Podcast
Questions and Answers
What is the function of bile formed by hepatocytes?
What is the function of bile formed by hepatocytes?
- To filter toxins from blood
- To store glucose
- To facilitate fat digestion (correct)
- To aid in protein synthesis
Which structure is described as a small duct that forms from canaliculi and joins to form part of the bile drainage system?
Which structure is described as a small duct that forms from canaliculi and joins to form part of the bile drainage system?
- Ductule (correct)
- Gall bladder
- Central vein
- Hepatic duct
In the context of liver micro-anatomy, what does the acinus refer to?
In the context of liver micro-anatomy, what does the acinus refer to?
- A structural unit of the gall bladder
- Hepatocytes and sinusoids from two adjacent lobules supplied by one portal tract (correct)
- The central vein of the liver
- The outer layer of liver tissue
Which zone of the acinus is most severely affected by ischaemic or toxic injury?
Which zone of the acinus is most severely affected by ischaemic or toxic injury?
What primarily causes chronic passive venous congestion of the liver?
What primarily causes chronic passive venous congestion of the liver?
What are the primary blood supplies to the liver?
What are the primary blood supplies to the liver?
Which of the following is NOT a common cause of liver damage?
Which of the following is NOT a common cause of liver damage?
What distinguishes compensated cirrhosis from decompensated cirrhosis?
What distinguishes compensated cirrhosis from decompensated cirrhosis?
Which cell type in the liver helps in the regeneration process?
Which cell type in the liver helps in the regeneration process?
Portal hypertension can develop due to which of the following conditions?
Portal hypertension can develop due to which of the following conditions?
What is the typical weight of a healthy adult liver?
What is the typical weight of a healthy adult liver?
The Space of Disse in the liver is located between which structures?
The Space of Disse in the liver is located between which structures?
Which condition is commonly associated with non-alcoholic fatty liver disease?
Which condition is commonly associated with non-alcoholic fatty liver disease?
What is the most common appearance of chronic passive venous congestion of the liver?
What is the most common appearance of chronic passive venous congestion of the liver?
Which condition is indicated by obstruction to venous outflow from the liver?
Which condition is indicated by obstruction to venous outflow from the liver?
Which factor does NOT increase susceptibility to ischaemic injury to the liver?
Which factor does NOT increase susceptibility to ischaemic injury to the liver?
What is the potential outcome of extensive liver damage?
What is the potential outcome of extensive liver damage?
Which type of liver injury results in massive hepatic necrosis?
Which type of liver injury results in massive hepatic necrosis?
What is primarily synthesized by the liver?
What is primarily synthesized by the liver?
Which statement about ischaemic hepatitis is true?
Which statement about ischaemic hepatitis is true?
What defines chronic liver disease?
What defines chronic liver disease?
What is the term used for interface inflammation that indicates 'piecemeal necrosis'?
What is the term used for interface inflammation that indicates 'piecemeal necrosis'?
Which of the following best describes the stage of fibrosis when fibrous bands surround regenerative nodules and the architecture is diffusely distorted?
Which of the following best describes the stage of fibrosis when fibrous bands surround regenerative nodules and the architecture is diffusely distorted?
What is a key structural change in the liver due to cirrhosis?
What is a key structural change in the liver due to cirrhosis?
Which factor most directly contributes to the development of portal hypertension in cirrhosis?
Which factor most directly contributes to the development of portal hypertension in cirrhosis?
What is the histological feature observed in cirrhosis when using a trichrome stain?
What is the histological feature observed in cirrhosis when using a trichrome stain?
In cirrhosis, what compensatory mechanism occurs due to splanchnic vasodilation?
In cirrhosis, what compensatory mechanism occurs due to splanchnic vasodilation?
Which pattern of fibrosis is characterized by connections between portal tracts and central veins?
Which pattern of fibrosis is characterized by connections between portal tracts and central veins?
What effect does vascular alterations due to cirrhosis have on liver function?
What effect does vascular alterations due to cirrhosis have on liver function?
What happens to the blood flow in the portal system when there is increased blood flow to the intestines?
What happens to the blood flow in the portal system when there is increased blood flow to the intestines?
What contributes to the development of ascites in portal hypertension?
What contributes to the development of ascites in portal hypertension?
