Podcast
Questions and Answers
Which of the following findings during a hip examination would most strongly suggest the need to differentiate hip pathology from a lumbar spine issue?
Which of the following findings during a hip examination would most strongly suggest the need to differentiate hip pathology from a lumbar spine issue?
- Limited and painful range of motion (ROM) of the hip joint, particularly internal rotation. (correct)
- Tenderness upon palpation of the lumbar spinous processes.
- Muscle spasms in the paraspinal muscles.
- Pain radiating down the leg following a dermatomal pattern.
A patient presents with lower back pain, recent unexplained weight loss, and a history of a previous cancer diagnosis. What is the MOST appropriate next step in managing this patient?
A patient presents with lower back pain, recent unexplained weight loss, and a history of a previous cancer diagnosis. What is the MOST appropriate next step in managing this patient?
- Order an MRI of the lumbar spine to assess for disc herniation.
- Recommend ergonomic modifications to the patient's workstation.
- Initiate a course of NSAIDs and physical therapy.
- Order blood tests and consider imaging to rule out underlying systemic conditions or metastasis. (correct)
A patient experiencing persistent lower back pain despite several weeks of conservative management, including physical therapy and analgesics. There are no neurological deficits. Which of the following would be the MOST appropriate next step?
A patient experiencing persistent lower back pain despite several weeks of conservative management, including physical therapy and analgesics. There are no neurological deficits. Which of the following would be the MOST appropriate next step?
- Refer the patient for psychological evaluation.
- Order imaging (radiographs, CT scan, or MRI) to further evaluate structural abnormalities. (correct)
- Prescribe a stronger opioid pain medication.
- Recommend surgical intervention.
Which of the following is LEAST likely to be included as part of conservative management for lower back pain?
Which of the following is LEAST likely to be included as part of conservative management for lower back pain?
A patient's lower back pain is significantly influenced by prolonged sitting at work and poor posture. Besides ergonomic adjustments, which of the following strategies would be MOST beneficial as part of a comprehensive management plan?
A patient's lower back pain is significantly influenced by prolonged sitting at work and poor posture. Besides ergonomic adjustments, which of the following strategies would be MOST beneficial as part of a comprehensive management plan?
A patient presents with lower back pain. Which aspect of their history is MOST crucial in determining the potential cause of their pain?
A patient presents with lower back pain. Which aspect of their history is MOST crucial in determining the potential cause of their pain?
During a physical examination of a patient with lower back pain, which element would be MOST helpful in identifying nerve root compression?
During a physical examination of a patient with lower back pain, which element would be MOST helpful in identifying nerve root compression?
A patient undergoing the Straight Leg Raise (SLR) test reports pain radiating down their leg. What does this finding MOST likely indicate?
A patient undergoing the Straight Leg Raise (SLR) test reports pain radiating down their leg. What does this finding MOST likely indicate?
When performing the Slump Test on a patient, at which point should you observe for radicular symptoms?
When performing the Slump Test on a patient, at which point should you observe for radicular symptoms?
What is the PRIMARY purpose of assessing a patient's spinal range of motion (ROM) during a physical examination for lower back pain?
What is the PRIMARY purpose of assessing a patient's spinal range of motion (ROM) during a physical examination for lower back pain?
Which aspect of social history is MOST relevant when evaluating a patient with lower back pain?
Which aspect of social history is MOST relevant when evaluating a patient with lower back pain?
When palpating the lumbar spine, sacrum, and pelvis of a patient with lower back pain, what is the examiner primarily assessing for?
When palpating the lumbar spine, sacrum, and pelvis of a patient with lower back pain, what is the examiner primarily assessing for?
Which of the following is the MOST important reason to include functional assessments in the evaluation of a patient with lower back pain?
Which of the following is the MOST important reason to include functional assessments in the evaluation of a patient with lower back pain?
Flashcards
Hip Examination
Hip Examination
Assessing the hip joint's range of motion, stability, and integrity.
Red Flags in Diagnostics
Red Flags in Diagnostics
Symptoms indicating serious conditions needing urgent attention.
Differential Diagnosis
Differential Diagnosis
Considering various potential causes of a patient's pain.
