Podcast
Questions and Answers
What is the primary role of the lymphatic system in maintaining fluid balance within the body?
What is the primary role of the lymphatic system in maintaining fluid balance within the body?
- To produce albumin to maintain osmotic pressure in the blood.
- To return excess interstitial fluid and proteins to the bloodstream. (correct)
- To filter waste products from the blood and excrete them in urine.
- To directly regulate blood pressure by adjusting sodium levels.
Why are lymphatic capillaries particularly well-suited for absorbing interstitial fluid?
Why are lymphatic capillaries particularly well-suited for absorbing interstitial fluid?
- They have valves that promote fluid entry but prevent its exit.
- They possess a continuous layer of endothelial cells tightly joined together.
- They have walls made of overlapping epithelial cells forming one-way mini-valves. (correct)
- They contain a thick basement membrane that prevents leakage.
How does the structure of lymphatic vessels support the unidirectional flow of lymph?
How does the structure of lymphatic vessels support the unidirectional flow of lymph?
- The smooth muscle layer in the vessel walls continuously contracts to propel lymph forward.
- The close proximity to arteries allows for pressure gradients to drive lymph flow.
- The large diameter of lymphatic vessels reduces resistance and promotes flow.
- Internal valves prevent backflow, ensuring lymph moves towards the heart. (correct)
What is the primary mechanism by which lymph is moved through the lymphatic system, given that it lacks a central pump?
What is the primary mechanism by which lymph is moved through the lymphatic system, given that it lacks a central pump?
Which of the following is a primary function of lymph nodes?
Which of the following is a primary function of lymph nodes?
What is the functional significance of the spleen's red pulp?
What is the functional significance of the spleen's red pulp?
How does the thymus contribute to immune function?
How does the thymus contribute to immune function?
What is the role of Mucosa-Associated Lymphoid Tissue (MALT) in the body's defense?
What is the role of Mucosa-Associated Lymphoid Tissue (MALT) in the body's defense?
Which characteristic distinguishes innate immunity from adaptive immunity?
Which characteristic distinguishes innate immunity from adaptive immunity?
How do interferons protect the body against viral infections?
How do interferons protect the body against viral infections?
Which of the following is the most accurate description of the complement system's function?
Which of the following is the most accurate description of the complement system's function?
What is the role of natural killer (NK) cells in the immune system?
What is the role of natural killer (NK) cells in the immune system?
Which of the following events is a cardinal sign of inflammation?
Which of the following events is a cardinal sign of inflammation?
How does fever contribute to the body's defense against infection?
How does fever contribute to the body's defense against infection?
What is the role of T-lymphocytes in adaptive immunity?
What is the role of T-lymphocytes in adaptive immunity?
How do antibodies contribute to the elimination of pathogens from the body?
How do antibodies contribute to the elimination of pathogens from the body?
Which type of immunity is acquired through vaccination?
Which type of immunity is acquired through vaccination?
What is the underlying cause of autoimmune disorders?
What is the underlying cause of autoimmune disorders?
What is the role of Regulatory T-lymphocytes (T-regs) in the immune response?
What is the role of Regulatory T-lymphocytes (T-regs) in the immune response?
How does the lymphatic system contribute to the spread of cancer (metastasis)?
How does the lymphatic system contribute to the spread of cancer (metastasis)?
What is the role of MHC molecules in the adaptive immune response?
What is the role of MHC molecules in the adaptive immune response?
Which is the primary method by which the body responds to soluble antigens such as toxins?
Which is the primary method by which the body responds to soluble antigens such as toxins?
What triggers the release of Oxytocin during breast feeding?
What triggers the release of Oxytocin during breast feeding?
What is the most important risk factor for Cervical Cancer?
What is the most important risk factor for Cervical Cancer?
Flashcards
Lymphatic System Functions
Lymphatic System Functions
Transports lymphocytes, returns excess fluid to blood, maintains blood volume.
Lymphatic System Components
Lymphatic System Components
Lymph vessels, lymphatic tissues, and organs. Lymph is the fluid itself.
Primary Lymph Structures
Primary Lymph Structures
Red bone marrow and thymus; involved in lymphocyte maturation.
