Podcast
Questions and Answers
Which part of the nephron is responsible for establishing a concentration gradient in the renal interstitium?
Which part of the nephron is responsible for establishing a concentration gradient in the renal interstitium?
- Proximal tubule
- Ascending loop of Henle (correct)
- Descending loop of Henle
- Collecting duct
What is the approximate osmolarity of the tubular fluid entering the descending loop of Henle?
What is the approximate osmolarity of the tubular fluid entering the descending loop of Henle?
- 100 mOsm
- 500 mOsm
- 300 mOsm (correct)
- 1200 mOsm
What is the mechanism by which the thick ascending loop of Henle actively transports solutes?
What is the mechanism by which the thick ascending loop of Henle actively transports solutes?
- Facilitated diffusion
- Active transport (correct)
- Passive diffusion
- Osmosis
Why does the tubular fluid in the descending loop of Henle quickly equilibrate with the interstitial fluid?
Why does the tubular fluid in the descending loop of Henle quickly equilibrate with the interstitial fluid?
What is the maximum concentration gradient that can be created by the active pump in the thick ascending loop of Henle?
What is the maximum concentration gradient that can be created by the active pump in the thick ascending loop of Henle?
How does the fluid flow from the proximal tubule contribute to the process of concentrating the renal interstitium?
How does the fluid flow from the proximal tubule contribute to the process of concentrating the renal interstitium?
What is the primary mechanism responsible for increasing the osmolarity of the renal interstitium over time?
What is the primary mechanism responsible for increasing the osmolarity of the renal interstitium over time?
What is the final approximate osmolarity of the renal interstitium after the concentration gradient is fully established?
What is the final approximate osmolarity of the renal interstitium after the concentration gradient is fully established?
What is the primary mechanism responsible for the further dilution of the tubular fluid as it flows through the early distal tubule?
What is the primary mechanism responsible for the further dilution of the tubular fluid as it flows through the early distal tubule?
What is the role of antidiuretic hormone (ADH) in the regulation of water reabsorption in the cortical collecting tubule?
What is the role of antidiuretic hormone (ADH) in the regulation of water reabsorption in the cortical collecting tubule?
Which of the following correctly describes the role of urea in the formation of concentrated urine?
Which of the following correctly describes the role of urea in the formation of concentrated urine?
Which of the following statements regarding the reabsorption of urea is INCORRECT?
Which of the following statements regarding the reabsorption of urea is INCORRECT?
What is the primary factor responsible for maintaining the high osmolarity of the renal medulla?
What is the primary factor responsible for maintaining the high osmolarity of the renal medulla?
Why is the reabsorption of water minimal in the ascending limb of the loop of Henle?
Why is the reabsorption of water minimal in the ascending limb of the loop of Henle?
Which of the following segments of the nephron is most responsible for the final concentration of urine?
Which of the following segments of the nephron is most responsible for the final concentration of urine?
Which of the following statements accurately represents the relationship between ADH and urea reabsorption?
Which of the following statements accurately represents the relationship between ADH and urea reabsorption?
What happens to the osmolarity of tubular fluid as it flows down the descending loop of Henle?
What happens to the osmolarity of tubular fluid as it flows down the descending loop of Henle?
Which statement correctly describes the characteristics of the ascending loop of Henle?
Which statement correctly describes the characteristics of the ascending loop of Henle?
What is the osmolarity of fluid leaving the distal tubular segment?
What is the osmolarity of fluid leaving the distal tubular segment?
In the absence of ADH, how does the renal system manage the tubular fluid in distal segments?
In the absence of ADH, how does the renal system manage the tubular fluid in distal segments?
How does the kidney adjust to maintain fluid balance when producing urine?
How does the kidney adjust to maintain fluid balance when producing urine?
What happens to the osmolarity of urine when there is excess water in the body?
What happens to the osmolarity of urine when there is excess water in the body?
What effect does the presence of ADH have on urine concentration?
What effect does the presence of ADH have on urine concentration?
Which of the following best describes the urine concentration capability of human kidneys?
Which of the following best describes the urine concentration capability of human kidneys?
How does antidiuretic hormone (ADH) affect urine concentration?
How does antidiuretic hormone (ADH) affect urine concentration?