Conservative Management
Conservative Management
Signup and view all the flashcards
Multidisciplinary Approach
Multidisciplinary Approach
Signup and view all the flashcards
History of presenting complaint
History of presenting complaint
Signup and view all the flashcards
Aggravating and relieving factors
Aggravating and relieving factors
Signup and view all the flashcards
Associated symptoms
Associated symptoms
Signup and view all the flashcards
Functional limitations
Functional limitations
Signup and view all the flashcards
Inspection in physical exam
Inspection in physical exam
Signup and view all the flashcards
Straight Leg Raise (SLR) test
Straight Leg Raise (SLR) test
Signup and view all the flashcards
Slump Test
Slump Test
Signup and view all the flashcards
Neurological examination
Neurological examination
Signup and view all the flashcards
Study Notes
History and Symptoms
- A thorough history of the presenting complaint is essential. This includes the onset, duration, location, and radiation of pain.
- Note any aggravating or relieving factors, such as posture, movement, or activity.
- Document associated symptoms: numbness, tingling, weakness, bowel or bladder dysfunction, fever, or trauma.
- Determine if the pain is chronic or acute, and note any relevant past medical history.
- Assess functional limitations, such as difficulty with daily activities like walking, dressing, or lifting.
- A detailed social history, including occupational factors and lifestyle habits (e.g., smoking, alcohol), is vital.
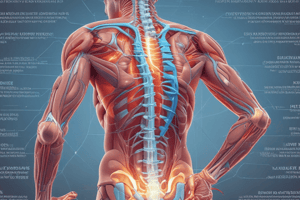
Physical Examination
- Inspection: Visual assessment of posture, gait, and visible deformities (e.g., scoliosis).
- Palpation: Systematic palpation of the lumbar spine, sacrum, and pelvis, noting tenderness, muscle spasm, or bony abnormalities. Carefully palpate specific areas of concern.
- Range of Motion: Full assessment of spinal range of motion (ROM), including flexion, extension, lateral flexion, and rotation for both the lumbar spine and hips. Observe for pain during each movement.
- Neurological Examination: Crucial for identifying potential nerve root compression. Assess muscle strength, reflexes, sensation (light touch, pinprick, vibration), and dermatomal distribution.
- Straight Leg Raise (SLR): Used to evaluate nerve root irritation. Patient lies supine while the examiner elevates the affected leg. Observe for pain radiating into the buttock or leg. Note the elevation degree at which pain occurs; this differentiates from hamstring impingement pain.
- Slump Test: Assesses nerve root impingement. Patient sits while flexing the neck and maintaining flexion, and observes for worsening radicular symptoms with passive stretching of the knee and ankle.
- Slump Test Variations: These tests evaluate the effect of different positions and stretches on nerve root symptoms.
- Functional Assessments: Assess the patient's ability to perform specific functional tasks (e.g., rising from a chair, climbing stairs). Note any difficulties or pain.
- Special tests (if indicated): Include tests for specific conditions (e.g., Patrick's test for hip pathologies, femoral nerve stretch test).
- Hip Examination: Assess the hip joint's ROM, stability, and integrity to differentiate hip from lumbar spine pathology.
Diagnostic Considerations
- Red Flags: Symptoms suggesting serious underlying conditions (e.g., cancer, infection, fracture) require immediate attention. Look for signs of systemic illness, unexplained weight loss, recent trauma, history of infection or cancer, and significant bowel/bladder disturbances.
- Differential Diagnosis: Consider various possible causes of pain, from muscle strains and ligament sprains to herniated discs, spinal stenosis, osteoarthritis, facet syndrome, and spondylolisthesis.
- Imaging: Radiographs, CT scans, or MRIs might be indicated to assess for structural abnormalities. The decision to order imaging is based on physical exam findings, patient history, and suspicion for underlying conditions.
- Further Investigations: Blood tests might be needed to rule out systemic conditions.
Management Strategies
- Conservative Management: Often the initial approach, including pain management (analgesics, NSAIDs), activity modification, physical therapy, and manual therapy.
- Surgical Intervention: Reserved for cases that fail conservative management, indicated by severe, persistent pain, progressive neurological deficits, or significant functional impairment.
- Posture and/or Ergonomics Modifications: Identify risk factors to prevent future episodes, such as prolonged sitting, poor posture, or improper lifting techniques.
- Patient Education: Crucial to educate patients about their condition, self-management strategies, and contributing factors.
- Multidisciplinary Approach: In cases of complicated pain, involve other professionals (e.g., physiatrists, psychologists, nutritionists) for a comprehensive management approach.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.