Podcast
Questions and Answers
What is the primary vector responsible for transmitting Wuchereria bancrofti in most parts of Asia?
What is the primary vector responsible for transmitting Wuchereria bancrofti in most parts of Asia?
- Anopheles mosquito
- Culex quinquefasciatus (correct)
- Mansonia mosquito
- Aedes mosquito
In which of the following regions is Brugia timori primarily found?
In which of the following regions is Brugia timori primarily found?
- Malaysia
- Timor Island, Indonesia (correct)
- India
- Africa
What is the size range of adult male Wuchereria bancrofti worms?
What is the size range of adult male Wuchereria bancrofti worms?
- 2-4 cm (correct)
- 1-3 cm
- 4-10 cm
- 10-15 cm
Which of the following states in Malaysia is NOT mentioned as endemic for lymphatic filariasis?
Which of the following states in Malaysia is NOT mentioned as endemic for lymphatic filariasis?
What is the typical lifespan of an adult Wuchereria bancrofti worm?
What is the typical lifespan of an adult Wuchereria bancrofti worm?
What is the length of microfilariae of Wuchereria bancrofti?
What is the length of microfilariae of Wuchereria bancrofti?
Which of the following species of mosquitoes is responsible for transmitting Wuchereria bancrofti in Africa?
Which of the following species of mosquitoes is responsible for transmitting Wuchereria bancrofti in Africa?
Which major biological feature distinguishes female Wuchereria bancrofti from males?
Which major biological feature distinguishes female Wuchereria bancrofti from males?
What is the characteristic that distinguishes Wuchereria bancrofti from other microfilariae regarding their body nuclei?
What is the characteristic that distinguishes Wuchereria bancrofti from other microfilariae regarding their body nuclei?
When are Wuchereria bancrofti microfilariae predominantly found in peripheral blood circulation?
When are Wuchereria bancrofti microfilariae predominantly found in peripheral blood circulation?
What happens to microfilariae if they are not taken up by a female vector mosquito?
What happens to microfilariae if they are not taken up by a female vector mosquito?
Which of the following mosquitoes acts as a vector for Wuchereria bancrofti?
Which of the following mosquitoes acts as a vector for Wuchereria bancrofti?
What is the infective stage of the larva that enters the human skin when a vector mosquito takes a blood meal?
What is the infective stage of the larva that enters the human skin when a vector mosquito takes a blood meal?
Which of the following is true about the maturation of microfilariae inside the vector mosquito?
Which of the following is true about the maturation of microfilariae inside the vector mosquito?
In which anatomical site do adult Wuchereria bancrofti worms primarily reside within the human body?
In which anatomical site do adult Wuchereria bancrofti worms primarily reside within the human body?
Which stage of the Wuchereria bancrofti life cycle does the female adult worm produce?
Which stage of the Wuchereria bancrofti life cycle does the female adult worm produce?
What characterizes the chronic obstructive phase of Classical Filariasis?
What characterizes the chronic obstructive phase of Classical Filariasis?
What acute symptoms may occur during the inflammatory stage of Classical Filariasis?
What acute symptoms may occur during the inflammatory stage of Classical Filariasis?
Which condition is NOT typically associated with the chronic stage of Classical Filariasis?
Which condition is NOT typically associated with the chronic stage of Classical Filariasis?
How long does it usually take for the obstructive phase of Classical Filariasis to develop?
How long does it usually take for the obstructive phase of Classical Filariasis to develop?
Microfilariae are typically absent in which stage of Classical Filariasis?
Microfilariae are typically absent in which stage of Classical Filariasis?
What is the common name for Wuchereria bancrofti?
What is the common name for Wuchereria bancrofti?
What is the primary cause of hydrocoele in Classical Filariasis?
What is the primary cause of hydrocoele in Classical Filariasis?
Which symptom is specifically linked to the chronic stage of Classical Filariasis?
Which symptom is specifically linked to the chronic stage of Classical Filariasis?
Which of the following statements correctly describes the morphology of B. malayi?
Which of the following statements correctly describes the morphology of B. malayi?
What differentiates the periodicity of B. malayi from W. bancrofti?
What differentiates the periodicity of B. malayi from W. bancrofti?
Which of the following is a characteristic of lymphangitis in the acute stage?
Which of the following is a characteristic of lymphangitis in the acute stage?
What is the primary mode of transmission for B. malayi?
What is the primary mode of transmission for B. malayi?
Which feature distinguishes the appearance of the microfilariae of W. bancrofti from that of B. malayi?
Which feature distinguishes the appearance of the microfilariae of W. bancrofti from that of B. malayi?