What is a potential risk associated with the development of shunts in portal hypertension?
What is a potential risk associated with the development of shunts in portal hypertension?
Which of the following is NOT a characteristic of decompensated cirrhosis?
Which of the following is NOT a characteristic of decompensated cirrhosis?
What triggers might lead to the decompensation of compensated cirrhosis?
What triggers might lead to the decompensation of compensated cirrhosis?
In which condition is there a block to blood flow due to liver damage?
In which condition is there a block to blood flow due to liver damage?
What is one effect of sodium and water retention in patients with portal hypertension?
What is one effect of sodium and water retention in patients with portal hypertension?
Which mechanism is involved in the body’s compensation during widespread vasodilation in portal hypertension?
Which mechanism is involved in the body’s compensation during widespread vasodilation in portal hypertension?
Which of the following best describes the concept of cirrhosis?
Which of the following best describes the concept of cirrhosis?
Which statement accurately differentiates between compensated and decompensated cirrhosis?
Which statement accurately differentiates between compensated and decompensated cirrhosis?
Which of the following is least likely to contribute to the development of portal hypertension?
Which of the following is least likely to contribute to the development of portal hypertension?
What role do hepatic stellate cells play in the liver’s response to injury?
What role do hepatic stellate cells play in the liver’s response to injury?
What is the significance of the Space of Disse in liver structure?
What is the significance of the Space of Disse in liver structure?
Which pattern of liver damage is most commonly associated with chronic alcohol consumption?
Which pattern of liver damage is most commonly associated with chronic alcohol consumption?
Which of the following processes directly contributes to ascites formation in liver disease?
Which of the following processes directly contributes to ascites formation in liver disease?
Which condition is primarily characterized by retained bile salts causing liver injury?
Which condition is primarily characterized by retained bile salts causing liver injury?
Which condition is characterized by elevation of liver blood tests due to ischaemic injury?
Which condition is characterized by elevation of liver blood tests due to ischaemic injury?
What is a common gross appearance of chronic passive venous congestion of the liver?
What is a common gross appearance of chronic passive venous congestion of the liver?
Which of the following is not a trigger for liver cell injury?
Which of the following is not a trigger for liver cell injury?
What can result from ongoing insult to the liver over an extended period?
What can result from ongoing insult to the liver over an extended period?
What defines the grade of liver damage during assessment?
What defines the grade of liver damage during assessment?
How does the liver typically respond to acute damage?
How does the liver typically respond to acute damage?
Which liver function includes the excretion of bilirubin?
Which liver function includes the excretion of bilirubin?
What is a potential consequence of massive hepatic necrosis?
What is a potential consequence of massive hepatic necrosis?
What is the 1 year mortality rate for patients with compensated cirrhosis who also have varices?
What is the 1 year mortality rate for patients with compensated cirrhosis who also have varices?
What is the median survival time for patients diagnosed with decompensated cirrhosis?
What is the median survival time for patients diagnosed with decompensated cirrhosis?
Which complication is least likely to develop in patients with compensated cirrhosis?
Which complication is least likely to develop in patients with compensated cirrhosis?
How does the development of complications in chronic liver disease affect patient prognosis?
How does the development of complications in chronic liver disease affect patient prognosis?
Which of the following is not typically associated with decompensation in chronic liver disease?
Which of the following is not typically associated with decompensation in chronic liver disease?
Which statement best characterizes the outcomes of hepatic decompensation in cirrhosis?
Which statement best characterizes the outcomes of hepatic decompensation in cirrhosis?
Which of the following features greatly increases the risk of mortality in decompensated liver disease?
Which of the following features greatly increases the risk of mortality in decompensated liver disease?
What is a major consequence of developing decompensated cirrhosis?
What is a major consequence of developing decompensated cirrhosis?
What effect does portal hypertension have on the peritoneal cavity?
What effect does portal hypertension have on the peritoneal cavity?
Which compensatory mechanism is activated due to widespread vasodilation in portal hypertension?
Which compensatory mechanism is activated due to widespread vasodilation in portal hypertension?
What complication may arise due to intrahepatic porto-systemic shunts resulting from portal hypertension?
What complication may arise due to intrahepatic porto-systemic shunts resulting from portal hypertension?