What effect does a high osmolarity in bodily fluids have on the secretion of ADH?
What effect does a high osmolarity in bodily fluids have on the secretion of ADH?
What determines the volume and concentration of urine produced by the kidneys?
What determines the volume and concentration of urine produced by the kidneys?
Which segment of the nephron allows for equal reabsorption of solutes and water, maintaining osmolarity?
Which segment of the nephron allows for equal reabsorption of solutes and water, maintaining osmolarity?
During extreme hydration, how much dilute urine can kidneys excrete in a day?
During extreme hydration, how much dilute urine can kidneys excrete in a day?
What occurs to the filtrate osmolarity as it passes through the glomerulus?
What occurs to the filtrate osmolarity as it passes through the glomerulus?
When the kidneys excrete concentrated urine, what happens to solute excretion?
When the kidneys excrete concentrated urine, what happens to solute excretion?
What is a key function of the distal tubule and collecting ducts in the kidneys?
What is a key function of the distal tubule and collecting ducts in the kidneys?
What primary mechanism contributes to the hyperosmolarity of the renal medulla?
What primary mechanism contributes to the hyperosmolarity of the renal medulla?
Which component is essential for the kidney to form concentrated urine?
Which component is essential for the kidney to form concentrated urine?
What is the typical osmolarity of the renal interstitial fluid compared to that of the plasma?
What is the typical osmolarity of the renal interstitial fluid compared to that of the plasma?
Which anatomical structure plays a crucial role in maintaining the osmotic gradient for water absorption in the kidneys?
Which anatomical structure plays a crucial role in maintaining the osmotic gradient for water absorption in the kidneys?
Which process primarily occurs in the thick ascending limb of the loop of Henle to facilitate solute concentration?
Which process primarily occurs in the thick ascending limb of the loop of Henle to facilitate solute concentration?
What is the significance of the countercurrent multiplier mechanism in the kidney?
What is the significance of the countercurrent multiplier mechanism in the kidney?
How does urea contribute to the osmolarity of the renal medulla?
How does urea contribute to the osmolarity of the renal medulla?
What factors limit the urine concentrating ability in the kidneys?
What factors limit the urine concentrating ability in the kidneys?
Flashcards
Urine Concentration & Dilution
Urine Concentration & Dilution
The ability of kidneys to adjust the concentration of urine based on the body's water needs. This is crucial for maintaining fluid balance and overall health.
Antidiuretic Hormone (ADH) or Vasopressin
Antidiuretic Hormone (ADH) or Vasopressin
The hormone that controls water reabsorption in the kidneys, affecting urine concentration. When ADH levels are high, water reabsorption is increased, leading to concentrated urine. When ADH levels are low, water reabsorption is decreased, leading to dilute urine.
Urine Formation
Urine Formation
The process of removing waste products from the blood and forming urine. This process begins in the glomerulus, where blood is filtered, and continues through the tubules, where substances are reabsorbed or secreted.
Tubular Secretion
Tubular Secretion
Signup and view all the flashcards
Tubular Reabsorption
Tubular Reabsorption
Signup and view all the flashcards
Proximal Tubule
Proximal Tubule
Signup and view all the flashcards
Distal Tubule & Collecting Ducts
Distal Tubule & Collecting Ducts
Signup and view all the flashcards
Urine Osmolarity
Urine Osmolarity
Signup and view all the flashcards
Osmosis
Osmosis
Signup and view all the flashcards
Renal Medulla
Renal Medulla
Signup and view all the flashcards
Concentration of Filtrate in Descending Loop
Concentration of Filtrate in Descending Loop
Signup and view all the flashcards
Ascending Loop of Henle
Ascending Loop of Henle
Signup and view all the flashcards
Dilution of Filtrate in Ascending Loop
Dilution of Filtrate in Ascending Loop
Signup and view all the flashcards
Hypo-osmotic Filtrate
Hypo-osmotic Filtrate
Signup and view all the flashcards
Dilute Urine Formation
Dilute Urine Formation
Signup and view all the flashcards