What is a distinguishing characteristic of the cephalic space between W. bancrofti and B. malayi?
What is a distinguishing characteristic of the cephalic space between W. bancrofti and B. malayi?
Which clinical feature is NOT associated with Malayan Filariasis caused by B. malayi?
Which clinical feature is NOT associated with Malayan Filariasis caused by B. malayi?
How long is the typical clinical incubation period for filariasis after infection?
How long is the typical clinical incubation period for filariasis after infection?
Which patient demographic is primarily affected by Bm elephantiasis?
Which patient demographic is primarily affected by Bm elephantiasis?
What is a key clinical manifestation of occult filariasis?
What is a key clinical manifestation of occult filariasis?
Which of the following tests is useful for detecting microfilariae during daytime?
Which of the following tests is useful for detecting microfilariae during daytime?
What period of time is critical for blood collection to detect microfilariae?
What period of time is critical for blood collection to detect microfilariae?
Which condition is characterized by pulmonary symptoms and an increased eosinophil count?
Which condition is characterized by pulmonary symptoms and an increased eosinophil count?
What is the estimated eosinophil count indicative of tropical pulmonary eosinophilia?
What is the estimated eosinophil count indicative of tropical pulmonary eosinophilia?
What type of fluid is described as chylous?
What type of fluid is described as chylous?
Which serological marker is often elevated in cases of tropical pulmonary eosinophilia?
Which serological marker is often elevated in cases of tropical pulmonary eosinophilia?
Which treatment is recommended for managing elephantiasis symptoms?
Which treatment is recommended for managing elephantiasis symptoms?
What is a characteristic appearance of chylous urine?
What is a characteristic appearance of chylous urine?
What is the primary goal of the National Lymphatic Filariasis Elimination Program in Malaysia?
What is the primary goal of the National Lymphatic Filariasis Elimination Program in Malaysia?
What method is used for molecular diagnosis of filariasis?
What method is used for molecular diagnosis of filariasis?
Which of the following is a recommended treatment approach for patients diagnosed with lymphatic filariasis?
Which of the following is a recommended treatment approach for patients diagnosed with lymphatic filariasis?
What vector is associated with the transmission of Loa loa?
What vector is associated with the transmission of Loa loa?
Which preventive measure is suggested for controlling filariasis in endemic areas?
Which preventive measure is suggested for controlling filariasis in endemic areas?
What is the significance of detecting microfilaria in a patient's blood?
What is the significance of detecting microfilaria in a patient's blood?
Flashcards
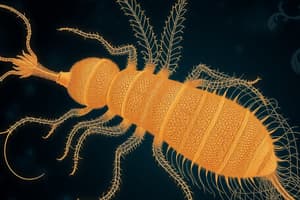
Microfilaria (Mf) W. bancrofti
Microfilaria (Mf) W. bancrofti
The microfilariae, or larval stage, of the worm Wuchereria bancrofti, found circulating in the blood.
Wuchereria bancrofti Habitat (Adult)
Wuchereria bancrofti Habitat (Adult)
The adult worm lives in the lymphatic system. It's usually found in the lower limbs, between the abdomen and thigh, and also in the upper limbs.
W. bancrofti Vector in Asia & Pacific
W. bancrofti Vector in Asia & Pacific
Aedes mosquitoes are the primary vectors of Wuchereria bancrofti in Asia and the Pacific.