Secondary Lymph Structures
Secondary Lymph Structures
Signup and view all the flashcards
Lymphatic Capillaries
Lymphatic Capillaries
Signup and view all the flashcards
Metastasis
Metastasis
Signup and view all the flashcards
Lymphatic Movement
Lymphatic Movement
Signup and view all the flashcards
Lymphedema
Lymphedema
Signup and view all the flashcards
Red Bone Marrow
Red Bone Marrow
Signup and view all the flashcards
Thymus
Thymus
Signup and view all the flashcards
Lymph Nodes
Lymph Nodes
Signup and view all the flashcards
Lymph Node Flow
Lymph Node Flow
Signup and view all the flashcards
Hodgkin Lymphoma
Hodgkin Lymphoma
Signup and view all the flashcards
Spleen
Spleen
Signup and view all the flashcards
Splenectomy
Splenectomy
Signup and view all the flashcards
Tonsillitis
Tonsillitis
Signup and view all the flashcards
Lymphatic Nodules
Lymphatic Nodules
Signup and view all the flashcards
MALT
MALT
Signup and view all the flashcards
Innate Immunity
Innate Immunity
Signup and view all the flashcards
Adaptive Immunity
Adaptive Immunity
Signup and view all the flashcards
Cardinal Signs of Inflammation
Cardinal Signs of Inflammation
Signup and view all the flashcards
Fever
Fever
Signup and view all the flashcards
Adaptive Immunity
Adaptive Immunity
Signup and view all the flashcards
Two branches of adaptive immunity
Two branches of adaptive immunity
Signup and view all the flashcards
Organ Transplants and MHC Molecules
Organ Transplants and MHC Molecules
Signup and view all the flashcards
Study Notes
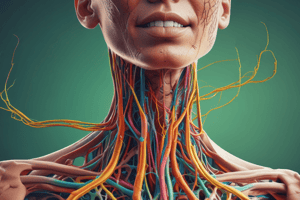
Lymphatic System Functions
- Transports lymphocytes and other immune cells
- Returns excess fluid from body tissues to the blood, maintaining blood volume
Lymphatic System Components
- Consists of lymph vessels, lymphatic tissues, and organs
- Lymph is fluid transported within the lymph vessels
Primary Lymph Structures
- Involved in lymphocyte maturation and formation
- Includes red bone marrow and thymus
Secondary Lymph Structures
- Houses immune cells
- Responsible for immune response initiation
- Includes lymph nodes, spleen, tonsils, and lymphatic nodules as well as mucosa-associated lymphatic tissue (MALT)
Characteristics of Lymph
- Some fluid from blood capillaries isn't reabsorbed
- Interstitial fluid enters capillaries where it becomes lymph
Lymph Components
- Consists of water, dissolved solutes, and small amounts of protein
- May contain cell debris, pathogens, or cancer cells
Lymphatic Capillaries
- Absorb interstitial fluid through small, closed-ended vessels
- Interspersed with most blood capillaries
- Absent in avascular tissues, red bone marrow, spleen, and CNS
- Slightly larger than blood capillaries, with no basement membrane
- Walls are overlapping epithelial cells with one-way flaps
- Lacteals are lymphatic capillaries in GI tract absorbing lipid-soluble substances
Cancer Metastasis
- Cancer cells travel, forming secondary tumors
- Cancer cells develop in new locations within the body
- Cancerous cells break away from a primary tumor
- Cancer cells are transported in the lymph
Lymphatic Vessels
- Vessels are fed by lymphatic capillaries
- Located near arteries and veins
- Valves prevent pooling and backflow
Lymph Movement
- The lymphatic system lacks a pump, relies on skeletal muscles, respiratory pumps, pulsation of nearby arteries, and rhythmic contraction of larger lymph vessel walls to move lymph
- Some vessels connect to lymph nodes for lymph filtration
Lymphedema
- Blockage of lymph system results in swelling
- Interstitial fluid accumulation due to obstructed lymphatic drainage
- Usually caused by obstruction, surgical removal of lymph nodes, spread of malignant tumors, scarring from radiation therapy, or trauma/infection
- Can be controlled with compression garments, exercise, and massage
Elephantiasis
- Extreme form of lymphedema
- Caused by filarial worms infecting the lymphatic system, occurs in southeast Asia/Africa
Red Bone Marrow
- Found between trabeculae of spongy bone
- Located in flat bones such as the skull, ribs, sternum, vertebrae, ossa coxae, and the head of the femur, etc
- Site of hematopoiesis (blood cell formation)
- T and B lymphocytes are formed
- T-lymphocytes migrate to the thymus to complete maturation
Thymus
- Involved in T-lymphocyte maturation
