Podcast
Questions and Answers
A patient presents with weakness in hip adduction and difficulty with knee joint stability. Sensory examination reveals altered sensation on the proximal medial thigh. Which nerve is MOST likely affected?
A patient presents with weakness in hip adduction and difficulty with knee joint stability. Sensory examination reveals altered sensation on the proximal medial thigh. Which nerve is MOST likely affected?
- Lateral femoral cutaneous
- Obturator (correct)
- Common fibular
- Sciatic
Following a hip replacement surgery, a patient reports numbness and tingling along the lateral aspect of their thigh. Which nerve is MOST likely to have been injured during the procedure?
Following a hip replacement surgery, a patient reports numbness and tingling along the lateral aspect of their thigh. Which nerve is MOST likely to have been injured during the procedure?
- Lateral femoral cutaneous (correct)
- Obturator
- Sciatic
- Tibial
An athlete is diagnosed with a hamstring strain. Which nerve could potentially be affected, leading to weakness in knee flexion?
An athlete is diagnosed with a hamstring strain. Which nerve could potentially be affected, leading to weakness in knee flexion?
- Obturator nerve
- Common fibular nerve
- Sciatic nerve (correct)
- Tibial nerve
A patient reports difficulty with dorsiflexion of the foot after a knee injury. Sensation is diminished on the anterior aspect of the lower leg and the dorsum of the foot. Which nerve is MOST likely involved?
A patient reports difficulty with dorsiflexion of the foot after a knee injury. Sensation is diminished on the anterior aspect of the lower leg and the dorsum of the foot. Which nerve is MOST likely involved?
A patient presents with paresthesia on the lateral aspect of their leg and foot, but maintains the ability to evert their foot. Which nerve is MOST likely affected?
A patient presents with paresthesia on the lateral aspect of their leg and foot, but maintains the ability to evert their foot. Which nerve is MOST likely affected?
Following a fracture of the fibular head, a patient experiences foot drop (inability to dorsiflex) and sensory loss in the web space between the first and second toes. Which nerve is MOST likely injured?
Following a fracture of the fibular head, a patient experiences foot drop (inability to dorsiflex) and sensory loss in the web space between the first and second toes. Which nerve is MOST likely injured?
Which of the following conditions would MOST likely result from compression of the tibial nerve within the tarsal tunnel?
Which of the following conditions would MOST likely result from compression of the tibial nerve within the tarsal tunnel?
A patient experiences weakness in plantarflexion and inversion of the foot, along with sensory loss on the plantar surface. Which nerve is MOST likely affected?
A patient experiences weakness in plantarflexion and inversion of the foot, along with sensory loss on the plantar surface. Which nerve is MOST likely affected?
Following a peripheral nerve injury where the axon is severed but the endoneurial tube remains intact, what is the most likely prognosis for recovery, and why?
Following a peripheral nerve injury where the axon is severed but the endoneurial tube remains intact, what is the most likely prognosis for recovery, and why?
What is the primary mechanism by which compression of a peripheral nerve leads to segmental demyelination?
What is the primary mechanism by which compression of a peripheral nerve leads to segmental demyelination?
In Wallerian degeneration, what happens to the segment of the nerve fiber distal to the injury site?
In Wallerian degeneration, what happens to the segment of the nerve fiber distal to the injury site?
Why is surgical attachment of the proximal and distal ends of the endoneurium considered important in cases of nerve severance?
Why is surgical attachment of the proximal and distal ends of the endoneurium considered important in cases of nerve severance?
Which of the following is an internal cause of peripheral nerve compression?
Which of the following is an internal cause of peripheral nerve compression?
How does damage to autonomic nerve fibers contribute to persistent edema following a peripheral nerve lesion?
How does damage to autonomic nerve fibers contribute to persistent edema following a peripheral nerve lesion?
Why do contractures develop in muscles affected by peripheral nerve lesions?
