Podcast
Questions and Answers
What process allows water to follow nutrients out of the proximal tubule?
What process allows water to follow nutrients out of the proximal tubule?
- Filtration
- Osmosis (correct)
- Diffusion
- Active transport
What role does the macula densa play in the kidney's function?
What role does the macula densa play in the kidney's function?
- Detecting changes in sodium chloride concentration (correct)
- Producing renin
- Filtering blood
- Regulating blood flow
What component is crucial for the renin-angiotensin-aldosterone system (RAAS)?
What component is crucial for the renin-angiotensin-aldosterone system (RAAS)?
- Aldosterone
- Natriuretic peptide
- Renin (correct)
- Antidiuretic hormone
How do ions, drugs, and toxins enter the distal tubule?
How do ions, drugs, and toxins enter the distal tubule?
What is the primary function of the juxtaglomerular apparatus (JGA)?
What is the primary function of the juxtaglomerular apparatus (JGA)?
What characteristic of the Loop of Henle facilitates water reabsorption?
What characteristic of the Loop of Henle facilitates water reabsorption?
What cellular component assists in communication between the macula densa and juxtaglomerular cells?
What cellular component assists in communication between the macula densa and juxtaglomerular cells?
What mechanism is primarily responsible for the reabsorption of water in the collecting duct?
What mechanism is primarily responsible for the reabsorption of water in the collecting duct?
What is a primary function of the urinary system?
What is a primary function of the urinary system?
Which structure is NOT part of the urinary system?
Which structure is NOT part of the urinary system?
What is the primary role of the renal pelvis in the kidney?
What is the primary role of the renal pelvis in the kidney?
Where are the kidneys located in the body?
Where are the kidneys located in the body?
Which part of the kidney is responsible for urine production?
Which part of the kidney is responsible for urine production?
Which structure in the kidney contains triangular regions of tissue?
Which structure in the kidney contains triangular regions of tissue?
Which statement about the locations of kidneys is accurate?
Which statement about the locations of kidneys is accurate?
What are calyces in the kidney responsible for?
What are calyces in the kidney responsible for?
What structures compose each nephron?
What structures compose each nephron?
Which layer of Bowman’s capsule directly envelopes the capillaries of the glomerulus?
Which layer of Bowman’s capsule directly envelopes the capillaries of the glomerulus?
What is the primary function of the glomerulus?
What is the primary function of the glomerulus?
Which type of nephron is located entirely in the cortical region of the kidney?
Which type of nephron is located entirely in the cortical region of the kidney?
What role does blood pressure play in the function of the glomerulus?
What role does blood pressure play in the function of the glomerulus?
What begins at the urinary pole of each renal corpuscle?
What begins at the urinary pole of each renal corpuscle?
What structure is interposed between the visceral and parietal layers of Bowman’s capsule?
What structure is interposed between the visceral and parietal layers of Bowman’s capsule?
How does the structure of the glomerulus facilitate filtration?
How does the structure of the glomerulus facilitate filtration?
What is the primary function of the kidneys in relation to urine?
What is the primary function of the kidneys in relation to urine?
Which hormone produced by the kidneys stimulates red blood cell production?
Which hormone produced by the kidneys stimulates red blood cell production?
What occurs during the filtration process in the kidneys?
What occurs during the filtration process in the kidneys?
How do the kidneys contribute to blood pressure regulation?
How do the kidneys contribute to blood pressure regulation?
Which of the following statements about urine formation is correct?
Which of the following statements about urine formation is correct?
What role does the enzyme renin play in the RAAS?
What role does the enzyme renin play in the RAAS?
Which of these functions is NOT performed by the kidneys?
Which of these functions is NOT performed by the kidneys?
What is a primary outcome of the kidneys' regulatory functions?
What is a primary outcome of the kidneys' regulatory functions?
What is the primary function of angiotensin II in response to low blood pressure?
What is the primary function of angiotensin II in response to low blood pressure?
Which enzyme is responsible for converting angiotensinogen to angiotensin I?
Which enzyme is responsible for converting angiotensinogen to angiotensin I?
How does aldosterone primarily affect the kidneys?
How does aldosterone primarily affect the kidneys?
Which physiological response occurs when the sympathetic nervous system is activated due to low blood pressure?
Which physiological response occurs when the sympathetic nervous system is activated due to low blood pressure?
What role does ACE play in the renin-angiotensin system?
