Podcast
Questions and Answers
Which of the following imaging findings is most consistent with Medullary Sponge Kidney?
Which of the following imaging findings is most consistent with Medullary Sponge Kidney?
- Multiple cysts of various sizes, which replace the normal renal parenchyma
- Multiple non-communicating cysts with absence of renal parenchyma
- Enlarged Kidneys bilaterally with hyperechoic parenchyma
- Bilateral hyperechoic medullary pyramids with or without shadowing (correct)
A 70-year-old patient presents with multiple cysts of varying sizes in both kidneys. Which of the following conditions should the patient be evaluated for?
A 70-year-old patient presents with multiple cysts of varying sizes in both kidneys. Which of the following conditions should the patient be evaluated for?
- Autosomal Dominant Polycystic Kidney Disease (ADPKD) (correct)
- Medullary Sponge Kidney
- Multicystic Dysplastic Kidneys (MCDK)
- Autosomal Recessive Polycystic Kidney Disease (ARPKD)
What is the most common cause of an abdominal mass in newborns?
What is the most common cause of an abdominal mass in newborns?
- Simple Renal Cysts
- Medullary Sponge Kidney
- Autosomal Recessive Polycystic Kidney Disease (ARPKD)
- Multicystic Dysplastic Kidneys (MCDK) (correct)
Which of the following is NOT a common complication associated with Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
Which of the following is NOT a common complication associated with Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
Which of the following criteria is NOT used to differentiate between a simple renal cyst and a complex renal cyst on ultrasound?
Which of the following criteria is NOT used to differentiate between a simple renal cyst and a complex renal cyst on ultrasound?
What is the most common location for simple renal cysts?
What is the most common location for simple renal cysts?
What complication is commonly associated with ARPKD?
What complication is commonly associated with ARPKD?
Which of the following is a characteristic sonographic finding of a simple renal cyst?
Which of the following is a characteristic sonographic finding of a simple renal cyst?
What is the typical age of onset for Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
What is the typical age of onset for Autosomal Dominant Polycystic Kidney Disease (ADPKD)?
Which of the following is NOT a feature of Multicystic Dysplastic Kidneys (MCDK)?
Which of the following is NOT a feature of Multicystic Dysplastic Kidneys (MCDK)?
What is a possible differential diagnosis to consider when a patient presents with hyperechoic renal pyramids?
What is a possible differential diagnosis to consider when a patient presents with hyperechoic renal pyramids?
Which type of renal cyst is also known as an atypical cyst?
Which type of renal cyst is also known as an atypical cyst?
What is the term used to describe the condition where one kidney undergoes hypertrophy to compensate for the loss of function of the other kidney?
What is the term used to describe the condition where one kidney undergoes hypertrophy to compensate for the loss of function of the other kidney?
Which of the following is a common finding in patients with Medullary Sponge Kidney?
Which of the following is a common finding in patients with Medullary Sponge Kidney?
What is the term used to describe a cyst located in the renal sinus?
What is the term used to describe a cyst located in the renal sinus?
What is the primary function of the ureters?
What is the primary function of the ureters?
Which structure exits posteriorly at the hilum of the kidney?
Which structure exits posteriorly at the hilum of the kidney?
What characterizes the renal cortex?
What characterizes the renal cortex?
Which embryonic kidney is non-functional and disappears around the 4th week of development?
Which embryonic kidney is non-functional and disappears around the 4th week of development?
What is the typical size range for human kidneys?
What is the typical size range for human kidneys?
Which anatomical structure is located superior and medial to the right kidney?
Which anatomical structure is located superior and medial to the right kidney?
What does the renal fascia do?
What does the renal fascia do?
In females, which ducts arise from mesonephros and eventually develop into the uterus and vagina?
In females, which ducts arise from mesonephros and eventually develop into the uterus and vagina?
What is a normal value for the resistive index (RI) in renal evaluation?
What is a normal value for the resistive index (RI) in renal evaluation?
Which patient condition is most likely to result in increased renal arterial resistance?
Which patient condition is most likely to result in increased renal arterial resistance?
In the Doppler evaluation technique, what is the maximum acceptable angle between the Doppler beam and the direction of flow?
In the Doppler evaluation technique, what is the maximum acceptable angle between the Doppler beam and the direction of flow?
What anatomical abnormality is commonly associated with unilateral renal agenesis?
What anatomical abnormality is commonly associated with unilateral renal agenesis?
Which of the following conditions does NOT typically result from renal duplication?
Which of the following conditions does NOT typically result from renal duplication?
What is the embryological origin of kidneys?
What is the embryological origin of kidneys?
What imaging finding is characteristic of a duplex kidney?
What imaging finding is characteristic of a duplex kidney?
In the case of crossed fused renal ectopia, where are two kidneys commonly located?
In the case of crossed fused renal ectopia, where are two kidneys commonly located?
What major complication can arise from ectopic kidneys?
What major complication can arise from ectopic kidneys?
Which syndrome is associated with renal agenesis and vertebral defects?
Which syndrome is associated with renal agenesis and vertebral defects?
What is the most common location for ectopic kidneys?