Why do contractures develop in muscles affected by peripheral nerve lesions?
What is a key difference between the symptoms of causalgia and typical pain associated with peripheral nerve lesions?
What is a key difference between the symptoms of causalgia and typical pain associated with peripheral nerve lesions?
Why is direct palpation of a nerve generally contraindicated in cases of axonotmesis or neurotmesis?
Why is direct palpation of a nerve generally contraindicated in cases of axonotmesis or neurotmesis?
What is the primary focus when treating nerve compression/entrapment (neuropraxia)?
What is the primary focus when treating nerve compression/entrapment (neuropraxia)?
A patient presents with atrophy, flaccidity, and sensory loss in their lower arm following a traumatic injury. Which treatment approach should be avoided initially?
A patient presents with atrophy, flaccidity, and sensory loss in their lower arm following a traumatic injury. Which treatment approach should be avoided initially?
When treating edema proximal to a nerve lesion, which technique is MOST appropriate?
When treating edema proximal to a nerve lesion, which technique is MOST appropriate?
What is the recommended timing for initiating direct treatment at the lesion site following a nerve injury and subsequent regeneration?
What is the recommended timing for initiating direct treatment at the lesion site following a nerve injury and subsequent regeneration?
In the context of peripheral nerve regeneration, what is the purpose of using segmental techniques proximal to the lesion?
In the context of peripheral nerve regeneration, what is the purpose of using segmental techniques proximal to the lesion?
Which presentation is MOST indicative of a nerve injury (axonotmesis or neurotmesis) rather than a nerve compression (neuropraxia)?
Which presentation is MOST indicative of a nerve injury (axonotmesis or neurotmesis) rather than a nerve compression (neuropraxia)?
What is the rationale behind using the ulnar border of the hand proximal to a nerve lesion for 'blocking'?
What is the rationale behind using the ulnar border of the hand proximal to a nerve lesion for 'blocking'?
A patient presents with an inability to wrinkle their forehead and difficulty closing one eye. Which cranial nerve is MOST likely affected?
A patient presents with an inability to wrinkle their forehead and difficulty closing one eye. Which cranial nerve is MOST likely affected?
A patient reports numbness and tingling in the skin over the lateral thigh. Which nerve is MOST likely involved?
A patient reports numbness and tingling in the skin over the lateral thigh. Which nerve is MOST likely involved?
Weakness in wrist extension is observed during a neurological examination. Which nerve is MOST likely affected?
Weakness in wrist extension is observed during a neurological examination. Which nerve is MOST likely affected?
A patient has difficulty with fine motor movements and sensory loss in the tips of the index and middle fingers. Which nerve is MOST likely compressed?
A patient has difficulty with fine motor movements and sensory loss in the tips of the index and middle fingers. Which nerve is MOST likely compressed?
During an upper limb assessment, a therapist notes atrophy of the thenar eminence. This finding is MOST likely related to damage of which nerve?
During an upper limb assessment, a therapist notes atrophy of the thenar eminence. This finding is MOST likely related to damage of which nerve?
A patient exhibits a 'claw hand' deformity affecting all digits. Which neurological structure is MOST likely involved?
A patient exhibits a 'claw hand' deformity affecting all digits. Which neurological structure is MOST likely involved?
A patient consistently holds their arm adducted and internally rotated. What is this presentation commonly referred to as?
A patient consistently holds their arm adducted and internally rotated. What is this presentation commonly referred to as?
A patient presents with tingling sensations in their hands and feet, but no noticeable muscle weakness or atrophy. Based on this information, which type of neuropathy is most likely?
A patient presents with tingling sensations in their hands and feet, but no noticeable muscle weakness or atrophy. Based on this information, which type of neuropathy is most likely?
A patient demonstrates weakness in finger abduction and adduction. Which nerve is MOST likely affected?
A patient demonstrates weakness in finger abduction and adduction. Which nerve is MOST likely affected?
