Podcast
Questions and Answers
Which process is compromised in liver cirrhosis, leading to a buildup of toxic substances in the bloodstream?
Which process is compromised in liver cirrhosis, leading to a buildup of toxic substances in the bloodstream?
- Bile production and excretion
- Albumin synthesis
- Detoxification by hepatocytes (correct)
- Clotting factor production
What causes the yellowish stool often observed in individuals with liver cirrhosis?
What causes the yellowish stool often observed in individuals with liver cirrhosis?
- Accumulation of albumin in the intestines
- Increased production of bile salts
- Decreased excretion of bilirubin (correct)
- Increased iron absorption in the intestines
What is the primary mechanism by which the cirrhotic liver contributes to ascites?
What is the primary mechanism by which the cirrhotic liver contributes to ascites?
- Reduced production of albumin (correct)
- Enhanced detoxification of ammonia
- Increased synthesis of clotting factors
- Increased metabolism of estrogen
Which diagnostic finding is most indicative of impaired liver function related to clotting factor production?
Which diagnostic finding is most indicative of impaired liver function related to clotting factor production?
What is the rationale behind administering lactulose to a patient with hepatic encephalopathy?
What is the rationale behind administering lactulose to a patient with hepatic encephalopathy?
Why are beta-blockers prescribed for patients with portal hypertension secondary to cirrhosis?
Why are beta-blockers prescribed for patients with portal hypertension secondary to cirrhosis?
A patient with cirrhosis develops sudden pain and bluish discoloration around the umbilicus. What condition should be suspected?
A patient with cirrhosis develops sudden pain and bluish discoloration around the umbilicus. What condition should be suspected?
What is the physiological basis for 'asterixis' observed in patients with hepatic encephalopathy?
What is the physiological basis for 'asterixis' observed in patients with hepatic encephalopathy?
The hepatic portal vein carries nutrient-rich blood from which organs to the liver?
The hepatic portal vein carries nutrient-rich blood from which organs to the liver?
An individual with liver cirrhosis is likely to have alterations in the metabolism of which hormone?
An individual with liver cirrhosis is likely to have alterations in the metabolism of which hormone?
Which of these is a primary function of bile produced by the liver?
Which of these is a primary function of bile produced by the liver?
A patient presenting with right upper quadrant pain triggered by fatty food ingestion is likely experiencing which condition?
A patient presenting with right upper quadrant pain triggered by fatty food ingestion is likely experiencing which condition?
What is the underlying mechanism for referred shoulder pain in a patient with acute cholecystitis (Boas sign)?
What is the underlying mechanism for referred shoulder pain in a patient with acute cholecystitis (Boas sign)?
What is the significance of clay-colored stools in patients with cholecystitis?
What is the significance of clay-colored stools in patients with cholecystitis?
What vitamin deficiencies are commonly associated with cholecystitis due to bile obstruction?
What vitamin deficiencies are commonly associated with cholecystitis due to bile obstruction?
Chenodeoxycholic acid (chenodiol) is used in the management of cholecystitis primarily to achieve what outcome?
Chenodeoxycholic acid (chenodiol) is used in the management of cholecystitis primarily to achieve what outcome?
Why might a patient experience shoulder pain following a laparoscopic cholecystectomy?
Why might a patient experience shoulder pain following a laparoscopic cholecystectomy?
What is the function of the pancreatic acinar cells?
What is the function of the pancreatic acinar cells?
In pancreatitis, which process contributes most directly to the autodigestion of the pancreatic tissue?
In pancreatitis, which process contributes most directly to the autodigestion of the pancreatic tissue?
How does alcohol consumption contribute to the pathophysiology of pancreatitis?
How does alcohol consumption contribute to the pathophysiology of pancreatitis?
What is the rationale for making patients with acute pancreatitis NPO (nothing by mouth)?
What is the rationale for making patients with acute pancreatitis NPO (nothing by mouth)?
What causes Cullen's sign (bluish discoloration around the umbilicus) in patients with severe pancreatitis?
What causes Cullen's sign (bluish discoloration around the umbilicus) in patients with severe pancreatitis?
In patients with pancreatitis, what is the effect of pancreatic damage on blood glucose levels?
In patients with pancreatitis, what is the effect of pancreatic damage on blood glucose levels?
Why should pancrelipase not be mixed with alkaline liquids?
Why should pancrelipase not be mixed with alkaline liquids?
What is the primary initiating event in the pathophysiology of appendicitis?
What is the primary initiating event in the pathophysiology of appendicitis?
What physical assessment finding suggests appendicitis?
What physical assessment finding suggests appendicitis?
Rovsing's sign is elicited during an abdominal examination. What response indicates a positive Rovsing’s sign?
Rovsing's sign is elicited during an abdominal examination. What response indicates a positive Rovsing’s sign?
What is the primary treatment for appendicitis?
What is the primary treatment for appendicitis?