- Located in the mediastinum
- Larger in children than adults
- Grows until puberty, then gradually replaced by adipose tissue
- Outer cortex contains immature T-lymphocytes
- Inner medulla contains mature T-lymphocytes
Lymph Nodes
- Filter lymph and remove unwanted substances
- Small, oval, encapsulated structures along lymph vessel pathways
- Occur in clusters, filtering lymph from body regions
- Cervical nodes receive lymph from head and neck
- Axillary nodes receive lymph from breasts, axilla, and upper limbs
- Inguinal nodes receive lymph from pelvis and lower limbs
Lymph Flow Through Nodes
- Enters nodes through afferent vessels
- Creates pressure, pushing lymph out through a single exit vessel
- Lymph is monitored for foreign material
- Macrophages remove debris
- Lymphocytes may initiate an immune response
- Enlarged nodes can be palpated in neck and axilla
Hodgkin Lymphoma vs Non-Hodgkin Lymphoma
-
Both:
- Malignant neoplasms from lymph structures
- Feature nontender, enlarged lymph nodes
-
Hodgkin:
- May also cause night sweats, fever, and weight loss
- Occurs in young adults and people over 60
- Can be cured with excision, radiation, and chemotherapy if localized
-
Non-Hodgkin:
- More common, aggressive, and multiple
Spleen
- The largest lymphatic organ, contains tissues of the spleen
- White pulp: clusters of T and B lymphocytes and macrophages around the central artery
- Red pulp contains erythrocytes, platelets, macrophages, and B-lymphocytes; stores erythrocytes and platelets
Splenectomy
- Surgical removal of the spleen
- May be required after a ruptured spleen (most common), or infection, cyst, tumor, blood disorder, or cancer
- May predispose to life-threatening infections
Tonsils
- Pharyngeal tonsil: called adenoids when enlarged
- Palatine tonsils and lingual tonsils
Tonsillitis and Tonsillectomy
- Acute tonsillitis: inflammation and infection of tonsils
- Palatine tonsils are most commonly affected
- Symptoms: reddened and enlarged tonsils, partial pharynx obstruction, fever, chills, sore throat, difficulty swallowing; caused by viruses or bacteria
- Persistent recurrent infections is chronic tonsillitis, may require surgical removal
Lymphatic Nodules
- Clusters of lymphatic cells with some extracellular matrix
- Not completely surrounded by connective tissue capsule
- Scattered nodules diffuse lymphatic tissue
- Found in every body organ, help defend against infection
- Groups together form larger structures called MALT
Mucosa-Associated Lymphatic Tissue (MALT)
- Located in GI, respiratory, genital, and urinary tracts
- Helps defend against foreign substances
- Peyer patches: collections of lymphatic nodules within the wall of the GI tract, especially in the ileum
Types of Immunity
- Two types of Immunity differ based on cells involved, specificity of cell response, mechanism of elimination of harmful sunstances, and response time
Body Defense
- Innate defenses guard against any pathogen
- Adaptive defenses (immunity) mount a response against a very specific target
- Innate defenses respond rapidly: species resistance, mechanical barriers, chemical barriers, natural killer cells, inflammation, phagocytosis, and fever
- Adaptive immunity is specific and develops slowly, carried out by lymphocytes
- Innate and adaptive immunity are distinct but work together
Innate Immunity
- Present at birth, protects against variety of substances (non-specific)
- No prior exposure to substances is necessary
- Includes barriers of the skin and mucosal membranes, nonspecific cellular and molecule internal defenses
- Responds immediately to potentially harmful agents
Adaptive Immunity
- Acquired and specific
- Response to antigen involves T and B-lymphocytes
- Responds to one specific foreign substance
- Takes several days to be effective
First Line of Defense: Mechanical Barriers
- Unbroken skin and mucous membranes prevent pathogen entry
- Includes hair, mucus, and sweat
Second Line of Defense: Chemical Barriers
- Highly acidic environment from gastric juice, or lysozyme in tears, kill many pathogens
- Interferons produced by cells infected by viruses induce nearby cells to produce antiviral enzymes and stimulate phagocytosis
- Complement activation stimulates inflammation, attracts phagocytes, and enhances phagocytosis
Natural Killer (NK) Cells
