Podcast
Questions and Answers
What type of nerve supply predominantly influences the spleen?
What type of nerve supply predominantly influences the spleen?
- Sympathetic nerve supply from the coeliac plexus (correct)
- Sensory fibres from the vagus nerve
- Sympathetic nerve supply from the pelvic plexus
- Parasympathetic nerve supply from the vagus nerve
Which region is the referred pain for the liver's diaphragmatic surface typically located?
Which region is the referred pain for the liver's diaphragmatic surface typically located?
- Left shoulder
- Lower back
- Epigastric region
- Right shoulder (correct)
Which nerve fibers stimulate the contraction of the gallbladder?
Which nerve fibers stimulate the contraction of the gallbladder?
- T10 spinal nerves
- Vagus nerve parasympathetic fibers (correct)
- Superior mesenteric plexus
- Celiac plexus sympathetic fibers
What is the primary role of endoscopic retrograde cholangiopancreatography (ERCP)?
What is the primary role of endoscopic retrograde cholangiopancreatography (ERCP)?
In which area is referred pain from the pancreas typically localized?
In which area is referred pain from the pancreas typically localized?
What can cause splenomegaly?
What can cause splenomegaly?
Which type of pain is associated with the fibrous capsule of the liver?
Which type of pain is associated with the fibrous capsule of the liver?
Which system is the spleen primarily a part of?
Which system is the spleen primarily a part of?
What is the primary function of the gallbladder?
What is the primary function of the gallbladder?
Which part of the gallbladder is responsible for preventing obstruction to the inflow/outflow of bile?
Which part of the gallbladder is responsible for preventing obstruction to the inflow/outflow of bile?
What is the length of the bile duct formed by the junction of the cystic and common hepatic ducts?
What is the length of the bile duct formed by the junction of the cystic and common hepatic ducts?
What type of gland is the pancreas classified as?
What type of gland is the pancreas classified as?
Where does the head of the pancreas lie?
Where does the head of the pancreas lie?
Which artery is primarily responsible for supplying the gallbladder?
Which artery is primarily responsible for supplying the gallbladder?
What major function does the spleen perform?
What major function does the spleen perform?
Which ligament is associated with the spleen and contains splenic vessels?
Which ligament is associated with the spleen and contains splenic vessels?
What is the anatomical location of the spleen?
What is the anatomical location of the spleen?
What happens at the major duodenal papilla?
What happens at the major duodenal papilla?
Which of the following statements accurately describes the functions of the liver?
Which of the following statements accurately describes the functions of the liver?
What anatomical feature serves as an attachment site for the lesser omentum?
What anatomical feature serves as an attachment site for the lesser omentum?
Which ligament divides the liver into right and left lobes?
Which ligament divides the liver into right and left lobes?
Which lobe of the liver is functionally associated with the quadrate lobe?
Which lobe of the liver is functionally associated with the quadrate lobe?
Which of the following vessels brings deoxygenated blood from the gastrointestinal tract to the liver?
Which of the following vessels brings deoxygenated blood from the gastrointestinal tract to the liver?
What is the significance of the hepatic ducts in liver anatomy?
What is the significance of the hepatic ducts in liver anatomy?
Which of the following correctly identifies the components of the right triangular ligament?
Which of the following correctly identifies the components of the right triangular ligament?
What is the primary role of the caudate lobe within the liver?
What is the primary role of the caudate lobe within the liver?
Which part of the liver is covered by visceral peritoneum except in specific areas?
Which part of the liver is covered by visceral peritoneum except in specific areas?
In which area of the liver does the common hepatic duct exit?
In which area of the liver does the common hepatic duct exit?
What anatomical relationship exists between the liver and the gallbladder?
What anatomical relationship exists between the liver and the gallbladder?
Which of the following statements is true regarding ligaments associated with the liver?
Which of the following statements is true regarding ligaments associated with the liver?
Which segment is known as Segment I in the functional lobes of the liver?
Which segment is known as Segment I in the functional lobes of the liver?