Which of the following clinical presentations would suggest damage to the autonomic nervous system?
Which of the following clinical presentations would suggest damage to the autonomic nervous system?
A patient reports sharp, shooting pain in the face triggered by chewing or touching their face. Which condition is MOST likely?
A patient reports sharp, shooting pain in the face triggered by chewing or touching their face. Which condition is MOST likely?
Following a nerve injury, a patient experiences Wallerian degeneration. Which of the following accurately describes this process?
Following a nerve injury, a patient experiences Wallerian degeneration. Which of the following accurately describes this process?
A patient has a nerve injury characterized by segmental demyelination and mild ischemia, resulting in weakness but no atrophy. Which type of nerve injury is most likely?
A patient has a nerve injury characterized by segmental demyelination and mild ischemia, resulting in weakness but no atrophy. Which type of nerve injury is most likely?
Following a fracture of the humerus, a patient is unable to extend their elbow against gravity. Which nerve is MOST likely injured?
Following a fracture of the humerus, a patient is unable to extend their elbow against gravity. Which nerve is MOST likely injured?
A construction worker has an accident at work, resulting in a deep laceration and complete severance of the ulnar nerve at the wrist. What is the MOST appropriate initial intervention?
A construction worker has an accident at work, resulting in a deep laceration and complete severance of the ulnar nerve at the wrist. What is the MOST appropriate initial intervention?
Which nerve injury classification is characterized by axonal damage, but with the endoneurium, perineurium, and epineurium remaining intact?
Which nerve injury classification is characterized by axonal damage, but with the endoneurium, perineurium, and epineurium remaining intact?
A patient is diagnosed with axonotmesis after a prolonged period of nerve compression. What clinical findings would be MOST expected?
A patient is diagnosed with axonotmesis after a prolonged period of nerve compression. What clinical findings would be MOST expected?
Following a crush injury, a patient is diagnosed with neurotmesis of the tibial nerve. Besides surgical intervention, what additional long-term complication should the therapist anticipate?
Following a crush injury, a patient is diagnosed with neurotmesis of the tibial nerve. Besides surgical intervention, what additional long-term complication should the therapist anticipate?
A patient presents with muscle weakness, fasciculations, and cramping. Nerve conduction studies reveal demyelination in multiple motor nerves but sensory nerves are unaffected. What condition is most likely?
A patient presents with muscle weakness, fasciculations, and cramping. Nerve conduction studies reveal demyelination in multiple motor nerves but sensory nerves are unaffected. What condition is most likely?
A patient with suspected nerve damage undergoes electrodiagnostic testing. The results show reduced nerve conduction velocity but normal compound muscle action potential (CMAP) amplitude. Which nerve injury is more likely?
A patient with suspected nerve damage undergoes electrodiagnostic testing. The results show reduced nerve conduction velocity but normal compound muscle action potential (CMAP) amplitude. Which nerve injury is more likely?
A patient presents with weakness in plantarflexion and inversion, along with sensory loss on the plantar aspect of the foot. Which nerve is MOST likely affected?
A patient presents with weakness in plantarflexion and inversion, along with sensory loss on the plantar aspect of the foot. Which nerve is MOST likely affected?
Which muscle is innervated by both the sciatic nerve and the obturator nerve?
Which muscle is innervated by both the sciatic nerve and the obturator nerve?
A patient exhibits foot drop and difficulty with eversion. Sensation is diminished on the dorsum of the foot and between the first and second toes. Which nerve is MOST likely compromised?
A patient exhibits foot drop and difficulty with eversion. Sensation is diminished on the dorsum of the foot and between the first and second toes. Which nerve is MOST likely compromised?
Which of the following is the MOST severe nerve injury, characterized by complete severance of the nerve with disruption of the axon and surrounding connective tissues?
Which of the following is the MOST severe nerve injury, characterized by complete severance of the nerve with disruption of the axon and surrounding connective tissues?