What is the significance of elevated WBC (White Blood Cell) and C-Reactive Protein (CRP) in a patient with suspected appendicitis?
What is the significance of elevated WBC (White Blood Cell) and C-Reactive Protein (CRP) in a patient with suspected appendicitis?
Flashcards
Liver Detoxification
Liver Detoxification
Cleansing of toxins from the blood, facilitated by hepatocytes.
Ammonia Conversion
Ammonia Conversion
Conversion of ammonia into urea for excretion.
Liver Cirrhosis
Liver Cirrhosis
Final stage of liver disease characterized by irreversible scarring.
Liver Vitamin Storage
Liver Vitamin Storage
Signup and view all the flashcards
Estrogen Regulation
Estrogen Regulation
Signup and view all the flashcards
Albumin Production
Albumin Production
Signup and view all the flashcards
Clotting Factors
Clotting Factors
Signup and view all the flashcards
Biles Function
Biles Function
Signup and view all the flashcards
Hepatic Artery
Hepatic Artery
Signup and view all the flashcards
Hepatic Portal Vein
Hepatic Portal Vein
Signup and view all the flashcards
Risk Factors of Cirrhosis
Risk Factors of Cirrhosis
Signup and view all the flashcards
Cirrhosis Progression
Cirrhosis Progression
Signup and view all the flashcards
Intoxication in Cirrhosis
Intoxication in Cirrhosis
Signup and view all the flashcards
Hepatic Encephalopathy
Hepatic Encephalopathy
Signup and view all the flashcards
Jaundice
Jaundice
Signup and view all the flashcards
Steatorrhea
Steatorrhea
Signup and view all the flashcards
Spider Angioma
Spider Angioma
Signup and view all the flashcards
Palmar Erythema
Palmar Erythema
Signup and view all the flashcards
Portal Hypertension
Portal Hypertension
Signup and view all the flashcards
Esophageal Varices
Esophageal Varices
Signup and view all the flashcards
Managing Intoxication
Managing Intoxication
Signup and view all the flashcards
Hepatic Encephalopathy Tx
Hepatic Encephalopathy Tx
Signup and view all the flashcards
Glucose Regulation
Glucose Regulation
Signup and view all the flashcards
Elevated Liver Enzymes
Elevated Liver Enzymes
Signup and view all the flashcards
Bile Storage
Bile Storage
Signup and view all the flashcards
Bilirubin carriage
Bilirubin carriage
Signup and view all the flashcards
Gallstones
Gallstones
Signup and view all the flashcards
Gallbladder disorder manifestation!
Gallbladder disorder manifestation!
Signup and view all the flashcards
Which diagnostics are used for gallbladder assessment?
Which diagnostics are used for gallbladder assessment?
Signup and view all the flashcards
Pancreatic juices
Pancreatic juices
Signup and view all the flashcards
Study Notes
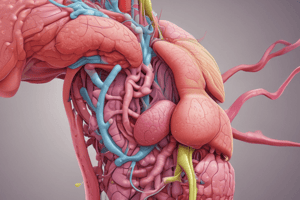
Liver Cirrhosis Physiology
- Hepatocytes detoxify the blood facilitated by sinusoid
- Ammonia, a byproduct of protein metabolism, is converted into urea for excretion
- Bile; bile salt and bilirubin (due to RBC breakdown) are excreted, causing yellowish stool
- Vitamins ADEK, B12 (cobalamin), B9 (folate), Iron, and glucose (glycogen) are stored
- Albumin is produced to maintain oncotic pressure and prevent blood vessel leakage
- Clotting factors like fibrinogen and prothrombin are produced
- Estrogen is metabolized and eliminated
- The liver facilitates blood flow through the hepatic portal vein
Liver Anatomy
- Hepatic portal vein drains blood which is rich with nutrients but low in oxygen
- Superior mesenteric vein drains the small intestine, pancreas, and large intestine
- Inferior mesenteric vein drains the large intestine and rectum
- Splenic vein drains the spleen and pancreas
- Gastric and Cystic veins drain the stomach and gallbladder
- Hepatic artery supplies oxygenated blood to the liver
Liver Cirrhosis Pathophysiology
- Liver cirrhosis is characterized by inflammation, fibrosis (liver scarring), and altered liver function
- Obesity, alcohol consumption, and Hepatitis B and C are common risk factors
Liver Cirrhosis Manifestation
- Intoxication occurs due to impaired detoxification through the sinusoid
- Hepatic encephalopathy (asterixis) and confabulation results from impaired ammonia conversion
- Jaundice, no ADEK absorption, and steatorrhea result from impaired bile production
- Malnutrition and impaired glucose regulation results from impaired vitamin and glycogen storage
- Ascites results in decreased production of albumin
- Bleeding/coagulopathy results in decreased production of clotting factors
- Spider angioma and palmar erythema results from impaired estrogen metabolism
- Portal hypertension and esophageal & gastric varices are dilated veins which may lead to bleeding due to impaired facilitation of blood through the hepatic portal vein
Liver Cirrhosis Management