What role does ACE play in the renin-angiotensin system?
What triggers the release of renin from the juxtaglomerular cells?
What triggers the release of renin from the juxtaglomerular cells?
What is one of the effects of angiotensin II on the blood vessels?
What is one of the effects of angiotensin II on the blood vessels?
Which hormone is released by the pituitary gland to help reabsorb water in the kidneys?
Which hormone is released by the pituitary gland to help reabsorb water in the kidneys?
What physiological process is inhibited when blood pressure and volume return to normal?
What physiological process is inhibited when blood pressure and volume return to normal?
What is the role of erythropoietin in maintaining homeostasis?
What is the role of erythropoietin in maintaining homeostasis?
Which substance converts ammonia into a less toxic form?
Which substance converts ammonia into a less toxic form?
What is the main effect of antidiuretic hormone (ADH) on the kidneys?
What is the main effect of antidiuretic hormone (ADH) on the kidneys?
How does alcohol contribute to dehydration during a hangover?
How does alcohol contribute to dehydration during a hangover?
Which hormones are primarily produced by the kidneys that help control blood pressure and volume?
Which hormones are primarily produced by the kidneys that help control blood pressure and volume?
What role do ACE inhibitors play in treating hypertension?
What role do ACE inhibitors play in treating hypertension?
What effect do caffeine and alcohol have on the action of ADH?
What effect do caffeine and alcohol have on the action of ADH?
Flashcards
Nephron
Nephron
The functional unit of the kidney, responsible for filtering blood and producing urine.
Renal Cortex
Renal Cortex
The outer region of the kidney, containing the glomeruli and convoluted tubules.
Renal Medulla
Renal Medulla
The inner region of the kidney, containing the collecting ducts and loops of Henle.
Renal Pelvis
Renal Pelvis
Signup and view all the flashcards
Calyces
Calyces
Signup and view all the flashcards
Medullary Pyramids
Medullary Pyramids
Signup and view all the flashcards
Renal Columns
Renal Columns
Signup and view all the flashcards
Urine Formation
Urine Formation
Signup and view all the flashcards
What is a nephron?
What is a nephron?
Signup and view all the flashcards
What is the glomerulus?
What is the glomerulus?
Signup and view all the flashcards
What is Bowman's capsule?
What is Bowman's capsule?
Signup and view all the flashcards
What is the urinary space?
What is the urinary space?
Signup and view all the flashcards
What is the vascular pole?
What is the vascular pole?
Signup and view all the flashcards
What is the urinary pole?
What is the urinary pole?
Signup and view all the flashcards
What are cortical nephrons?
What are cortical nephrons?
Signup and view all the flashcards
What are juxtamedullary nephrons?
What are juxtamedullary nephrons?
Signup and view all the flashcards
Proximal Tubule: Role in Nutrient Reabsorption
Proximal Tubule: Role in Nutrient Reabsorption
Signup and view all the flashcards
Loop of Henle: Concentrating Urine
Loop of Henle: Concentrating Urine
Signup and view all the flashcards
Distal Tubule: Fine-Tuning Urine
Distal Tubule: Fine-Tuning Urine
Signup and view all the flashcards
Collecting Duct: Final Water Removal
Collecting Duct: Final Water Removal
Signup and view all the flashcards
Juxtaglomerular Apparatus (JGA)
Juxtaglomerular Apparatus (JGA)
Signup and view all the flashcards
Macula Densa: Sensing Salt
Macula Densa: Sensing Salt
Signup and view all the flashcards
Juxtaglomerular (JG) Cells: Renin Production
Juxtaglomerular (JG) Cells: Renin Production
Signup and view all the flashcards
Extraglomerular Mesangial Cells: Communication Hub
Extraglomerular Mesangial Cells: Communication Hub
Signup and view all the flashcards
Kidney Filtration
Kidney Filtration
Signup and view all the flashcards
Kidney Regulation
Kidney Regulation
Signup and view all the flashcards
Renin Production
Renin Production
Signup and view all the flashcards
Erythropoietin Production
Erythropoietin Production
Signup and view all the flashcards
Vitamin D Conversion
Vitamin D Conversion
Signup and view all the flashcards
Nitrogenous Waste Removal
Nitrogenous Waste Removal
Signup and view all the flashcards
Kidney Homeostasis
Kidney Homeostasis
Signup and view all the flashcards
How does the body regulate blood pressure?
How does the body regulate blood pressure?