A patient reports pain radiating down the posterior aspect of their leg, with paresthesia in the foot. Symptoms are exacerbated by sitting. Which condition is MOST likely affecting the sciatic nerve?
A patient reports pain radiating down the posterior aspect of their leg, with paresthesia in the foot. Symptoms are exacerbated by sitting. Which condition is MOST likely affecting the sciatic nerve?
Which of the following nerve injuries is characterized by demyelination, resulting in a temporary conduction block, but with preserved axonal continuity?
Which of the following nerve injuries is characterized by demyelination, resulting in a temporary conduction block, but with preserved axonal continuity?
Which assessment would be MOST appropriate to evaluate a patient suspected of having thoracic outlet syndrome (TOS) affecting the brachial plexus?
Which assessment would be MOST appropriate to evaluate a patient suspected of having thoracic outlet syndrome (TOS) affecting the brachial plexus?
Which motor function would be MOST affected by damage to the common fibular nerve?
Which motor function would be MOST affected by damage to the common fibular nerve?
Flashcards
Motor Neuropathy
Motor Neuropathy
Damage to motor nerves, leading to muscle weakness, paralysis, atrophy, and reduced reflexes.
Sensory Neuropathy
Sensory Neuropathy
Disturbance of sensory nerves, causing tingling, abnormal sensations, pain, or numbness.
Autonomic Neuropathy
Autonomic Neuropathy
Dysfunction of autonomic nerves, leading to blood pressure changes, sweating abnormalities, or bowel issues.
Mixed Neuropathy
Mixed Neuropathy
Signup and view all the flashcards
Neuropraxia
Neuropraxia
Signup and view all the flashcards
Axonotmesis
Axonotmesis
Signup and view all the flashcards
Neurotmesis
Neurotmesis
Signup and view all the flashcards
Wallerian Degeneration
Wallerian Degeneration
Signup and view all the flashcards
Neuropraxia Cause
Neuropraxia Cause
Signup and view all the flashcards
Axonotmesis Cause
Axonotmesis Cause
Signup and view all the flashcards
Peripheral Nerve Regeneration
Peripheral Nerve Regeneration
Signup and view all the flashcards
Segmental Demyelination
Segmental Demyelination
Signup and view all the flashcards
Causes of Peripheral Nerve Lesions
Causes of Peripheral Nerve Lesions
Signup and view all the flashcards
Compression Nerve Lesions
Compression Nerve Lesions
Signup and view all the flashcards
Symptoms of Peripheral Nerve Lesions
Symptoms of Peripheral Nerve Lesions
Signup and view all the flashcards
Edema with Nerve Lesions
Edema with Nerve Lesions
Signup and view all the flashcards
Altered Tissue Health
Altered Tissue Health
Signup and view all the flashcards
Lateral Femoral Cutaneous Nerve
Lateral Femoral Cutaneous Nerve
Signup and view all the flashcards
Obturator Nerve
Obturator Nerve
Signup and view all the flashcards
Sciatic Nerve
Sciatic Nerve
Signup and view all the flashcards
Tibial Nerve
Tibial Nerve
Signup and view all the flashcards
Common Fibular Nerve
Common Fibular Nerve
Signup and view all the flashcards
Cutaneous Nerve Dysfunction
Cutaneous Nerve Dysfunction
Signup and view all the flashcards
Motor Nerve Dysfunction
Motor Nerve Dysfunction
Signup and view all the flashcards
Common Fibular Nerve Injury Site
Common Fibular Nerve Injury Site
Signup and view all the flashcards
Traction on regenerating nerve?
Traction on regenerating nerve?
Signup and view all the flashcards
Edema treatment near nerve injury?
Edema treatment near nerve injury?
Signup and view all the flashcards
Segmental techniques?
Segmental techniques?
Signup and view all the flashcards
Nerve 'blocking'?
Nerve 'blocking'?
Signup and view all the flashcards
Working on lesion site?
