Podcast
Questions and Answers
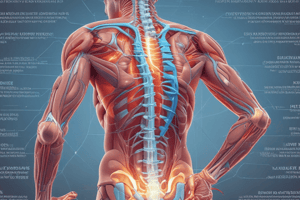
What is the primary definition of nonspecific low back pain (NSLBP)?
What is the primary definition of nonspecific low back pain (NSLBP)?
- Low back pain caused by a specific injury or trauma
- Low back pain with an identifiable cause, such as a herniated disc or spinal stenosis
- Low back pain without a known specific pathology or anatomical cause (correct)
- Low back pain that is chronic and persistent, lasting for more than 3 months
What do 'yellow flags' specifically refer to in relation to NSLBP?
What do 'yellow flags' specifically refer to in relation to NSLBP?
- Risk factors for developing a herniated disc or spinal stenosis
- Physical symptoms that indicate a serious underlying condition
- Psychological factors that may increase the risk of developing chronic pain (correct)
- Indicators for the need for diagnostic imaging tests
What is the best way to determine whether or not an individual will experience an episode of NSLBP?
What is the best way to determine whether or not an individual will experience an episode of NSLBP?
- Order diagnostic imaging tests, such as MRI or CT scan
- Perform a comprehensive physical examination
- There is no reliable way to predict who will experience NSLBP (correct)
- Assess the individual's risk factors and medical history
Which of the following is NOT a common intervention strategy utilized to provide therapy for clients with NSLBP?
Which of the following is NOT a common intervention strategy utilized to provide therapy for clients with NSLBP?
Which intervention strategy has been shown to produce the greatest therapeutic benefit for clients with NSLBP?
Which intervention strategy has been shown to produce the greatest therapeutic benefit for clients with NSLBP?
What is the value of using diagnostic imaging techniques, such as MRI, radiographic films, and CT scan?
What is the value of using diagnostic imaging techniques, such as MRI, radiographic films, and CT scan?
What is the difference between a primary and a secondary prevention strategy?
What is the difference between a primary and a secondary prevention strategy?
What is the hypothesized value of informing a client that pain improvements may require a considerable amount of time to take effect (potentially up to 4-6 weeks)?
What is the hypothesized value of informing a client that pain improvements may require a considerable amount of time to take effect (potentially up to 4-6 weeks)?
What are the therapeutic benefits of unloaded exercise in patients with NSLBP?
What are the therapeutic benefits of unloaded exercise in patients with NSLBP?
What is the MAIN factor that influences bone remodeling?
What is the MAIN factor that influences bone remodeling?
What is the primary purpose of the continuous process of bone resorption and bone formation?
What is the primary purpose of the continuous process of bone resorption and bone formation?
Which of the following is NOT a sign or symptom of osteoporosis?
Which of the following is NOT a sign or symptom of osteoporosis?
What is the BEST way to measure bone mineral density?
What is the BEST way to measure bone mineral density?
Which of the following is a NON-modifiable risk factor for osteoporosis?
Which of the following is a NON-modifiable risk factor for osteoporosis?
What type of exercise program is RECOMMENDED for individuals with osteoporosis or osteopenia?
What type of exercise program is RECOMMENDED for individuals with osteoporosis or osteopenia?
What is the MAIN benefit of prolonged cardiorespiratory training for individuals with osteoporosis or osteopenia?
What is the MAIN benefit of prolonged cardiorespiratory training for individuals with osteoporosis or osteopenia?
Which of the following is NOT a recommended approach when designing an exercise program for an individual with osteoporosis or osteopenia?
Which of the following is NOT a recommended approach when designing an exercise program for an individual with osteoporosis or osteopenia?
Which factor is crucial in the development of osteoporosis, according to the text?
Which factor is crucial in the development of osteoporosis, according to the text?
At what T-score does bone mineral density (BMD) indicate osteoporosis?
At what T-score does bone mineral density (BMD) indicate osteoporosis?
What comparison does the Z score make for bone density?
What comparison does the Z score make for bone density?
Which condition is NOT listed as a risk factor for osteoporosis in the text?
Which condition is NOT listed as a risk factor for osteoporosis in the text?
Approximately when is peak bone mass typically attained in life?
Approximately when is peak bone mass typically attained in life?
What does Osteopenia represent in terms of bone mass levels?
What does Osteopenia represent in terms of bone mass levels?