Signup and view all the flashcards
What role does the SNS play in blood pressure regulation?
What role does the SNS play in blood pressure regulation?
Signup and view all the flashcards
What is the RAAS?
What is the RAAS?
Signup and view all the flashcards
How does Angiotensin II affect blood pressure?
How does Angiotensin II affect blood pressure?
Signup and view all the flashcards
What does Aldosterone do?
What does Aldosterone do?
Signup and view all the flashcards
What is the function of ADH?
What is the function of ADH?
Signup and view all the flashcards
What triggers the RAAS?
What triggers the RAAS?
Signup and view all the flashcards
What is the role of renin?
What is the role of renin?
Signup and view all the flashcards
How does erythropoietin help maintain homeostasis?
How does erythropoietin help maintain homeostasis?
Signup and view all the flashcards
What is the role of the liver in ammonia metabolism?
What is the role of the liver in ammonia metabolism?
Signup and view all the flashcards
What is the role of ADH in water balance?
What is the role of ADH in water balance?
Signup and view all the flashcards
How do alcohol and caffeine affect ADH?
How do alcohol and caffeine affect ADH?
Signup and view all the flashcards
What causes dehydration after drinking alcohol?
What causes dehydration after drinking alcohol?
Signup and view all the flashcards
Why is coffee not a good cure for a hangover?
Why is coffee not a good cure for a hangover?
Signup and view all the flashcards
What is the amine unit and how is it removed from amino acids?
What is the amine unit and how is it removed from amino acids?
Signup and view all the flashcards
Study Notes
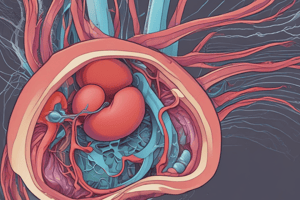
Urinary System Overview
- The Urinary System is responsible for water control and nitrogen disposal.
- It comprises several key organs: kidneys, ureters, urinary bladder, and urethra.
Organs of the Urinary System
- Kidneys: Bean-shaped organs located in the dorsal body wall, between T12 and L3 vertebrae. The right kidney is positioned slightly lower than the left. Attached to ureters, renal blood vessels, and nerves at the renal hilus. Each kidney has an adrenal gland.
- Ureters: Slender tubes connecting the kidneys to the bladder. They run behind the peritoneum. Peristalsis aids in urine transport.
- Urinary Bladder: A smooth, collapsible muscular sac that temporarily stores urine. It extends significantly without causing increased internal pressure.
- Urethra: A thin-walled tube carrying urine from the bladder to the exterior. Urine release is controlled by internal and external sphincters.
- Note gender-specific urethra differences: length and location
Kidney Structures
- Each kidney has a concave medial border, hilum, and convex lateral border.
- Blood and lymph vessels and nerves enter and exit through the hilum.
- Medullary pyramids - triangular regions of tissue in the medulla.
- Renal columns - extensions of cortex-like material inward.
- Calyces: cup-shaped structures funneling urine toward the renal pelvis.
Regions of the Kidney
- Renal cortex: The outer region of the kidney.
- Renal medulla: Located inside the cortex.
- Renal pelvis: The inner collecting tube of the kidney.
Kidney Division
- The kidney is divided into an outer cortex and inner medulla.
- The medulla consists of conical or pyramidal structures called medullary pyramids.
- Medullary rays arise from the base of each medullary pyramid and are parallel arrays of tubules.
Kidney Size
- An adult kidney measures approximately 12 cm (5 inches) in length, 6 cm (2.5 inches) in width, and 3 cm (1 inch) in thickness.
Anatomy of the Kidney
- The main structures of the mammalian kidney include: kidney cortex, renal medulla, renal pelvis, and nephrons.
Blood Flow in the Kidneys
- Blood flows from the aorta through renal, segmental, lobar, interlobar, arcuate, and interlobular arteries.
- Blood then flows through the glomerulus (capillaries) into peritubular capillaries.
- The blood exits through interlobular and other veins.
Anatomy of the Nephron
- Glomerulus: A tuft of capillaries surrounded by Bowman's capsule. Filtration occurs here.
- Proximal tubule: Receives the filtered fluid from Bowman's capsule.
- Loop of Henle: Establishes a concentration gradient for water reabsorption.
- Distal tubule: Reabsorbs essential substances and secretes wastes.
- Collecting duct: Collects the filtrate from several nephrons before it becomes urine.