Working on lesion site?
Signup and view all the flashcards
Treatment of weakened muscles?
Treatment of weakened muscles?
Signup and view all the flashcards
PROM direction?
PROM direction?
Signup and view all the flashcards
Neuropraxia treatment?
Neuropraxia treatment?
Signup and view all the flashcards
Adson's Test
Adson's Test
Signup and view all the flashcards
Tic Douloureux
Tic Douloureux
Signup and view all the flashcards
Bell's Palsy
Bell's Palsy
Signup and view all the flashcards
Erb's Palsy
Erb's Palsy
Signup and view all the flashcards
Klumpke's Paralysis
Klumpke's Paralysis
Signup and view all the flashcards
Ape Hand
Ape Hand
Signup and view all the flashcards
Oath Hand
Oath Hand
Signup and view all the flashcards
Cheiralgia Paresthetica
Cheiralgia Paresthetica
Signup and view all the flashcards
Saturday Night Palsy
Saturday Night Palsy
Signup and view all the flashcards
Wrist Drop
Wrist Drop
Signup and view all the flashcards
Ulnar Claw
Ulnar Claw
Signup and view all the flashcards
Study Notes
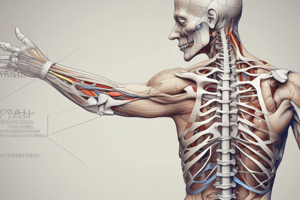
- The peripheral nervous system (PNS) includes all neural structures outside the brain and spinal cord.
- The PNS includes sensory receptors, peripheral nerves, associated ganglia, and efferent motor endings.
- The PNS links to the outside world by receiving and responding to stimuli via afferent and efferent nerves
- Peripheral nerves are supported and covered by three connective tissue layers: endoneurium, perineurium, and epineurium.
- Endoneurium surrounds each axon and is the innermost layer.
- Perineurium surrounds groups of neurons (fascicles) and is the middle layer.
- Epineurium surrounds the entire nerve and is the outermost layer.
- Myelinated nerves are larger in diameter and have an extra membrane for electrical insulation, speeding nerve impulse conduction.
- Unmyelinated nerves are smaller in diameter and lack the extra membrane, resulting in slower conduction time.
Terminology
- Neuropathy: functional disturbance and/or pathological change in nerve function.
- Neuralgia: Pain in the distribution of nerves generally in the absence of objective signs/structural damage to nerve.
- Neuritis: Inflammation of the nerve.
- Neuroma: Overgrowth of nerve cells.
- Radiculitis: Inflammation of a spinal nerve root.
- Radiculopathy: Compression of a nerve root, causing numbness and/or weakness.
- Polyradiculopathy: Affecting more than 1 nerve root.
- Plexopathy: Disorder involving one of the major neural plexuses – cervical, brachial, or lumbosacral.
- Fasciculation: Spontaneous contraction of muscle fibers in denervated tissue.
- Flaccidity: Paralysis in which muscle tone is lacking in the affected muscles, and tendon reflexes are decreased or absent.
- Atrophy: Decrease in size or wasting away of a body part or tissue.
- Double Crush Syndrome: Nerve compressed or injured in more than one location, like median nerve compression at the carpal tunnel and pronator teres.
- Peripheral nerves serve motor, sensory and autonomic functions, so neuropathies present differently based on the affected nerve type.
Motor Neuropathy
- Results in weakness, flaccid paralysis, atrophy, and decreased reflexes.
Sensory Neuropathy
- Results in paresthesias (tingling, prickling), dysesthesias (abnormal sensation), pain, and numbness.
Autonomic Neuropathy
- Results in hypotension (BP), anhidrosis (reduced sweating), diaphoresis (excessive sweating), diarrhea/constipation.
Mixed Neuropathy
- Presents as a combination of any of the above.
Nerve Injuries
- Neuropraxia involves compression of a nerve with no structural damage to the axon or distal tissue.