- Lymphocyte that defends against viruses and cancer by secreting perforins
- NK cells enhance inflammation
Inflammation
- Tissue response to pathogens characterized by heat, swelling, redness, and pain
- Vasodilation, blood volume increase, white blood cell invasion, blood clotting, and fibroblast appearance
Phagocytosis
- Neutrophils and monocytes (active phagocytes) leave the bloodstream at areas of injury (diapedesis)
- Attracted to injured area via chemotaxis
- Neutrophils engulf smaller particles, monocytes attack larger ones
- Monocytes become macrophages
- Removes foreign particles from the lymph
Fever
- Protection against infection by interfering with bacterial growth
- Fever reduces the amount of iron and nutrients available to pathogens
- Phagocytic cells attack with greater vigor when temperature rises
Innate Immunity Charcteristics
- Prevents entry of potentially harmful substances
- Responds nonspecifically to a range of harmful substances
- First line of defense is skin and mucosal membrane
- Second line: neutrophils, macrophages, dendritic cells, eosinophils, basophils, and NK cells
Immune System
- Antimicrobial proteins and interferons
- Interferons nonspecifically impede viral spread
- Leukocytes and virus infected cells produce IFNa and IFNβ- bind to neighboring cells and prevents function
- Triggers synthesis of enzymes that destroy viral nucleic acids, inhibit synthesis of viral proteins
- Stimulate NK cells to destroy virus infected cells T-lymphocytes and NK cells produce IFN, stimulates macrophages to destroy virus infected cells
Antimicrobial Proteins and Complement System
- Complement system: group of over 30 plasma proteins that works along with complement antibodies
- Identified with letter C and a number, synthesized by the liver, continuously released in inactive form
- Activation occurs by enzyme cascade, especially potent against bacterial infections
Inflammation (NsID)
- Immediate response to ward of unwanted substances
- Release of chemicals that initiate responses from injured tissue, basophils, mast cells, and infectious organisms
- Released chemicals include histamine, leukotrienes, prostaglandins, chemotactic factors
Vascular Changes Due to Released Chemicals
- Vasodilation
- Increased capillary permeability
- Increased endothelial expression of molecules for leukocyte adhesion
Leukocyte Recruitment
- Leukocytes release cytokines stimulating leukopoiesis in marrow
- Macrophages release pyrogens that induce fever
Delivery of Plasma Proteins to Site
- Immunoglobulins, complement, clotting factors, and kinins are delivered
- Clotting proteins form clots that wall off microbes
- Kinins stimulate pain receptors, increase capillary permeability
Effects of Inflammation
- Fluid (exudate) moves from blood to injured or effected area, contains proteins, immune cells to eliminate pathogens, promote healing
- Vasodilation brings more blood to area and increase capillary permeability
- Extravasted fluid is taken up by lymphatic capillaries, carries away debris while swelling results some fluid in interstitial space
Resolution of Inflammation
- The inflammatory response slows within 72 hours
- Macrophages eat bacteria, damaged host cells, and dying neutrophils
- Tissue repair begins as fibroblasts form new connective tissue
Cardinal Signs of Inflammation
- Redness from increased blood flow
- Heat from increased blood flow and increased metabolic activity
- Swelling from increased fluid loss from capillaries
- Pain from stimulation of pain receptors (compression (extra fluid) and chemical irritants)
- Loss of function with severe pain and swelling
- Duration of acute inflammation 8-10 days
Fever (NsID - pyrexia)
- Body temperature above normal (by 1°C or more)
- Results from the release of pyrogens from immune cells or infectious agents
Fever Events
- Pyrogens circulate through blood and target the hypothalamus
- The hypothalamus releases prostaglandin E2 increasing the temperature set point causing fever
- Fever stages: onset, stadium, and defervescence
Fever Benefits
- Inhibits reproduction of bacteria and viruses
- Promotes interferon activity
- Increases adaptive immunity
- Accelerates tissue repair
- Increases immune cell migration from blood
- Low-grade fever is recommended to be left untreated
Risks with High Fever