Flashcards are hidden until you start studying
Study Notes
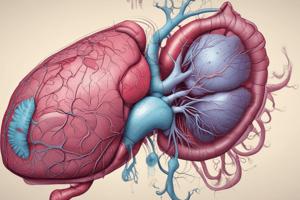
Liver
- Largest visceral organ in the body.
- Located primarily in the right hypochondrium and epigastric region, extending into the left hypochondrium.
- Has two surfaces:
- Diaphragmatic surface: Anterior, superior, and posterior.
- Visceral surface: Inferior.
- Responsible for various functions including metabolism, bile and prothrombin synthesis, excretion, glycogen storage, and protection via antibody formation.
Diaphragmatic Surface
- Smooth and domed.
- Lies against the inferior surface of the diaphragm.
- Associated with subphrenic and hepatorenal recesses:
- Subphrenic recess: Separates the liver from the diaphragm, divided into left and right areas by the falciform ligament.
- Hepatorenal recess: Part of the peritoneal cavity on the right side, between the liver and the right kidney and suprarenal gland.
- The two recesses are continuous anteriorly.
Visceral Surface
- Covered with visceral peritoneum except in the fossa for the gallbladder and at the porta hepatis.
- Related structures:
- Oesophagus.
- Right anterior part of the stomach.
- Superior part of the duodenum.
- Lesser omentum.
- Gallbladder.
- Right colic flexure.
- Right transverse colon.
- Right kidney.
- Right suprarenal gland.
Porta Hepatis
- Deep transverse fissure between the quadrate and caudate lobes.
- Point of entry for hepatic arteries and portal vein, and exit for hepatic ducts.
- Attachment site for the lesser omentum, surrounding structures of the porta hepatis.
- Hepatic ducts lie anterior to the portal vein, with hepatic arteries usually lying between the two.
Falciform Ligament
- Attaches the liver to the anterior abdominal wall.
- Divides the liver into right and left lobes on its posterior surface.
Ligaments Associated with the Liver
- Falciform Ligament: Attaches liver to anterior abdominal wall, divides liver into right and left lobes.
- Ligamentum Venosum: On posterior surface, borders caudate lobe superiorly, remnant of ductus venosus.
- Ligamentum Teres: Also known as round ligament, on posterior surface, found in interlobar notch, borders quadrate lobe inferiorly, remnant of umbilical vein.
- Hepatogastric Ligament: Connects liver to stomach.
- Hepatoduodenal Ligament: Connects liver to duodenum.
- Right and Left Triangular Ligaments: Attach liver to diaphragm.
- Anterior and Posterior Coronary Ligaments: Attach liver to diaphragm, enclose bare area of liver.
Bare Area of the Liver
- Part of the liver free from peritoneum.
- Anterior boundary: Indicated by anterior coronary ligament.
- Posterior boundary: Indicated by posterior coronary ligament.
- Coronary ligaments come together laterally to form right and left triangular ligaments.
Lobes of the Liver
- Falciform ligament divides the liver into right and left lobes.
- Right Lobe: Largest, accounts for approximately ⁵/₆ of the liver.
- Left Lobe: Flattened from above downwards, accounts for approximately ¹/₆ of the liver.
- Posteriorly, the fissure for the ligamentum venosum and ligamentum teres divide the liver into two lobes.
- Quadrate Lobe: Located between the fissure for the ligamentum teres (left) and the fossa for the gallbladder (right), functionally associated with the left lobe.
- Caudate Lobe: Located between the fissure for the ligamentum venosum (left) and the groove for the inferior vena cava (right), functionally separate from both the right and left lobes.
Vasculature of the Liver
- Hepatic artery, hepatic portal veins, hepatic veins.
- Hepatic artery and portal vein ascend in the lesser omentum to the porta hepatis.
- Common hepatic duct and lymphatic vessels descend in the lesser omentum.
- Hepatic veins leave the liver on its posterior surface to drain into the IVC.
