Podcast
Questions and Answers
What is the primary function of the kidneys in maintaining homeostasis?
What is the primary function of the kidneys in maintaining homeostasis?
- Maintaining the concentration of most of the constituents of body fluids (correct)
- Regulating the concentration of oxygen in the body
- Filtering out waste products from the digestive system
- Producing hormones to regulate blood pressure
What is the functional unit of the kidney?
What is the functional unit of the kidney?
- Bowman's capsule
- Glomerulus
- Renal tubule
- Nephron (correct)
What is the function of the proximal convoluted tubule?
What is the function of the proximal convoluted tubule?
- Filtration of plasma
- Regulation of blood pressure
- Reabsorption of glucose, Na+, K+, HCO3, and H2O (correct)
- Secretion of K+ and H+
What is the function of the loop of Henle?
What is the function of the loop of Henle?
What is the function of the distal convoluted tubule?
What is the function of the distal convoluted tubule?
What percentage of the cardiac output is received by the kidneys?
What percentage of the cardiac output is received by the kidneys?
What is the term for the renal plasma flow that becomes glomerular filtrate?
What is the term for the renal plasma flow that becomes glomerular filtrate?
What is the function of the juxtaglomerular apparatus?
What is the function of the juxtaglomerular apparatus?
What is the main function of secretion in the glomerular filtration process?
What is the main function of secretion in the glomerular filtration process?
What is the glomerular filtration rate (GFR) in milliliters per minute?
What is the glomerular filtration rate (GFR) in milliliters per minute?
What is the effect of an increase in osmotic pressure of Bowman's capsule on GFR?
What is the effect of an increase in osmotic pressure of Bowman's capsule on GFR?
What is the composition of the glomerular filtrate?
What is the composition of the glomerular filtrate?
Why does an increase in ABP have little effect on GFR?
Why does an increase in ABP have little effect on GFR?
What is the function of the basement membrane in the glomerular capillary membrane?
What is the function of the basement membrane in the glomerular capillary membrane?
What are the two forces that help filtration in the glomerular capillary membrane?
What are the two forces that help filtration in the glomerular capillary membrane?
What is the primary mechanism of active reabsorption in the proximal tubule?
What is the primary mechanism of active reabsorption in the proximal tubule?
What is the net filtration pressure in the glomerular capillary membrane?
What is the net filtration pressure in the glomerular capillary membrane?
What is the normal fasting blood glucose level?
What is the normal fasting blood glucose level?
What is the effect of an increase in glomerular hydrostatic pressure on the glomerular filtration rate?
What is the effect of an increase in glomerular hydrostatic pressure on the glomerular filtration rate?
What is the renal threshold for glucose?
What is the renal threshold for glucose?
What is the effect of a decrease in plasma proteins on the glomerular filtration rate?
What is the effect of a decrease in plasma proteins on the glomerular filtration rate?
What is the term for the abnormal excretion of glucose in the urine?
What is the term for the abnormal excretion of glucose in the urine?
What is the primary mechanism of sodium reabsorption and excretion in the kidneys?
What is the primary mechanism of sodium reabsorption and excretion in the kidneys?
What is the result of a decrease in GFR on urea excretion?
What is the result of a decrease in GFR on urea excretion?
What is the primary function of a chemical buffer system?
What is the primary function of a chemical buffer system?
Which buffer system is considered the strongest due to its huge amount?
Which buffer system is considered the strongest due to its huge amount?
How does the respiratory system control pH in the blood?
How does the respiratory system control pH in the blood?
What is the primary mechanism of water reabsorption in proximal tubules?
What is the primary mechanism of water reabsorption in proximal tubules?
What is the effect of aldosterone on sodium retention?
What is the effect of aldosterone on sodium retention?
What is the response of the respiratory system in case of acidosis?
What is the response of the respiratory system in case of acidosis?
What is the normal daily intake of potassium in an adult?
What is the normal daily intake of potassium in an adult?
How do the kidneys regulate pH in the body?
How do the kidneys regulate pH in the body?
What are the two types of acidosis and alkalosis?
What are the two types of acidosis and alkalosis?
What is the effect of ADH on urine concentration?
What is the effect of ADH on urine concentration?
What is the primary source of hydrogen ions in the body?
What is the primary source of hydrogen ions in the body?
What is the effect of diabetes insipidus on water balance?
What is the effect of diabetes insipidus on water balance?
What is the primary mechanism of regulating H+ concentration in the body?
What is the primary mechanism of regulating H+ concentration in the body?
What is the effect of osmotic diuretics on sodium reabsorption?
What is the effect of osmotic diuretics on sodium reabsorption?
Flashcards are hidden until you start studying
Study Notes
Kidney Function
- The kidneys perform two major functions: excreting end products of body metabolism (e.g., urea, uric acid) and maintaining the concentration of body fluid constituents (e.g., volume, ions, osmotic pressure).
- The kidneys play a crucial role in homeostasis.
- The kidneys produce renin and prostaglandins, which affect blood pressure.
- The kidneys produce renal erythropoietin, which helps synthesize red blood cells.