- In neuropraxia, the endo, peri & epineurium are intact, and the axon is preserved.
- Neuropraxia involves some myelin loss (segmental demyelination), reducing action potential conduction.
- Neuropraxia often follows nerve compression, causing mild ischemia of the nerve fiber.
- Neuropraxia results in mild weakness up to paresis/paralysis, without atrophy, and full recovery.
- Axonotmesis involves damage to the axon, but the epi, peri & endoneurium remain intact.
- Wallerian Degeneration, or axonal degeneration distal to the lesion, occurs
- Results in paresis/paralysis, with atrophy
- Axonotmesis often occurs after severe or prolonged compression, and prognosis for recovery is variable.
- Neurotmesis is complete severance of the axon and disruption of the endo, peri & epineurium.
- Wallerian Degeneration, or axonal degeneration distal to the lesion, occurs
- Neurotmesis often occurs after gunshot or stab wounds, or avulsion injuries.
- Neurotmesis requires surgical intervention for any neural re-growth.
- Neurotmesis results in paresis/paralysis, with atrophy, and recovery is incomplete.
- Peripheral nerves can regenerate even if the axon is damaged if the cell body is intact.
- In axonotmesis, the intact endoneurial tube provides a good pathway for nerve regeneration.
- Compression on a nerve causes myelin breakdown, exposing the axon and stimulating remaining Schwann cells to reproduce and form more myelin.
- Axonal Degeneration/Wallerian Degeneration
- The degeneration of an axon distal to a site of lesion.
- The segment between the nerve cell body and the site of injury remains intact.
- Proximal and distal ends of the endoneurium are surgically attached for better outcomes.
- The axon continues to re-grow until it reaches a muscle or sensory receptor.
Causes of Peripheral Nerve Lesions
- Compression: Internal (bony callus, tight muscles, tumor, edema) or External (crutches, casts).
- Trauma: Crush injuries, severance (knife, bullet), industrial accidents, or birth trauma.
- Systemic Disorders: Leprosy
- Systemic Edematous Conditions: Pregnancy, hypothyroidism, diabetes, kidney & heart conditions.
Common Symptoms of Peripheral Nerve Lesions
- Edema: Occurs due to injury-related inflammation, and persists if autonomic nerve fibers are damaged.
- Altered tissue health: Results from loss of autonomic function, causing changes to skin, hair, and nails (trophic changes).
- Altered motor function: Flaccid paralysis and muscle wasting within 3 weeks, fibrillation of denervated tissue a few weeks post-injury, and diminished deep tendon reflexes.
- Holding patterns: Limb positions such as wrist drop or claw hand may be present, depending on severity.
- Contractures: Develop due to unopposed antagonist muscles.
- Pain: Can develop into Causalgia or RSD (Reflex sympathetic dystrophy).
Management Guidelines for Peripheral Nerve Injury Recovery
- Acute Phase: Focus on healing and preventing complications through immobilization (time dictated by MD) and splinting/bracing to prevent deformities.
- Recovery Phase: Emphasize retraining and re-education when reinnervation occurs, including motor retraining (holding muscle in shortened position), desensitization (stroking skin with different textures), and discriminative sensory re-education (object identification with/without visual cues).
- Chronic Phase: Focus on training compensatory function when recovery plateaus with significant physical deficits, and splint/brace wearing may continue.
Muscle Weakness
- Neurogenic weakness is distal to proximal, fasciculations may be present, reflexes are diminished, and sensory signs/symptoms may be present.
- Myogenic weakness is proximal to distal, no fasciculations, reflexes are often preserved and no sensory signs.
Precautions & Treatment Considerations for Regenerating Lesions
- Do not traction a regenerating nerve.
- Treat edema with elevation, nodal pumping & drainage techniques, proximal to the edge of the edema.
- Use segmental techniques proximal to the lesion, applied at right angles to the direction of the regenerating nerve.