W. bancrofti Vector in India & Asia
W. bancrofti Vector in India & Asia
Signup and view all the flashcards
Adult W. bancrofti Morphology
Adult W. bancrofti Morphology
Signup and view all the flashcards
Microfilaria W. bancrofti Morphology
Microfilaria W. bancrofti Morphology
Signup and view all the flashcards
Geographical Distribution of W. bancrofti
Geographical Distribution of W. bancrofti
Signup and view all the flashcards
Geographical Distribution of Brugia malayi
Geographical Distribution of Brugia malayi
Signup and view all the flashcards
Vectors of Wuchereria bancrofti
Vectors of Wuchereria bancrofti
Signup and view all the flashcards
Wuchereria bancrofti's target
Wuchereria bancrofti's target
Signup and view all the flashcards
Wuchereria bancrofti's larval form
Wuchereria bancrofti's larval form
Signup and view all the flashcards
Wuchereria bancrofti's infective stage
Wuchereria bancrofti's infective stage
Signup and view all the flashcards
Brugia malayi's target
Brugia malayi's target
Signup and view all the flashcards
Brugia malayi's larval form
Brugia malayi's larval form
Signup and view all the flashcards
Brugia malayi's infective stage
Brugia malayi's infective stage
Signup and view all the flashcards
Incubation period of filariasis
Incubation period of filariasis
Signup and view all the flashcards
Wuchereria bancrofti Adult Worm
Wuchereria bancrofti Adult Worm
Signup and view all the flashcards
Wuchereria bancrofti Microfilariae
Wuchereria bancrofti Microfilariae
Signup and view all the flashcards
Definitive Host in Wuchereria bancrofti
Definitive Host in Wuchereria bancrofti
Signup and view all the flashcards
Intermediate Host in Wuchereria bancrofti
Intermediate Host in Wuchereria bancrofti
Signup and view all the flashcards
Infective Larvae (L3) in Wuchereria bancrofti
Infective Larvae (L3) in Wuchereria bancrofti
Signup and view all the flashcards
Transmission of Wuchereria bancrofti
Transmission of Wuchereria bancrofti
Signup and view all the flashcards
Brugia malayi
Brugia malayi
Signup and view all the flashcards
Asymptomatic Phase (Classical Filariasis)
Asymptomatic Phase (Classical Filariasis)
Signup and view all the flashcards
Acute Stage (Classical Filariasis)
Acute Stage (Classical Filariasis)
Signup and view all the flashcards
Hydrocele (Classical Filariasis)
Hydrocele (Classical Filariasis)
Signup and view all the flashcards
Lymphedema (Classical Filariasis)
Lymphedema (Classical Filariasis)
Signup and view all the flashcards
Elephantiasis (Classical Filariasis)
Elephantiasis (Classical Filariasis)
Signup and view all the flashcards
Chronic Stage (Classical Filariasis)
Chronic Stage (Classical Filariasis)
Signup and view all the flashcards
Chyluria (Classical Filariasis)
Chyluria (Classical Filariasis)
Signup and view all the flashcards
Lymphangiovarix (Classical Filariasis)
Lymphangiovarix (Classical Filariasis)
Signup and view all the flashcards
Occult Filariasis
Occult Filariasis
Signup and view all the flashcards
Meyers Kouwenaar Syndrome
Meyers Kouwenaar Syndrome
Signup and view all the flashcards
Massive Eosinophilia
Massive Eosinophilia
Signup and view all the flashcards
Hepatosplenomegaly
Hepatosplenomegaly
Signup and view all the flashcards
DEC Provocation Test
DEC Provocation Test
Signup and view all the flashcards
Adult Worms in Lymph Node Biopsy
Adult Worms in Lymph Node Biopsy
Signup and view all the flashcards
Tropical Pulmonary Eosinophilia
Tropical Pulmonary Eosinophilia
Signup and view all the flashcards
Chest X-ray Showing Mottled Shadows
Chest X-ray Showing Mottled Shadows
Signup and view all the flashcards
ELISA for lymphatic filariasis
ELISA for lymphatic filariasis
Signup and view all the flashcards
Immunochromatographic test (ICT) for lymphatic filariasis
Immunochromatographic test (ICT) for lymphatic filariasis
Signup and view all the flashcards
Molecular diagnosis using PCR for lymphatic filariasis
Molecular diagnosis using PCR for lymphatic filariasis
Signup and view all the flashcards
Drug combination therapy for lymphatic filariasis
Drug combination therapy for lymphatic filariasis
Signup and view all the flashcards
Lymphedema in lymphatic filariasis
Lymphedema in lymphatic filariasis
Signup and view all the flashcards
Chylous urine in lymphatic filariasis
Chylous urine in lymphatic filariasis
Signup and view all the flashcards
National Lymphatic Filariasis Elimination Program in Malaysia
National Lymphatic Filariasis Elimination Program in Malaysia
Signup and view all the flashcards
Medical management of chyluria in lymphatic filariasis
Medical management of chyluria in lymphatic filariasis
Signup and view all the flashcards
Study Notes
Tissue & Body Fluid Nematode
- Helminths are multicellular parasites.
- Helminths are divided into Nemathelminths (roundworms), Platyhelminths (flatworms).
- Class Nematoda includes roundworms.
- Class Trematoda includes flukes.
- Class Cestoda includes tapeworms.
Helminthology
- Helminths (worms) are multicellular parasites.
- They are divided into: Nemathelminths (round worms), Platyhelminths (flat worms).