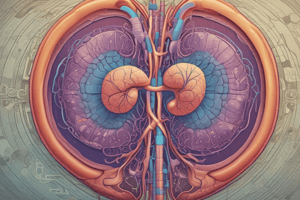
Functional Anatomy of the Kidney
- The functional unit of the kidney is the nephron, which consists of:
- Glomerulus (tuft of capillaries between two arterioles, embedded in Bowman's capsule) + Function: Filtration of plasma
- Renal tubule: - Proximal convoluted tubule: brush luminal border (microvilli), mitochondria for energy for active transport - Function: Reabsorption of glucose, Na+, K+, HCO3, H2O, and amino acids - Loop of Henle: - Descending and ascending limbs - Distal convoluted tubule >> collecting tubules >> renal pelvis - Function: + Reabsorption of Na+ (aldosterone), H2O (ADH) + Secretion of K+ (aldosterone) and H+
Blood Supply
- Each kidney contains about 1.3 million nephrons.
- The kidneys receive 20-25% of the cardiac output.
- The renal artery (a direct branch from the abdominal aorta) supplies blood to the kidney.
- The efferent arteriole gives rise to peritubular capillaries.
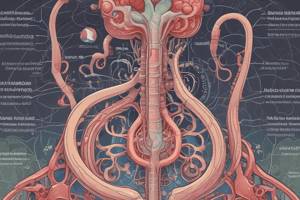
Formation of Urine
- Glomerular filtration: Plasma is filtered through the glomerular capillary membrane into the space of Bowman's capsule.
- Reabsorption: Transfer of substances from the lumen to the blood.
- Secretion: Transfer of substances from the blood to the lumen.
- Glomerular filtrate: Plasma minus plasma proteins.
- Glomerular filtration rate (GFR) = 125 ml/min = 180 L/day.
Glomerular Capillary Membrane
- Three layers: endothelial layer with pores (Fenestra), podocytes, and the basement membrane.
- 1% of albumin passes the membrane, which is cigar-shaped and negatively charged, decreasing diffusion.
Filtration Forces
- Two forces help filtration:
- Glomerular capillary pressure = 60 mmHg
- Osmotic pressure of proteins in Bowman's capsule = 0
- Two forces oppose filtration:
- Osmotic pressure of proteins in glomerulus = 32 mmHg
- Hydrostatic pressure in Bowman's capsule = 18 mmHg
Factors Affecting Glomerular Filtration
- Changes in filtration coefficient (Kf)
- Increases in glomerular hydrostatic pressure (e.g., increased blood pressure, dilation of afferent arteriole)
- Increases in hydrostatic pressure of Bowman's capsule (e.g., urine flow obstruction)
- Decreases in osmotic pressure of glomerular capillaries (e.g., decreased plasma proteins)
- Increases in osmotic pressure of Bowman's capsule (e.g., nephrotic syndrome)
Tubular Reabsorption
- Active reabsorption: Against concentration gradient, needs energy (e.g., Na+, K+, glucose, amino acids)
- Passive reabsorption: With concentration gradient, no energy required (e.g., glucose, amino acids, proteins, vitamins)
Glucose Reabsorption
- Completely reabsorbed by an active process in the proximal tubule
- Glucose level in blood: 70-110 mg/100 ml (fasting), 140 mg/100 ml (2 hours postprandial)
- Renal threshold for glucose: 180 mg/100 ml (above which glucose appears in urine)
Amino Acid Reabsorption
- Active reabsorption in the proximal convoluted tubule
Sodium Reabsorption and Excretion
- Mainly regulated by aldosterone
- 99% of Na+ filtered is reabsorbed in renal tubules
- Diuretics inhibit tubular sodium and water reabsorption
Potassium Regulation
- Normal plasma level: 3.5-5 mEq/L
- Daily intake: 100 mEq, excreted in urine (90 mEq) and feces (10 mEq)
- Factors increasing renal potassium excretion:
- High potassium diet
- Aldosterone in the distal convoluted tubule
- Renal failure leads to increased potassium levels in blood
Water Reabsorption and Excretion
- Obligatory water reabsorption in the proximal tubules
- Facultative water reabsorption in the late distal and collecting tubules, regulated by ADH
- Diabetes insipidus: Deficiency of ADH (pituitary) or failure of the kidney to respond to ADH (nephrogenic)
Regulation of H+ Concentration (Acid-Base Balance)
- Hydrogen ion concentration is kept constant (pH = 7.4)
- Sources of hydrogen ions in the body: metabolic processes
- Mechanism of acid-base balance:
- Rapidly acting (chemical buffers): seconds to minutes
- Intermediate acting (respiratory regulation): minutes to hours
- Slowly acting (renal regulation): hours to days
Chemical Buffers
- Buffer systems: Weak acids + salts of their conjugate base (e.g., H2CO3 + NaHCO3)
- Bicarbonate-carbonic acid system: Not a powerful buffer
- Protein buffer system: Plasma proteins (7 gm/100 cc) and hemoglobin (15 gm/100 cc) act as weak acids
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.