What triggers the decompensation of compensated cirrhosis?
What triggers the decompensation of compensated cirrhosis?
What is a common outcome of sodium and water retention in individuals with portal hypertension?
What is a common outcome of sodium and water retention in individuals with portal hypertension?
What describes the vascular changes in the liver due to cirrhosis?
What describes the vascular changes in the liver due to cirrhosis?
What underlying issue contributes to the higher mean hydrostatic pressure seen in portal hypertension?
What underlying issue contributes to the higher mean hydrostatic pressure seen in portal hypertension?
Which characteristic is indicative of bridging fibrosis?
Which characteristic is indicative of bridging fibrosis?
What is a main consequence of portal hypertension in cirrhosis?
What is a main consequence of portal hypertension in cirrhosis?
What is primarily affected due to cirrhosis in the context of blood flow dynamics?
What is primarily affected due to cirrhosis in the context of blood flow dynamics?
What consequence may result from the capillarisation of sinusoids in the context of portal hypertension?
What consequence may result from the capillarisation of sinusoids in the context of portal hypertension?
Which feature is observed in cirrhosis when using H&E staining?
Which feature is observed in cirrhosis when using H&E staining?
How does splanchnic vasodilation affect the cardiovascular system in cirrhosis?
How does splanchnic vasodilation affect the cardiovascular system in cirrhosis?
What does the presence of regenerative nodules and fibrous septa indicate in liver histology?
What does the presence of regenerative nodules and fibrous septa indicate in liver histology?
What is the role of the hepatic venous pressure gradient (HVPG) in portal hypertension?
What is the role of the hepatic venous pressure gradient (HVPG) in portal hypertension?
Which histological feature helps to identify the degree of fibrosis in liver biopsy?
Which histological feature helps to identify the degree of fibrosis in liver biopsy?
Flashcards are hidden until you start studying
Study Notes
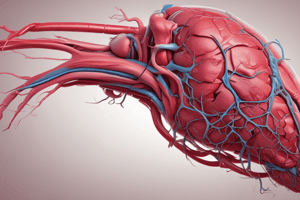
Liver Structure and Blood Supply
- Liver weighs approximately 1.5kg and possesses a significant functional reserve
- Liver cells are capable of regeneration
- Liver has a dual blood supply with both the hepatic artery and portal vein delivering blood
- Blood flows through sinusoids, which are blood spaces separating plates of hepatocytes
- Sinusoids are lined by fenestrated endothelium and Kupffer cells (macrophages)
- The Space of Disse lies between sinusoids and hepatocytes and contains hepatic stellate cells
- Venous drainage occurs via the hepatic vein to the inferior vena cava (IVC) to the right ventricle (RV)
Liver Function
- Liver synthesizes most plasma proteins, including those involved in clotting
- Liver produces bile for excretion of bilirubin and digestion of fats and fat-soluble vitamins (ADEK)
- Liver detoxifies both endogenous and exogenous compounds
- Liver plays a role in intermediary metabolism, altering and storing substances
- Liver participates in immune functions, acting as a buffer between the gut and the rest of the body
- Liver stores both normal and abnormal substances
- Liver performs hematopoiesis (blood cell production) in the fetus and infant
Liver Injury
- Liver has a reserve and regenerative capacity, allowing for recovery from acute damage in many cases
- Extensive acute damage can lead to acute liver failure
- Chronic liver damage occurs with ongoing insult and is defined as damage lasting over six months
- Chronic damage can lead to fibrosis and progression to cirrhosis
- Co-existing causes of liver damage can exacerbate the condition
- Patterns of cell damage can vary from single-cell death (apoptosis) to massive hepatic necrosis
- Cell injury can be triggered by direct cytotoxic effects, damage to hepatocytes rendering them antigenic (e.g., HBV), or damage to cells perceived as antigenic (e.g., autoimmune hepatitis)
Assessment of Liver Damage
- Inflammation and necrosis are graded based on extent of damage
- Inflammation can occur in the portal/periportal area or in the lobules (parenchyma)
- Piecemeal necrosis describes a specific pattern of interface inflammation
- Necrosis can be present as single-cell death, spotty necrosis, or bridging necrosis
- Predominant inflammatory cell type is influenced by the cause of liver damage
- Fibrosis is staged based on degree and extent
- Fibrosis can occur in portal areas, periportal areas, and as bridging fibrosis (portal tract to portal tract or portal tract to central vein)