- Potentially dangerous
- Changes in metabolic pathways and denaturation of proteins
- Possible seizures
- Irreversible brain damage above 41°C (106°F)
- Death is likely above the temperature of 42.8°C (109°F)
Pus and Abscess
- Pus is an exudate that contains destroyed pathogens, dead leukocytes, macrophages, cellular debris
- Removed by lymphatic system or through skin
- If not completely cleared, can form an abscess
- Pus is walled off by collagen fibers and removed by surgical intervention
Chronic Inflammation
- Inflammation continues for over 2 weeks
- Characterized by macrophages and lymphocytes, not neutrophils
- Can occur from overuse injuries (shin splints, tennis elbow), when acute inflammation is unable to clear the pathogen, or due to autoimmune disorder
- May lead to tissue destruction and scar tissue formation
Adaptive Immunity
- Involves specific lymphocyte responses to an antigen
- Contact with antigen causes lymphocyte proliferation
- The immune response consists of lymphocytes and their products
- Takes longer to respond than innate immunity; develops over days
- Considered the body's third line of defense
Branches of adaptive immunity
- Cell-mediated immunity involving T-lymphocytes
- Humoral immunity involving B-lymphocytes, plasma cells and antibodies
Immune System Disorders
- Immune system lacks tolerance for a specific antigen
- Initiates immune response as if cells were foreign
- Rheumatic heart disease, type 1 diabetes, multiple sclerosis are examples
T-Lymphocytes and B-Lymphocytes
- T-lymphocytes are cells of cell mediated immunity
- B-lymphocytes are cells of humoral immunity
Organ Transplants
- Individuals are tested prior to donation for MHC antigens and ABO group
- The major histocompatibility complex (MHC) cell surface proteins allow acquired immune system to recognise foreign
Major Histocompatibility Complex (MHC)
- Tags antigens derived from pathogens and displays them on the cells surface for recognition by the appropriate T cells
- No exact duplicate MHC molecules
- Components of innate and adaptive immunity attempt to destroy transplanted tissues
- Recipients take immunosuppressant drugs
Lymphocyte Formation
- T-lymphocytes originate in red bone marrow and migrate to the thymus as pre-T lymphocytes to complete maturation
- Immunocompetent T-lymphocytes can bind antigens and respond to them
- Naive T-lymphocytes haven't yet been exposed to antigens
- Regulatory T-lymphocytes (T-Regs) are CD4+ cells formed from T cells that find self antigens and inhibit immune response
- Some tumors foster T-reg proliferation, and certain cancer treatments try to inhibit tumor T-reg
Immunoglobulins
- Antibodies are Immunoglobulins (Ig) proteins produced against a particular antigen
- Antibodies tag pathogens for destruction by immune cells
- Offer defense against viruses, bacteria, toxins, and yeast spores
- Soluble antigens are combated by humoral immunity
Antibody Functions: Neutralization
- The antibody physically covers antigenic determination of pathogen
- The pathogen is ineffective in establishing infection
- Covers regions of a virus that are used to bind to a cell receptor
Antibody Functions: Agglutination
- Antibodies cross-link antigens of foreign cells causing clumping
- Effective against bacterial cells
Antibody Functions: Precipitation
- Antibodies cross-link circulating antigens forming a complex that becomes insoluble and precipitates out of body fluids
- Precipitated complexes are engulfed and eliminated by phagocytes
Antibody Functions: Complement Fixation
- IgG and IgM can bind complement for activation (classical complement activation)
Antibody Functions: Opsonization
- Certain antibody classes make a cell more likely to be phagocytized
Antibody Functions: NK Activation
- IgG triggers NK cells to release cytotoxins
- This process creates cell mediated cytotoxicity (ADCC)
Types of Antibodies
- There are give major types of antibodies that constitute the gamma globulin fraction of the plasma
- IgG antibodies are in tissue fluid and plasma, defend against viruses, toxins, and bacterial cells, and activate complement
- IgA antibodies are in exocrine secretions and defends against foreign substances
- IgM antibodies are primarily in plasma, activates complement, and reacts with blood cells during transfusions