Concentrated Urine Production
Concentrated Urine Production
Signup and view all the flashcards
Active Transport in Thick Ascending Limb
Active Transport in Thick Ascending Limb
Signup and view all the flashcards
Water Permeability in Thin Descending Limb
Water Permeability in Thin Descending Limb
Signup and view all the flashcards
Hyperosmotic Renal Interstitium
Hyperosmotic Renal Interstitium
Signup and view all the flashcards
Fluid Flow Through Descending Limb
Fluid Flow Through Descending Limb
Signup and view all the flashcards
Countercurrent Mechanism
Countercurrent Mechanism
Signup and view all the flashcards
Amplification of Osmolarity Gradient
Amplification of Osmolarity Gradient
Signup and view all the flashcards
Maximum Interstitial Osmolarity
Maximum Interstitial Osmolarity
Signup and view all the flashcards
Urine Concentration
Urine Concentration
Signup and view all the flashcards
Obligatory Urine Volume
Obligatory Urine Volume
Signup and view all the flashcards
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Signup and view all the flashcards
Osmotic Gradient
Osmotic Gradient
Signup and view all the flashcards
Countercurrent Multiplier Mechanism
Countercurrent Multiplier Mechanism
Signup and view all the flashcards
Hyperosmolarity of Renal Medulla
Hyperosmolarity of Renal Medulla
Signup and view all the flashcards
Active Transport in Thick Ascending Loop
Active Transport in Thick Ascending Loop
Signup and view all the flashcards
Urea Diffusion
Urea Diffusion
Signup and view all the flashcards
Urine Concentrating Ability
Urine Concentrating Ability
Signup and view all the flashcards
Cortical Collecting Tubule
Cortical Collecting Tubule
Signup and view all the flashcards
Descending Limb of Loop of Henle
Descending Limb of Loop of Henle
Signup and view all the flashcards
Ascending Limb of Loop of Henle
Ascending Limb of Loop of Henle
Signup and view all the flashcards
Urea Transporter
Urea Transporter
Signup and view all the flashcards
Study Notes
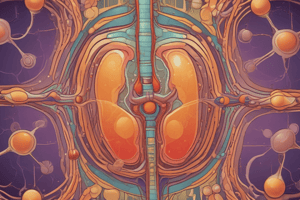
Urine Concentration and Dilution
- Kidneys regulate urine composition based on body water levels and osmolarity.
- Excess water results in dilute urine (osmolarity as low as 50 mOsm/L).
- Dehydration leads to concentrated urine (osmolarity of 1200-1400 mOsm/L).
- Urine volume can change while solute excretion remains relatively constant.
Antidiuretic Hormone (ADH)
- ADH (vasopressin) regulates water excretion independently of solutes.
- Increased osmolarity triggers ADH release, increasing water permeability in distal tubules & collecting ducts.
- This reduces urine volume but doesn't affect solute excretion.
- Reduced ADH leads to decreased water permeability, promoting dilute urine excretion.
Tubular Reabsorption
- Proximal tubules reabsorb water and solutes proportionally, maintaining near-equal osmolarity.
- Descending loop of Henle: Water reabsorption through osmosis, increasing filtrate osmolarity.
- Ascending loop of Henle (thick segment): Active solute (sodium, chloride, potassium) reabsorption, and impermeability to water which decreases filtrate osmolarity.
- Distal tubules and collecting ducts: ADH-dependent water reabsorption, further solute reabsorption regardless of ADH levels, and promoting dilute or concentrated urine output.
Urine Concentration Mechanisms
- Countercurrent multiplier mechanism creates a hyperosmotic renal medullary environment.
- Loops of Henle and vasa recta work together to establish this osmotic gradient.
- Solutes, primarily sodium and chloride, drive higher osmolarity within medulla.
- Urea passively diffuses out of the collecting duct into medulla, increasing medullary osmolarity.
Dilute Urine Formation
- Water reabsorption is reduced in distal segments while solute reabsorption continues.
- Fluid leaving ascending loop of Henle and early distal tubules is always dilute, irrespective of ADH levels.
- Absence of ADH leads to further dilution in distal tubules & collecting ducts, producing a large volume of dilute urine.
Urine Concentrating Ability
- Kidneys can concentrate urine up to 4-5 times the plasma osmolarity.
- High ADH levels are crucial for maximal urine concentration.
- High interstitial osmolarity in medulla provides the osmotic gradient for water reabsorption.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.