- Cirrhosis represents the end-stage of fibrosis
- Complex scoring systems are used to assess liver biopsy specimens, considering both grade and stage
Cirrhosis
- Cirrhosis is characterized by diffuse distortion of liver architecture, with fibrous bands, regenerative nodules, and distorted vascular relationships
- Cirrhosis impairs liver function, contributing to portal hypertension and increasing the risk of hepatocellular carcinoma
- Vascular changes in cirrhosis include obliteration or thrombosis of veins, formation of collateral channels, and capillarization of sinusoids, leading to an increased hepatic venous pressure gradient (HVPG)
- Cirrhosis represents the end-stage of chronic liver disease, diminishing liver reserve
Portal Hypertension
- Increased resistance to portal blood flow in cirrhosis initiates portal hypertension, raising HVPG
- Splanchnic vasodilatation (via nitric oxide, NO) further contributes to portal hypertension
- Splanchnic vasodilatation reduces total peripheral resistance (TPR) and blood pressure
- The body compensates with increased cardiac output, leading to a hyperdynamic circulation in cirrhosis
- Splanchnic vasodilatation triggers compensatory mechanisms, including activation of the renin-angiotensin-aldosterone system, ADH secretion, sodium and water retention, and renal vasoconstriction
Ascites
- Sodium and water retention in the setting of portal hypertension can lead to ascites
- Ascites occurs due to fluid leakage from peritoneal vessels, increased hydrostatic pressure, and decreased oncotic pressure (low albumin)
Portal Hypertension Shunts
- To decompress portal hypertension, collateral channels form both within and outside the liver
- Therapeutic shunts, such as transjugular intrahepatic porto-systemic shunts (TIPS), can be inserted
- Shunting bypasses the liver, further reducing liver function and exacerbating damage
Compensated vs. Decompensated Cirrhosis
- Compensated cirrhosis may not manifest with biochemical or radiological abnormalities or signs of chronic liver disease or portal hypertension
- Even with compensated cirrhosis, further injury (infection, bleeding, hypotension, alcohol, medications, dehydration, trauma, surgery) can trigger decompensation
- Decompensated cirrhosis is characterized by complications including ascites, hepatic encephalopathy, variceal hemorrhage, hepatorenal syndrome (HRS), jaundice, and infections
Liver Structure & Function
- The liver weighs about 1.5kg
- It has a large functional reserve
- The liver contains stable cells and is able to regenerate
- The liver's blood supply is dual: hepatic artery and portal vein
- Blood travels through sinusoids, which are blood spaces separating plates of hepatocytes
- Sinusoids are lined by fenestrated endothelium and macrophages (Kupffer cells)
- Space of Disse sits between sinusoids and hepatocytes and contains hepatic stellate cells
- Venous drainage is via the hepatic vein to the inferior vena cava (IVC) to the right ventricle (RV)
- Main functions include:
- Synthesis of most plasma proteins
- Clotting factors
- Bile formation
- Bilirubin: excretion
- Bile Salts -- digestion
- Fat/fat-soluble vitamins ADEK
- Detoxification of endogenous/exogenous compounds
- Intermediary metabolism
- Immune function as a buffer between the gut and rest of the body
- Storage - normal/abnormal
- Haematopoiesis (foetal/infant)
Liver Damage
- The liver has reserve and regenerative capacity
- Possible outcomes of acute liver damage depend on the degree of damage
- Extensive damage may result in acute liver failure
- Transient damage may lead to recovery
- On-going or repeated insult leads to chronic damage
- Chronic liver disease is defined as damage lasting longer than 6 months
- Fibrosis develops and progresses to cirrhosis
- The causes of liver damage may coexist, be superimposed, or potentiate each other
- Patterns of cell damage and death include different types of cell injury (reversible or irreversible)
- Triggers for injury include:
- Direct cytopathic/cytotoxic/ischaemic effects
- Damage to hepatocytes rendered antigenic (e.g. HBV)
- Damage to cells perceived as antigenic (e.g. autoimmune hepatitis)
- Different degrees of injury include:
- Single cell death (apoptosis)
- Small group cell death (spotty necrosis)
- Large confluent group cell death (bridging necrosis)
- Massive hepatic necrosis
Assessing Liver Damage
- Inflammation and/or necrosis is assessed by its extent, termed "grade"
- 炎症是否属于门脉周围、门脉或小叶性?有多少门脉周围、门脉或小叶性炎症?界面炎症= “片状坏死”
- Is necrosis present? Single cells, spotty or bridging?