- Class Nematoda: roundworms
- Intestinal nematodes (large intestine, small intestine)
- Tissue nematodes (Filarial worms)
- Class Trematoda (flukes):
- Blood trematodes
- Hepatic trematodes
- Intestinal trematodes
- Lung trematodes
- Class Cestoda (tapeworms):
- Intestinal cestodes
- Somatic/tissue cestodes
- Class Nematoda: roundworms
Differences between Cestodes, Trematodes, and Nematodes
- Cestodes (Tapeworms):
- Shape: Tape-like and segmented
- Head end: Suckers present; some have hooklets
- Alimentary canal: Absent
- Body cavity: Absent
- Sexes: Monoecious (except some species)
- Life cycle: Requires two hosts (except some species)
- Larva forms: Cysticercus, hydatid cyst, coenurus, cysticercoid, coracidium, plerocercoid, and procercoid
- Trematodes (Flukes):
- Shape: Leaf-like and unsegmented
- Head end: Suckers present; no hooklets
- Alimentary canal: Present but incomplete
- Body cavity: Absent
- Sexes: Monoecious (except schistosomes)
- Life cycle: Requires three hosts (except schistosomes)
- Larva forms: Cercaria, metacercaria, redia, miracidium, and sporocyst
- Nematodes (Roundworms):
- Shape: Elongated, cylindrical, and unsegmented
- Head end: No sucker, no hooklets; some have well-developed buccal capsules.
- Alimentary canal: Complete from mouth to anus
- Body cavity: Present
- Sexes: Diecious (except filarial worms and Dracunculus)
- Life cycle: Requires one host (except filarial worms and Dracunculus)
- Larva forms: Rhabditiform larva, filariform larva, and microfilaria.
Filarial
- Infection by filarial worms belonging to superfamily Filarioidea.
- Classified according to adult worm body location.
- Lymphatic filariasis
- Subcutaneous filariasis
- Serous cavity filariasis
- Types: Wuchereria bancrofti, Brugia malayi, Brugia timori
Lymphatic Filariasis
- Also known as elephantiasis.
- Painful, disfiguring swelling of the legs and genital organs (classic late-stage sign).
- Caused by filarial worms.
- Transmitted by mosquitoes carrying filarial worm infective larvae.
- Vectors: mosquito
- Species depends on geographical area.
- Common in developing countries.
- Three species of human filarial worms are found.
- In Malaysia only B. malayi & W. bancrofti are found.
- Endemic in 8 Malaysian states.
- Prevalent in tropical and sub-tropical areas with many mosquito vectors.
- Incidence in Malaysia decreasing due to effective control programs.
Morphology-Wuchereria bancrofti
- Adult worms: whitish, thread-like, smooth cuticle, tapering ends; female (4–10 cm) larger than male (2–4 cm); lifespan 10–15 years.
- Found in lymphatic vessels and lymph nodes.
- Embryos (microfilariae Mf): 250–300 µm length; colorless, transparent; blunt heads and pointed tails; covered by hyaline sheath; active movement; discrete, countable body nuclei; no terminal nuclei; short cephalic ratio (1:1); present in peripheral blood.
- Nocturnal periodicity (between 22:00 and 02:00); not in blood during day time.
- Microfilariae do not multiply in human body; they die if not taken by a female mosquito.
Morphology-Brugia malayi
- Adult worms are similar to W. bancrofti but smaller in size (53mm female, 24mm male).
- Microfilariae: tail has two distinct terminal nuclei (subterminal & terminal); released into bloodstream; kinky, cephalic space is longer (ratio is 2:1)
- Sheath is stained, overlapping body nuclei.
Morphology-Brugia timori
- Endemic in Timor Island, Indonesia.
- Microfilariae larger than those of B. malayi; sheath does not stain with Giemsa stain; 5–8 nuclei present in tail.
- Lesions are milder.
Morphology-Loa-loa
- Loa-loa is also known as African eyeworm.
- Causes loiasis (fugitive swellings).
- Vectors: Day-biting flies, Chrysops.
- Microfilariae is sheathed, and nuclei extend up to tail tip.
- Microfilariae appears during the day (diurnal periodic).
Morphology-Onchocerca volvulus
- Produces onchocerciasis ("river blindness").
- Adult worm is white, with transverse striations on cuticle, curved posterior end.
- Microfilariae is unsheathed, tail-tip free of nuclei, nonperiodic.
- Definitive host: Humans.
- Intermediate host: Female black flies (Simulium).
Morphology-Mansonella streptocerca
- Seen only in West Africa.
- Adult worms live in the dermis, just under the skin surface; unsheathed microfilariae found in skin.
- Vectors: Culicoides species.
- Reservoir hosts: Chimpanzees.
- Infection: dermatitis with pruritus and hypopigmented macules.
- Diagnosis: microfilariae in skin clippings.
- Treatment: Ivermectin.
Morphology-Mansonella ozzardi
- New World filaria, seen in Central and South America and the West Indies.
- Adult worms in peritoneal and pleural cavities of humans.