Nephron
- An individual kidney contains around 4 million nephrons; each nephron is the kidney's fundamental unit.
- Each nephron comprises a renal corpuscle and a renal tubule.
- The renal corpuscle is a double-walled epithelial capsule, Bowman's capsule, enclosing the glomerulus (a tuft of capillaries).
Renal Corpuscles
- Each renal corpuscle is about 200 µm in diameter.
- It comprises a tuft of capillaries, glomerulus.
- The glomerulus is encompassed by a double-walled epithelial capsule, Bowman's capsule, which has an internal layer (visceral) and an external layer (parietal).
- The urinary space is present between the parietal and visceral layers.
- Afferent arterioles enter, and efferent arterioles leave through the vascular pole.
- The proximal convoluted tubule starts at the urinary pole.
Glomerulus, filtration of blood
- The glomerulus acts as the sole filtration site.
- Blood pressure pushes plasma through capillary walls into Bowman's capsule.
Proximal Tubule, reabsorption of materials
- Nutrients (salts, vitamins) are moved out of the proximal tubule through active transport.
- Water follows the nutrients by osmosis.
Loop of Henle
- Interstitial fluid surrounding the loop of Henle is elevated in sodium chloride concentration.
- This enables water to passively diffuse out of the loop.
Distal Tubule, secretion of wastes, control of ions
- Active transport is instrumental in releasing more nutrients and regulating the level of concentrated urine.
- Ions, drugs, and toxins are also actively secreted into the tubule.
Collecting Duct
- Water is passively released from the tube through osmosis, as the tube is surrounded by saline tissue.
- Urea is removed through diffusion.
Juxtaglomerular Apparatus (JGA)
- A specialized structure near the glomerulus.
- A crucial component of the nephron and plays a vital role in regulating blood pressure, blood volume, and filtration rate.
Blood Pressure Regulation (RAAS)
- Renin is released by the JGA in response to low BP.
- Renin converts angiotensinogen (liver protein) to angiotensin I.
- Angiotensin-converting enzyme (ACE) converts angiotensin I into angiotensin II.
- Angiotensin II causes vasoconstriction and stimulates aldosterone release.
- Aldosterone retains water and sodium, increasing blood volume and pressure.
Functions of the Kidney
- Filtration: Kidneys filter gallons of fluid from the bloodstream per day.
- Waste processing: The kidneys process the filtrate, removing wastes and excess ions to leave the body in urine while returning needed substances to the blood (e.g. salts, etc).
- Elimination: Kidneys are mainly responsible for eliminating nitrogenous wastes, toxins, and drugs from the body, however other organs play a role as well
Kidney Hormones
- Renin: Regulates blood pressure.
- Erythropoietin: Stimulates red blood cell production in the bone marrow.
- Vitamin D: Kidney cells convert vitamin D to its active form.
Urea Removal
- Kidneys remove urea from the bloodstream, urea being a result of proteins broken down in the body.
Amino Acid Metabolism and Ammonia
- The liver converts ammonia into urea.
- Ammonia is toxic, while urea is less toxic.
Regulating Water (ADH)
- Antidiuretic hormone (ADH) regulates water balance.
- ADH increases the permeability of the distal tubule, which causes an increase in water recovery.
Caffeine and Alcohol
- Caffeine and alcohol are diuretics, they cause increased water loss.
- Alcohol inhibits ADH release.
- Caffeine interferes with ADH activity.
Water balance
- Water intake must equal water output.
- Water is necessary for numerous body functions.
Water and Electrolytes
- Changes in electrolyte balance lead to water movement between compartments.
Variations in Urine Production
- Dilute urine results from excessive water intake.
- Concentrated urine arises from significant water loss.
Kidney Development
- Functional kidneys typically develop during the third month of gestation.
- Newborns' bladders are smaller and cannot concentrate urine efficiently.
Aging and the Urinary System
- Aging involves decline in urinary function, bladder shrinkage, and increased urinary retention in males.
Urethra: Gender Differences
- Females have a short urethra, while males have a long one.
- Functionally, both genders' urethras only carry urine.
Voiding (Micturition)
- Voiding involves the simultaneous opening of both sphincters, (external and internal)
- The internal sphincter relaxes.
- Pelvic splanchnic nerves trigger the external sphincter relaxation.
Water Balance: Different Ages
- Young adults have different water composition percentages in their body compared to babies or old age individuals.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.