- Predominant inflammatory cell type depends on aetiology, not whether the disease is acute or chronic in duration.
- Fibrosis is assessed by its degree and extent, termed "stage"
- Portal fibrosis
- Periportal fibrosis
- Bridging fibrosis: portal to portal tract or portal to central vein
- Cirrhosis
- Liver biopsy is used for complex scoring systems to assess grade and stage independently
Cirrhosis
- A diffuse distortion of liver architecture
- Fibrous bands/septa surround regenerative nodules
- Distorted vascular relationships lead to:
- Decreased liver function
- Portal hypertension
- Risk of hepatocellular carcinoma
Portal Hypertension
- Results from increased hepatic resistance to portal blood flow, and a rise in HVPG (hepatic venous pressure gradient)
- Augmented by splanchnic vasodilatation, which increases portal blood flow
- Splanchnic vasodilatation also lowers total peripheral resistance (TPR) and blood pressure (BP)
- A compensatory increase in cardiac output leads to the hyperdynamic circulation of cirrhosis
- Splanchnic vasodilatation triggers compensatory mechanisms
- Activation of the renin-angiotensin-aldosterone system
- Stimulation of antidiuretic hormone (ADH) secretion
- Sodium and water retention
- Reflex renal vasoconstriction = reduced perfusion and glomerular filtration rate (GFR), increasing the risk of hepatorenal syndrome (HRS)
Ascites
- Sodium and water retention, related to portal hypertension, preferentially accumulates fluid in the peritoneal cavity.
- Fluid leaks from peritoneal vessels
- Higher mean hydrostatic pressure due to portal hypertension
- Lower oncotic pressure to keep fluid in due to low albumin
Portal Hypertension & Shunts
- Collaterals develop to decompress portal hypertension:
- Intrahepatic porto-systemic shunts/collaterals
- Extrahepatic porto-systemic anastomoses dilate
- Therapeutic insertion of a shunt (TIPS -- transjugular intrahepatic porto-systemic shunt)
- "Shunted" blood bypasses the liver, further reducing liver function and increasing the risk of hepatic encephalopathy
- "Capillarisation" of sinusoids exacerbates this process
- Shunting reduces perfusion of the liver, worsening the damage
Compensated vs. Decompensated Cirrhosis
- Compensated (Silent) Cirrhosis
- May or may not have biochemical/radiological abnormality
- May or may not have signs of chronic liver disease/portal hypertension
- May or may not have varices on OGD (gastroscopy)
- Potential for instability, with further injury triggering decompensation (infection, bleeding, hypotension, alcohol, medications, dehydration, trauma, surgery)
- Decompensated Cirrhosis
- Key complications:
- Ascites (may become refractory to treatment)
- Hepatic encephalopathy
- Variceal hemorrhage
- Hepatorenal syndrome (HRS)
- Jaundice
- Infection (esp. spontaneous bacterial peritonitis)
- Hepatocellular carcinoma
- Key complications:
- Decompensation significantly affects prognosis
- 1-year mortality:
- Compensated - 1%
- Compensated with varices - 4%
- Decompensated, ascites - 20%
- Decompensated, other features - >50%
- 1-year mortality:
Natural History of Chronic Liver Disease
- Decompensation affects prognosis
- Progression from chronic liver disease to compensated cirrhosis to decompensated cirrhosis can lead to death.
- Median compensated cirrhosis survival is approximately 9 years.
- Median decompensated cirrhosis survival is approximately 1.6 years.
- Variceal hemorrhage, ascites, encephalopathy, and jaundice are all common complications.
- Orthotopic liver transplant (OLT) may be a treatment option.
- Survival times in cirrhosis are significantly impacted by decompensation.
- The median survival for patients with cirrhosis overall is 9 years.
- For patients with decompensated cirrhosis, the median survival is 1.6 years.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.