- Lymphatic drainage: Caval, hepatic, paracardial, and coeliac nodes.
- Some lymph from coronary ligaments drain into the thoracic duct directly.
Functional Lobes of the Liver
- Liver divided into eight functional segments based on the distribution of portal venous branches in the parenchyma.
- Divided into four portal sectors: Right anterior, right posterior, left medial, left lateral.
- Division is due to four main hepatic veins, with three hepatic veins lying between segments as intersectoral veins.
- Veins lie in main fissures which divide sectors.
- Segments labelled in clockwise fashion (on anterior view) starting with Segment I, the caudate lobe.
Gallbladder
- Pear-shaped sac lying between the right and quadrate lobes of the liver.
- Measures approximately 7-10cm long, 3cm broad, with a capacity of 30-50ml.
- Receives, concentrates, and stores bile from the liver.
- Components:
- Fundus: Rounded end projecting from the inferior border of the liver, situated in the angle between the rectus abdominus and the 9th costal cartilage.
- Body: Lies against the transverse colon and superior part of the duodenum, continuous with the neck at the right end of the porta hepatis.
- Neck: Narrow part with mucosal folds which form a spiral fold preventing obstruction to bile outflow/inflow.
Cystic Duct
- 3-4cm long, originating at the neck of the gallbladder.
- Joins the common hepatic duct at an angle to form the bile duct.
- Mucous membrane forms crescenteric folds.
Bile Duct
- Formed by the union of the cystic duct and common hepatic duct.
- 8cm long, running through supraduodenal, retroduodenal, infraduodenal, and intraduodenal regions.
- Opens into the major duodenal papilla.
Neurovasculature of the Gallbladder
- Arterial Supply: Cystic artery (branch of right hepatic artery) supplies the gallbladder, and the posterior superior pancreaticoduodenal artery supplies the bile duct.
- Venous Drainage: Cystic veins, portal veins, hepatic veins.
- Lymphatics: Cystic node, hepatic node, upper pancreaticosplenic node.
- Nerve Supply: Cystic plexus of nerves, right phrenic nerves.
Pancreas
- Located posterior to the stomach, extending across the posterior abdominal wall between the duodenum and spleen, at L1.
- J-shaped, 15-20cm long.
- Retroperitoneal except for a small part of the tail.
- Structurally:
- Branched acinar gland wrapped in delicate connective tissue.
- Healthy pancreas is yellow, with a soft-to-firm consistency and a lobulated surface.
- Components:
- Head: Lies within the C-shaped concavity of the duodenum.
- Uncinate Process: Projects from the lower part of the head, lies posterior to the superior mesenteric vessels.
- Neck: Anterior to the superior mesenteric vessels, the splenic and superior mesenteric veins join to form the portal vein posterior to the neck of the pancreas.
- Body: Elongated, extends from the neck to the tail of the pancreas.
- Tail: Passes between layers of the splenorenal ligament.
Pancreatic Duct
- Begins in the tail of the pancreas, turns inferiorly at the head of the pancreas.
- Joins the bile duct in the lower part of the head forming the hepatopancreatic ampulla.
- The hepatopancreatic ampulla enters the second part of the duodenum at the major duodenal papilla.
- Surrounding the ampulla is the sphincter of ampulla (collection of smooth muscles).
Accessory Pancreatic Duct
- Empties into the minor duodenal papilla just above the major duodenal papilla.
- Usually communicates with the main pancreatic duct.
Arterial Supply of the Pancreas
- Gastroduodenal artery from the common hepatic artery:
- Anterior superior pancreaticoduodenal artery.
- Posterior superior pancreaticoduodenal artery.
- Inferior pancreatic artery from the splenic artery:
- Dorsal pancreatic artery.
- Great pancreatic artery.
- Inferior pancreaticoduodenal artery from the superior mesenteric artery:
- Anterior inferior pancreaticoduodenal artery.
- Posterior inferior pancreaticoduodenal artery.