- Nonperiodic, unsheathed microfilariae in blood.
- Vectors: Culicoides species.
- Infection is asymptomatic, except for possible transient abdominal pain, rashes, angioedema, and malaise.
Morphology-Mansonella perstans
- Extensively distributed in tropical Africa and coastal South America, adult worms in body cavities (mainly peritoneum and often in the pleura).
- Unsheathed and subperiodic microfilaria.
- Vectors: Culicoides species; reservoir hosts are African primates
- Infection generally asymptomatic, possible transient abdominal pain, rashes, angioedema, and malaise.
- Diagnosis: microfilaria detected in the peripheral blood or serosal effusions; Treatment: Doxycycline.
Life Cycle- filarial worms
- Infective larvae enter the human skin through mosquito bites.
- Develop into adult worms in the lymphatic system.
- Adult female worms produce sheathed microfilariae that migrate into lymphatic and blood channels.
- When the vector mosquito takes a blood meal, it ingests the microfilariae.
- Microfilariae shed sheaths, penetrate the mosquito's midgut and migrate to thoracic muscles.
- Develop into L1 larva.
- Molts twice and develops into L3 larva.
- L3 larvae migrate to heads and proboscis, infecting another human when the mosquito takes a blood meal.
Treatment
- Medication: DEC and Albendazole (in combination)
- Surgical for hydrocele (rarely successful), elephantine legs: elevation, elastic bandages, foot care.
- Special boots or elastic bandages to reduce enlarged limb size
- Medical management of chyluria: bed rest, high protein diet, and treatment with DEC.
Prevention & Control
- National Lymphatic Filariasis Elimination Program (Malaysia): mass drug administration (annual, 5 cycles) in endemic areas; health education (community knowledge, healthy lifestyle, personal hygiene).
- Blood screening and probe study to identify new endemic areas, chemotherapy in endemic areas.
- Vector control: spraying, treated nets for periodic infections, adding larvae-eating fish to ponds.
- Proper clothing, use of repellents to avoid contact with vectors
Laboratory Diagnosis
- Microscopic examination of blood smears (thick and thin, Giemsa or H&E); blood collection at night (10 pm–2 am) for microfilaria detection.
- Concentration techniques (centrifugation, filtration through Nucleopore membrane).
- Detection of adult worms in lymph node biopsies.
- Serological tests (ELISA, immunochromatographic test [ICT]).
- Molecular diagnosis (PCR) to detect filarial DNA in blood.
- Chylous urine (milky appearance), as well as hydrocele fluid.
Clinical Manifestations of Classical Filariasis
- Asymptomatic: microfilariae present in blood in endemic areas; no clinical signs.
- Acute (inflammatory): fever, malaise, headache, chills, lymphadenitis, lymphangitis, lymphoedema.
- Chronic (obstructive): 10-15 years, hydrocele (swelling of scrotum, fluid accumulation in testes), lymphedema (swelling of upper and lower extremities), elephantiasis (enlargement and thickening of lower and/or upper extremities, scrotum, breasts), Lymphangiovarix (lymph vessel dilation), chyluria (lymph in urine).
Pathogenesis
- Depends on the host's immune system and inflammatory responses.
- Infection of W. bancrofti-Wuchereriasis or bancroftian filariasis.
- Brugia malayi causes brugian/malayan filariasis, similar to bancroftian filariasis, but there is no chyluria and no involvement of male genitalia; usually restricted to the legs.
Pathogenesis of Occult Filariasis
- Also known as Meyers Kouwenaar syndrome, it's a hypersensitivity reaction to microfilarial antigens, not due to lymphatic involvement.
- Microfilariae are not found in blood (destroyed by allergic inflammation in tissues).
- Features: massive eosinophilia, hepatosplenomegaly, pulmonary symptoms (dry cough, dyspnea, wheezing).
- Occurs as a result of hypersensitivity to microfilarial antigens.
- Also include arthritis, glomerulonephritis, thrombophlebitis, and tenosynovitis.
- Absence of classical lymphatic filariasis features.
- Common in tropical pulmonary eosinophilia with low-grade fever, weight loss, dry nocturnal cough, dyspnea, asthmatic wheezing, marked increase in eosinophils (>3000 µm, up to 50,000 or more).
- Chest X-ray shows mottled shadows, similar to miliary tuberculosis, elevated serum IgE (>1000 IU/mL), filarial antibodies.
Questions
- Listed topics include discussing lymphatic filariasis, endemic lymphatic filariasis in Malaysia (types and vectors, periodicity, pathogenesis, and clinical manifestations) and discussing lymphatic filariasis (diagnosis, and prevention)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.