
- Leydig cells transport cholesterol, which serves as the initial structure for steroid-hormone synthesis.
- LH binds to surface membrane LH receptors, activating and producing steroid hormone synthetic enzymes like side-chain cleavage enzyme complex.
- Leydig cells produce testosterone, which diffuses is out and either enters circulation or Sertoli cells.
Sertoli Cells
- Sertoli cells form tight junctions to create a functional blood-testis barrier, which is selectively permeable for substances like testosterone.
- Sertoli cells primarily express FSH receptors.
- Sertoli cells GPCR (G protein-coupled receptor) work through the AC-induced cAMP system.
- Sertoli cells stimulate the synthesis of aromatase and inhibins for FSH negative feedback.
- Sertoli cells rely on Leydig cells for testosterone.
- Aromatase activation facilitates the conversion of testosterone into estradiol.
- Sertoli cells also regulate much of the protein synthesis in both Sertoli and Leydig cells.
- Sertoli cells secrete androgen-binding protein (ABP) along with testosterone into the seminiferous tubular lumen.
Testosterone
- Testosterone is produced from the conversion of androstenedione via 17-Ketosteroid reductase.
- Testosterone has a high binding affinity to sex steroid-binding globulin (SSBG) and albumin.
- Only ~2% of testosterone circulates in the biologically active free form.
- The liver produces SSBG.
- Testosterone secreted in the urine and feces.
- Testosterone is responsible for the distinguishing characteristics of the masculine body.
- Essentially no testosterone is produced during childhood until about the ages of 10 to 13 years.
- During puberty, testosterone contributes to the enlargement of the penis, scrotum, and testes.
- Testosterone contributes to male secondary sex characteristics, increases skin thickness, spurs muscle development, and increases bone matrix and causes calcium retention.
- The effects of testosterone occur due to increased rate of protein formation in the target cells.
- Testosterone enters the target cells, is converted to dihydrotestosterone by 5 α-reductase, and migrates to the cell nucleus, binds with a nuclear protein, and induces transcription.
- Testosterone is secreted from Leydig cells, exerting negative feedback on the hypothalamus and anterior pituitary.
- Testosterone stimulates Sertoli cells to release inhibins, which provides negative feedback, decreasing the secretion of Follicle Stimulating Hormone (FSH).
Sperm
- Sperm matures in the epididymis for 18-24 hours, which develops the capability of motility.
- Several inhibitory proteins in the epididymal fluid prevent final motility until after ejaculation.
- In the adult testicles, there can be up to 120M sperm and stored for up to a month.
- The spermatoza are kept in an inactive state by multiple inhibitory substances.
Seminal Vesicles
- Seminal vesicles are each lined with a secretory epithelium.
- Epithelium in seminal vesicles secretes nutrient substances, prostaglandins, and fibrinogen.
- During the process of emission and ejaculation, the seminal vesicle empties its contents into the ejaculatory duct after the vas deferens empties the sperm.
Prostate Gland
- Secretes a thin, milky fluid containing calcium, citrate ion, phosphate ion, a clotting enzyme, and a profibrinolysin.
- During the emission, the prostate glands contracts simultaneously with the Contractions of vas deferens.
- Slightly alkaline prostatic fluid helps neutralize the acidity of the other seminal fluids, which enhances the motility and fertility of the sperm.
Semen
- Semen composition breakdown: fluid/sperm from the vas deferens (10%), fluid from the seminal vesicles (60%), and fluid from the prostate gland (30%).
- The fluids mix in the internal urethra with mucus already secreted from the bulbourethral glands.
- Sperm has a maximal lifespan of 24-48 hours at body temperature once ejaculated in the semen.
Neuronal Stimulus for Male Sexual Act
- Sensory nerve signals for initiating the male sexual act is the glans penis stimulates signals to pudendal nerve, then the sacral plexus into the sacral portion of cord.
- Signals travel to undefined areas of the brain.
Stages of the Male Sexual Act
- Erection is initiated through parasympathetic impulses.
- Parasympathetic nerve fibers release nitric oxide and/or vasoactive intestinal peptide along with acetylcholine.
- NO activates the enzyme guanylyl cyclase, causing increased formation of cGMP.
- cGMP relaxes the arteries of the penis and the smooth muscle fibers in the erectile tissue of the corpora cavernosa and corpus spongiosum.
- Erectile dysfunction, caused by vascular disease, can be treated with phosphodiesterase-5 (PDE-5) inhibitors.
- PDE-5 inhibitors increase cGMP levels in the erectile tissue by inhibiting the enzyme PDE-5 to Prolong the effect of cGMP to cause erection
- Emission and ejaculation are functions of the sympathetic nerves.
- Intense sexual stimulus causes reflex centers of the spinal cord to emit sympathetic impulses.
- Nerves leave the cord at T12 to L2 to initiate emission.
- Filling of the internal urethra with semen elicits sensory signals transmitted through the pudendal nerves to the sacral regions of the cord.
- Sensory signals excite rhythmical contraction of the internal genital organs and cause contraction of muscles of the penial erectile tissue.
- Together, increases increase in pressure in the erectile tissue of the penis and the genital ducts and urethra causes semen to be ejaculated.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.