Venous and Lymphatic Drainage of the Pancreas
- Venous Drainage:
- Portal vein, superior mesenteric vein, splenic vein.
- Superior and inferior pancreaticoduodenal veins drain the head and uncinate process.
- Splenic vein drains the body and tail of the pancreas.
- Lymphatic Drainage: Extensive.
- Starts at interlobular septa within the gland, larger lymphatic vessels follow paths of arteries.
- Tail and body: Nodes along the splenic artery.
- Head and neck: Pre-aortic nodes.
- Starts at interlobular septa within the gland, larger lymphatic vessels follow paths of arteries.
Spleen
- Develops as part of the vascular system in the dorsal mesentery.
- Located in the left hypochondrium, against the diaphragm at Rib 9-Rib 10.
- Wedge-shaped organ, between the fundus of the stomach and diaphragm.
- Functions in phagocytosis, haematopoiesis, immune response, and storage of red blood cells.
- Splenic Hilum: Entry point for splenic vessels, the tail of the pancreas is related to this area.
- Anterior End: Expanded and reaches the midaxillary line.
- Posterior End: Rounded, rests on the upper pole of the left kidney.
- Superior Border: Notched on the anterior end (splenic notch).
- Inferior Border: Rounded.
- Impressions on the Visceral Surface: Gastric, renal, colic, pancreatic.
- Gastrosplenic Ligament: Attaches to the greater curvature of the stomach, containing short gastric and gastro-omental vessels.
- Splenorenal Ligament: Attaches to the left kidney, containing splenic vessels.
Vasculature of the Spleen
- Arterial Supply: Splenic artery, gives off a left gastro-omental artery.
- Venous Drainage: Splenic vein, joins the superior mesenteric vein to form the portal vein.
- Lymphatics: Pancreaticosplenic nodes.
- Nerve Supply: Coeliac plexus, sympathetic innervation.
Innervation of Accessory Organs
- Liver:
- Parenchyma supplied by the hepatic plexus:
- Sympathetic: Coeliac plexus.
- Parasympathetic: Vagus nerve fibres.
- Referred pain: Epigastric region for parenchyma, right shoulder for diaphragmatic surface, localized ‘somatic’ pain for fibrous capsule.
- Parenchyma supplied by the hepatic plexus:
- Spleen:
- Sympathetic: Coeliac plexus (dominant).
- Parasympathetic: Vagus nerve.
- Referred pain in the epigastric region.
- Gallbladder:
- Sympathetic and sensory fibres: Coeliac plexus.
- Parasympathetic fibres: Vagus nerve (stimulates gallbladder contraction).
- Referred pain: Right hypochondriac and epigastric regions, can radiate to the back, inferior to the right scapula.
- Pancreas:
- Sympathetic: Extra-pancreatic and intra-pancreatic plexuses of autonomic nerves.
- Parasympathetic: Vagal efferents reach the pancreas via hepatic, gastric, and coeliac branches of the vagus nerve.
- Referred pain localized to the lower thoracic spine due to inflammation of the pancreas involving the retroperitoneum, which is innervated by somatic nerves.
Clinical Relevance
-
ERCP (Endoscopic Retrograde Cholangiopancreatography):
- Used to remove obstructing gallstones within the biliary tree.
- Combines endoluminal endoscopy with fluoroscopy to diagnose and treat problems in biliary and pancreatic ducts.
- Endoscope is passed through the oesophagus and stomach to the second part of the duodenum where the major duodenal papilla is.
- Bile or pancreatic duct is cannulated, and contrast is injected into either the bile duct (cholangiogram) or pancreatic duct (pancreatogram).
-
Splenomegaly:
- Spleen is part of the reticuloendothelial system, involved in haematopoiesis and the immune system.
- Diseases such as leukaemia or lymphoma can cause generalized lymphadenopathy and splenomegaly.
- Spleen enlarges during normal physiological functioning.
- Can also occur due to increased venous pressure from heart failure, portal hypertension, or splenic vein thrombosis.
- Enlarged spleen is prone to rupture.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.