- Avoid hepatotoxic drugs to prevent intoxication
- Lactulose is administered for hepatic encephalopathy (asterixis) and confabulation
- Intravenous (IV) fat emulsion is administered in the case of no ADEK absorption and steatorrhea
- Nutritional supplements are recommended for malnutrition
- Monitor for signs of hyperglycemia/hypoglycemia for glucose regulation
- Diuretics and paracentesis are administered for ascites
- Bleeding precautions, BT, IVF are applied for bleeding
- Beta-blockers are administered and straining is avoided for portal hypertension, esophageal & gastric varices
Liver Cirrhosis Diagnostics
- Increased AST (Aspartate Aminotransferase) and ALT (Alanine Aminotransferase) indicates impaired liver function
- International Normalized Ratio (INR) is elevated; normal range is 10–14 seconds
- Prothrombin Time (PT) is elevated; normal range is 0.8–1.2
- Platelet, WBCs and hemoglobin counts are decreased indicating splenic sequestration
- Albumin levels are decreased
- Ammonia levels are increased
Cholecystitis Physiology
- Bile is stored for fat digestion/emulsification
- Bilirubin, a brownish/yellow fluid (byproduct of RBC breakdown), is carried and excreted through the gastrointestinal (GI) tract (feces)
Cholecystitis Pathophysiology
- Gallstone (cholelithiasis), obesity, high fat diet and skipping meals may cause cholecystitis
- Obstruction or no contraction could lead to increased pressure in the gallbladder wall
- Inflammation of the gallbladder
- Altered gallbladder function
Cholecystitis Manifestation
- Steatorrhea, vitamin ADEK deficiency/malnutrition are symptoms of cholecystitis
- Clay-colored stool, jaundice, and dark urine are manifestations of cholecystitis
- Pain in the right upper back/shoulder (referred pain) is known as Boas sign, and occurs due to phrenic nerve irritation
- Murphy's sign is right upper quadrant (RUQ) pain upon inspiration
- Biliary colic is RUQ pain triggered by fat ingestion
Cholecystitis Management
- Chenodeoxycholic acid (chenodiol) is administered as a gallstone dissolution agent
- Laparoscopic Cholecystectomy may cause shoulder pain
- Open Cholecystectomy is a treatment option
Cholecystitis Diagnostics
- ERCP Endoscopic Retrograde Cholangiopancreatography) is used for diagnostics
- Abdominal Ultrasound is used for diagnostics
- Increased bilirubin is a diagnostic measure
Pancreatitis Physiology
- Acinar cells produce lipase, protease (trypsin and chymotrypsin), and amylase
- Insulin, a hormone or 'key', is produced in the Islet of Langerhans, and facilitates entry of blood glucose into the cell
- Glucagon, a hormone, stimulates stored glucose (glycogen) in the liver
Pancreatitis Pathophysiology
- Obstruction in pancreatic duct/common bile duct/sphincter of Oddi (gallstone, cystic fibrosis) and alcohol can cause pancreatitis
- Acinar cell damage results in premature activation of pancreatic juices
- Autodigestion is a pancreatic enzyme that leads to inflammation of the pancreas and possible hemorrhage
- Thick mucus can obstruct the pancreas
- Blocked pancreatic duct
- All of the above contribute to altered function of the pancreas
Pancreatitis Manifestation
- Postprandial pain
- Vitamin ADEK malabsorption/malnutrition, steatorrhea are manifestations of pancreatitis
- Hyperglycemia (Type 3c Diabetes/T3cD) is when blood sugar is too high
- Hypoglycemia is when blood sugar is too low
- Bleeding due to autodigestion
- Cullen's sign: bluish discoloration on the umbilicus
- Grey Turner sign: bluish discoloration on the flank area
Pancreatitis Management
- Acute condition: NPO (nothing by mouth)
- Nutritional support
- Monitor blood glucose
- Pancrelipase (should not be mixed with alkaline liquids)
- Low fat, no alcohol consumption, and limit simple carbohydrates
Pancreatitis Diagnostics
- CT scan or Ultrasound
- Elevated White Blood Cell (WBC) count
- Elevated C-Reactive Protein (CRP)
- The findings above are not only limited to pancreatitis, but are indicative
Appendicitis Pathophysiology
- Fecalith due to low fiber intake is the main cause
- Bacterial Infection
- Inflammation of the appendix, leading to rupture
Appendicitis Manifestation
- McBurney's point tenderness: RLQ pain when pressed
- Rovsing's sign: pain in RLQ when pressing the LLQ
- Psoas sign: pain in RLQ when extending the right leg
- Obturator sign: pain in RLQ when internally rotating the right hip
Appendicitis Management
- Laparoscopic Appendectomy is a treatment option
- Open Appendectomy is a treatment option
- Antibiotics
- Analgesics are prescribed for pain
- Elevated WBC and C-Reactive Protein are indicative of appendicitis
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.