- IgD antibodies are on the surface of most B lymphocytes and functions in B cell activation
- IgE antibodies are in exocrine gland secretions and promote allergic reactions
Practical Classification of Immunity
- Naturally acquired active immunity is acquired by exposing the body to an antigen
- Artificially acquired active immunity is acquired by getting vaccines
- Artificially acquired passive immunity is acquired by receiving a gamma globulin
- Naturally acquired passive immunity is acquired during pregnancy when a mother passes antibodies to her fetus
Hypersensitivities
- Are abnormal and exaggerated immune responses to an antigen
- Acute hypersensitivity: reactions occur within seconds (anaphylactic)
- Subacute hypersensitivity: occur within 1-3 hours, both involve humoral immunity
- Delayed hypersensitivity: occur in 1-3 days, involve cell mediated immunity
Vaccinations
- Introduces weakened or dead organisms, or organism components
- Stimulates the immune system to develop memory B-lymphocytes
- Provides a relatively safe means for initial exposure to a microorganism
- If exposed later in life, will trigger a secondary response
- The immune system response predominantly comes from the humoral branch
- May provide either lifelong immunity or require a booster shot
Gametogenesis
- Defined as male and female reproductive systems consisting of a series of glands and tubes to produce and nurture sex cells, and transport them to the site of fertilization
Sperm and Oocytes
- Sperm cells are male sex cells
- Oocytes are female sex cells
Sperm Cell Formation
- In the male embryo, undifferentiated spermatogenic cells turn into spermatogonia; each contains 46 chromosomes
- Primary spermatocytes are formed during spermatogenesis when spermatogonia enlarges
- Secondary spermatocytes with 23 chromosomes divide from primary spermatocytes by meiosis
- The secondary spermatocytes divide again to form spermatids, each of which matures into a sperm cell
Oocyte Formation
- During prenatal development, small groups of cells form millions of primordial follicles; each has a primary oocyte and follicular cells
- The primary oocytes begin to undergo meiosis early on, but then are halted until puberty.
- 400-500 are released from the ovary during the reproductive life of the female.
Oogenesis
- At puberty, oocytes are stimulated to continue meiosis
- During meiosis, a primary oocyte matures into a secondary oocyte
- A second cytoplasmic division results in an egg cell and another polar body
Pregnancy
- Continuous process of individual changes from one life phase to another, consisting of an increase in size (growth)
- The prenatal period includes the time from fertilization to birth
- Postnatal period includes the time from birth to death
- Pregnancy is the presence of offspring developing in the uterus
Fertilization
- Sperms erode away the corona radiata and zona pellucida surrounding the secondary oocyte with the acrosomal enzyme and one sperm cell penetrates the egg cell membrane
- Penetration prevents the entry of subsequent sperm cells
- Fusion of egg and sperm nuclei is completed, resulting in a diploid zygote
Stages of Prenatal Development
- The zygote undergoes cleavage (mitosis)
- The dividing mass of cells (morula) moves down the uterine tube to the uterus, where a stage called the blastocyst implants in the lining of the uterus, marking the start of the embryonic stage
- The offspring is called an embryo during the first eight weeks and then a fetus
Pregnancy Hormones
- The trophoblast secretes human chorionic gonadotropin (hCG) to maintain the corpus luteum and thus maintain the uterine lining and the pregnancy.
Key Pregnancy Hormones
- Secreted by the trophoblast are human chorionic gonadotropin (hCG), which are sustained until the placenta is developed for hormone prodution to support pregnancy
- Also secreted by the placenta are placental lactogen for mammary gland development and secretion of estrogen
Fetal Stage
- Begins at the end of eighth week and lasts until birth.
- Structures grow and mature, and the bones ossify Maternal feeling of fetal movement occurs near the fifth month of gestation alongside hair appearance
- Last stage of fetal growth: brain cells form rapidly and organs grow and mature as the fetus increases in size.