- Consider "blocking" with the ulnar border of the hand, just proximal to the lesion, to prevent drag on the healing tissue.
- Avoid work on lesion site until regeneration has passed (approx. 2 weeks post-trauma or 3 weeks post-surgery).
- Treat flaccid or weakened muscles distal to the lesion with light strokes & gentle compressions.
- PROM can be used to affect joints in the direction that shortens the affected tissue & nerve.
- Treatment of nerve compression/entrapment (neuropraxia) is different from treatment for nerve injuries (axonotmesis, neurotmesis).
- Neuropraxia (non-degenerative condition) presents with paresthesia, dysesthesia, pain, mild weakness, and nerve palpation is indicated.
- Axonotmesis/Neurotmesis (degenerative condition) is indicated when there is atrophy, flaccidity, significant weakness/paresis/paralysis, sensory loss, and palpation of the nerve is not indicated.
- Simple compressions or entrapments without tissue damage require releasing compression at the compression site for treatment.
- The precautions apply to degenerative conditions.
Assessment Considerations
- Acute injuries and regenerating tissue must be handled with extreme caution, and MD/Neurologist confirmation is needed for movement assessment & treatment.
- Palpation: Compare bilaterally for muscle bulk (atrophy), sweating (anhidrosis/diaphoresis), and edema.
- ROM testing: Avoid actions that traction/stretch a regenerating nerve; ROM testing can be used on the affected muscles.
- PROM: Can be used with a regenerating nerve to assess contracture of unopposed antagonistic muscles, as long as the motion does not traction or stretch the regenerating nerve.
- AAROM Can be used with minimal assistance provided by a therapist.
- Deep Tendon Reflexes diminish with a partial lesion (hyporeflexia); hyperreflexia may be indicative of an upper motor neuron lesion.
- Sensory Testing: Dysfunction appears in the affected nerve's normal function. Types of sensory testing include deep & light touch, 2 point discrimination, piloerector response and temperature.
Nerve Root Compression vs. Peripheral Nerve Lesion
-
Nerve root compression causes altered sensation in a dermatome pattern
-
Assess the corresponding myotome to determine muscle function
-
Nerve roots are part of the PNS.
-
Cutaneous nerves are C-fibers that respond to thermal, mechanical, and chemical stimuli, producing dull, diffuse, aching, burning, and delayed pain.
-
During palpation: consider the nerve's referral pattern
-
Nerves may feel like tight bands/wires/nodules in tissue
-
If a nerve is compressed/tractioned/suffering a chemical imbalance, it may become swollen due to intraneural edema.
-
The key points for muscles and skin for the various cranial and spinal nerves include
-
Cranial Nerve 5
-
Cranial Nerve 7
-
Brachial Plexus
-
Median Nerve
-
Radial Nerve
-
Ulnar Nerve
-
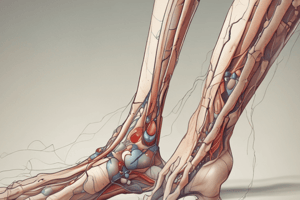
Lateral Femoral Cutaneous Nerve
-
Obturator Nerve
-
Sciatic Nerve
-
Tibial Nerve
-
Common Fibular Nerve
-
The following symptoms are caused by cutaneous nerve damage
-
Pain (dull, ache, sharp, bright)
-
Numbness, tingling, prickling, and loss of sensation
-
The following symptoms are caused by motor nerve damage
-
Weakness, paresis, and paralysis of innevated muscles
-
Atrophy, flacidity dependong on the length and severity
-
Key clinical findings for common nerve distributions include
-
Cranial Nerve 5
-
Cranial Nerve 7
-
Brachial Plexus
-
Median Nerve
-
Radial Nerve
-
Lateral Femoral Cutaneous Nerve
-
Obturator Nerve
-
Sciatic Nerve
-
Tibial Nerve
-
Common Fibular Nerve
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.