Podcast
Questions and Answers
Which part of the urinary bladder is located cranially?
Which part of the urinary bladder is located cranially?
- Body
- Vertex (correct)
- Neck
- Base
What type of epithelium lines the mucosa of the urinary bladder?
What type of epithelium lines the mucosa of the urinary bladder?
- Stratified cuboidal epithelium
- Columnar epithelium
- Transitional epithelium (correct)
- Simple squamous epithelium
What is the function of the median vesical ligament in the fetus?
What is the function of the median vesical ligament in the fetus?
- Supports the urinary bladder
- Houses the umbilical arteries
- Serves as a conduit for urine
- Contains the urachus (correct)
How many cell layers are typically seen in the transitional epithelium of the urinary bladder?
How many cell layers are typically seen in the transitional epithelium of the urinary bladder?
Which muscular layer of the urinary bladder is composed of circular muscle fibers?
Which muscular layer of the urinary bladder is composed of circular muscle fibers?
What happens to the epithelium of the bladder when it is empty?
What happens to the epithelium of the bladder when it is empty?
What is a characteristic of the lamina propria in the bladder?
What is a characteristic of the lamina propria in the bladder?
What structure collapses at birth and forms the round ligaments?
What structure collapses at birth and forms the round ligaments?
What is the primary function of principal cells in the collecting ducts?
What is the primary function of principal cells in the collecting ducts?
Which of the following correctly describes intercalated cells in the collecting ducts?
Which of the following correctly describes intercalated cells in the collecting ducts?
What is the role of aquaporin-2 channels in principal cells?
What is the role of aquaporin-2 channels in principal cells?
Where does urine from the collecting ducts ultimately empty?
Where does urine from the collecting ducts ultimately empty?
Which statement about the connecting tubule and collecting duct is accurate?
Which statement about the connecting tubule and collecting duct is accurate?
What happens to the function of podocytes in the glomerulus with age-related changes?
What happens to the function of podocytes in the glomerulus with age-related changes?
Which of the following is NOT a function of principal cells?
Which of the following is NOT a function of principal cells?
Why is the structure of the renal pelvis characterized by transitional epithelium?
Why is the structure of the renal pelvis characterized by transitional epithelium?
Which component of the glomerulus is primarily responsible for regulating blood flow?
Which component of the glomerulus is primarily responsible for regulating blood flow?
What is the primary function of the filtration slits formed by podocytes?
What is the primary function of the filtration slits formed by podocytes?
Which cells line the outer layer of Bowman's capsule?
Which cells line the outer layer of Bowman's capsule?
Which structure acts as a filtration barrier in the glomerulus?
Which structure acts as a filtration barrier in the glomerulus?
What is the role of juxtaglomerular cells?
What is the role of juxtaglomerular cells?
What happens to podocytes as a person ages?
What happens to podocytes as a person ages?
Which of the following best describes glomerular endothelial cells?
Which of the following best describes glomerular endothelial cells?
Which cells are classified as specialized epithelial cells covering the glomerular capillaries?
Which cells are classified as specialized epithelial cells covering the glomerular capillaries?
Flashcards are hidden until you start studying
Study Notes
Distal Convoluted Tubule and Collecting Tubule
- The distal convoluted tubule transitions gradually into the cortical collecting duct, and the connecting tubule is not clearly defined due to cell intermingling
- Two distinct cell types are present in the collecting tubules: principal cells (majority) and intercalated cells (minority)
- Principal cells are responsible for water reabsorption and are responsive to antidiuretic hormone (ADH)
- They have fewer and smaller microvilli
- They express aquaporin-2 channels
- They have channels and transporters for sodium and water reabsorption
- Intercalated cells regulate acid-base balance by secreting H+ and K+
- They have more and larger microvilli
- They do not respond to ADH
- They do not express aquaporin-2 channels
- They have channels and transporters for hydrogen ion and potassium secretion
Renal Papilla
- The renal papilla is the site where urine in the collecting ducts empties into the renal pelvis
- The renal pelvis is the initial dilated portion of the ureter
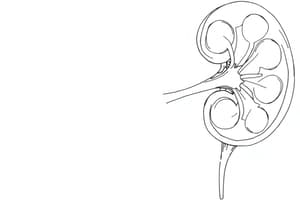
Urinary Bladder
- The urinary bladder is a musculo-membranous organ with varying size and shape depending on urine content
- The bladder has three main parts:
- Apex (cranial)
- Body
- Neck (continuous with urethra)
- The median and lateral vesical ligaments attach the urinary bladder to the pelvic cavity
- The median ligament contains the urachus in the fetus, and collapses at birth
- The lateral ligaments contain the umbilical arteries in the fetus, and collapse at birth to form the round ligaments
Urinary Bladder Histology
- The bladder wall has three layers:
- Mucosa: lined by transitional epithelium with three cell layers
- Cuboidal basal cells
- Intermediate cells
- Superficial cells
- Muscularis: three layers with connective tissue separating muscle fiber bundles
- Innermost and outermost layers: longitudinal muscle fibers
- Intermediate layer: circular muscle fibers
- Serosa: formed by the visceral peritoneum
- Mucosa: lined by transitional epithelium with three cell layers
Urethra
- Glomerulus Composition:
- Glomerular Endothelial Cells:
- Fenestrated capillaries with large, flat cells and large round fenestrations
- Podocytes (Glomerular Epithelial Cells):
- Cover the outer surface of the glomerular basement membrane
- Have pedicels (finger-like projections) that form filtration slits
- Intraglomerular Mesangial Cells:
- Contractile cells located in the glomerulus center
- Support glomerular capillaries and regulate blood flow
- Parietal Epithelial Cells:
- Line the outer layer of Bowman's capsule
- Continuous with the proximal convoluted tubule
- Glomerular Endothelial Cells:
Filtration Barrier
- The filtration barrier consists of:
- Fenestrated endothelium
- Glomerular basement membrane
- Glomerular visceral epithelium (podocyte pedicels)
Juxtaglomerular Apparatus
- Located at the vascular pole of the glomerulus
- Has two components:
- Vascular Component:
- Juxtaglomerular cells in the afferent arteriole terminal portion
- Modified smooth muscle cells that release renin
- Extend processes into the efferent arteriole initial portion
- Tubular Component:
- Macula densa cells in the distal convoluted tubule
- Specialized epithelial cells that sense sodium concentration in the tubular fluid
- Function: regulate blood pressure and filtration rate
- Vascular Component:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.