Birth Process
- Pregnancy terminates after thirty-eight weeks
- The aging Placenta produces less progesterone which can stimulate the synthesis of prostaglandins, which can initiate labor
- Stretch of uterine tissues releases oxytocin to stimulates uterine contraction
- Fetal head stretches the cervix and stimulates positive feedback for stronger contractions and releases additional oxytocin.
- Muscles work together force baby through the birth canal, followed by placenta via uterine contractions (afterbirth)
Postnatal Period
- Mother and newborn undergo physical and physiological changes
Milk Production
- The mammary glands produce large qualities of milk after childbirth
- Colostrum (first milk) is a watery fluid that is rich in proteins and antibodies
- Sucking action of the infant releases oxytocin which triggers the release of milk
Neonatal Period
- Starts at birth and lasts for four weeks
- Forceful first breath inflates lungs for the first time
Newborn
- Surfactant in a full-term newborn reduces alveolar surface tension
- Newborns live off their fat stores for two to three days followed by mother's milk
- The newborn is susceptible to dehydration due to homeostatic mechanisms that are unable to fully conserve water
Common Elements: Male and Female Repro
- Possess primary repro organs (gonads) --Ovaries: female gonads -- Testes: male gonads
- Gonads produce sex cells (gametes) and unite during fertilization
- Gamete union initiates new individual development
Sex Hormones
- Gonads Produce sex hormones
- Affects the maturation development and activity of repro organs
- Both sexes possess accessory reproductive organs -- Female: Repro ducts bring gametes to site of fert -- Male: Repro ducts bring gametes closer body exterior
Puberty
- Occurs during adolescence -- Develop external sex characteristics
-
- Gametes become mature -- Gonads start secreting sex horones
Hormones
- Initiated when hypothalamus secretes GnRH
- GnRH stimulates anterior pit secretes two hormones: FSH LH
- The gonads begin producing significant levels of sex hormones which initiates gamete and sexual maturation
Gametes
- Prod by males and females Female prod releases a single gamete monthly (oocyte)
- Male prod large number: -- 100 million 1 day Are Stored for only short time if not released from the body Reabsorbed by body
Menopause
- Occurs once women have no cycles for one year Not associated with pregnancy or medical
- Occurs at 45-55 age range
- The ovaries produce negligible or not estrogen or progesterone production to grow or sustain the linings of the uterus
- End result-no menstruation
Tubal Pregnancy
- Occurs when fertilized oocytes implant in regions of the uterus Fertilization in uterine tube
- Embryo viable for only 8 wks (not sustainable development)
Endomitosis
- Occurs when endometrial tissues becomes displaced and implanted on external surfaces within the abdominopelvic cavity
- Causes chronic pain as tissue cannot be expelled normally
- Endometrium is sensitive to hormones
Cervial Cancer
- HPV is a leading risk factor for malignancy in female repro sys Vaccine for the 4 most common strands are recommended
Pap tests
- Detects abnormal cellular development in cervical Performed scraping cell edge to be exam Invasive or cancerous cell are removed with hysterectomy
Mammary Glands
Release Breast Milk Occurs as result interaction from both intenaland external Starts shortly after partituion
Prolactin
- Produced in the anterior Pit Responsible in milk production Results with increase Mammary gland forming greater alveriols
Oxytocin
- Results in Hypothalamus causing ejection Response from breast feeding
Pregnancy Prevention
- Abstinence (100%)
- Rhythm (25% risk): by timing intercourse to when ovulation is least likely
- Pulling Out (19% risk): pulling before ejaculation
- Barriers methods : Condoms
Lactation
- Hypthothmically suppresses FSH and LH to inhibit conception
- Intrauterine Devices: Mech device inserts into utrus
Sexual Regulation
- Hormone production -- Hypothal releases GnRH (1.stim)
- ( 2.stim) Releases FSH and LH
- FSH and LH stimulate spermatogenises LH releases interstitial for testosterone FSH release testerone for hight in testis where is bind for cell activity
Testerone
- Testerone Faciliates spermagenesis, blocks GnRH, pituitary sensitives and produces negative back effect
- Stertoial cells releases cell count (inhibin), producing more count decreasing and blocks secretions
- Testo facilitates libido development, develops sex and axillary hair, facial hair and voice
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.