What is the most common location for ectopic kidneys?
What type of appearance does a horseshoe kidney have?
What type of appearance does a horseshoe kidney have?
What is a significant risk associated with hydronephrosis in congenital anomalies?
What is a significant risk associated with hydronephrosis in congenital anomalies?
What is the most common clinical manifestation of renal cell carcinoma?
What is the most common clinical manifestation of renal cell carcinoma?
In which condition are patients at an increased risk for developing renal cell carcinoma due to long-term dialysis?
In which condition are patients at an increased risk for developing renal cell carcinoma due to long-term dialysis?
What imaging characteristic is often suggestive of a renal oncocytoma?
What imaging characteristic is often suggestive of a renal oncocytoma?
Which of the following tumors is most commonly seen in childhood?
Which of the following tumors is most commonly seen in childhood?
What is a key imaging sign that must be documented in renal mass evaluations?
What is a key imaging sign that must be documented in renal mass evaluations?
Which group of tumors is characterized by the presence of fat cells intermixed with smooth muscle cells?
Which group of tumors is characterized by the presence of fat cells intermixed with smooth muscle cells?
What common feature is associated with both Von Hippel-Lindau disease and tuberous sclerosis?
What common feature is associated with both Von Hippel-Lindau disease and tuberous sclerosis?
What condition presents with multiple cysts in kidneys as a result of long-term dialysis?
What condition presents with multiple cysts in kidneys as a result of long-term dialysis?
What is the typical age range at which Von Hippel-Lindau disease usually presents symptoms?
What is the typical age range at which Von Hippel-Lindau disease usually presents symptoms?
Which renal tumor is characterized by a likely homogeneous and well-circumscribed echogenic mass?
Which renal tumor is characterized by a likely homogeneous and well-circumscribed echogenic mass?
Which type of urothelial carcinoma accounts for about 10% of such cancers?
Which type of urothelial carcinoma accounts for about 10% of such cancers?
What is the appearance of an infarcted area within 24 hours of arterial occlusion?
What is the appearance of an infarcted area within 24 hours of arterial occlusion?
The diagnosis of angiomyolipoma is confirmed by which imaging characteristic?
The diagnosis of angiomyolipoma is confirmed by which imaging characteristic?
Which mechanism is responsible for prerenal failure in Acute Kidney Injury (AKI)?
Which mechanism is responsible for prerenal failure in Acute Kidney Injury (AKI)?
How does a Wilms tumor commonly appear in imaging?
How does a Wilms tumor commonly appear in imaging?
What is a common sonographic finding in acute pyelonephritis?
What is a common sonographic finding in acute pyelonephritis?
Which factor is most commonly associated with emphysematous pyelonephritis?
Which factor is most commonly associated with emphysematous pyelonephritis?
What is the typical sonographic appearance of chronic pyelonephritis?
What is the typical sonographic appearance of chronic pyelonephritis?
What intervention is typically required for pyonephrosis?
What intervention is typically required for pyonephrosis?
What characterizes acute focal bacterial nephritis?
What characterizes acute focal bacterial nephritis?
Which bacterial type is most commonly involved in acute pyelonephritis?
Which bacterial type is most commonly involved in acute pyelonephritis?
Which condition involves the presence of fungal masses in the renal system?
Which condition involves the presence of fungal masses in the renal system?
What is the outcome of acute kidney injury if not addressed?
What is the outcome of acute kidney injury if not addressed?
What is a significant finding in patients with xanthogranulomatous pyelonephritis?
What is a significant finding in patients with xanthogranulomatous pyelonephritis?
What aspect often complicates fungal infections in renal cases?
What aspect often complicates fungal infections in renal cases?
How is acute tubular necrosis classified in terms of renal failure?
How is acute tubular necrosis classified in terms of renal failure?
What is Hydronephrosis primarily characterized by?
What is Hydronephrosis primarily characterized by?
Which grade of Hydronephrosis is characterized by mild distortion of pelvocaliceal structures?
Which grade of Hydronephrosis is characterized by mild distortion of pelvocaliceal structures?
What can chronic untreated Hydronephrosis lead to?
What can chronic untreated Hydronephrosis lead to?
Which type of calculi is primarily composed of uric acid?
Which type of calculi is primarily composed of uric acid?
Which symptom is commonly associated with Nephrolithiasis?
Which symptom is commonly associated with Nephrolithiasis?
Nephrocalcinosis refers to ___.
Nephrocalcinosis refers to ___.
Which condition is NOT a cause of intrinsic Hydronephrosis?
Which condition is NOT a cause of intrinsic Hydronephrosis?
What can spontaneous hematomas in the kidney result from?
What can spontaneous hematomas in the kidney result from?
What is often the first imaging choice for assessing renal trauma?
What is often the first imaging choice for assessing renal trauma?
Which of the following is NOT a type of nephrolithiasis?
Which of the following is NOT a type of nephrolithiasis?
What indicates postrenal failure in kidney sonography?
What indicates postrenal failure in kidney sonography?
Which of the following kidney conditions is irreversible?
Which of the following kidney conditions is irreversible?
What is the main symptom of Nephrolithiasis when severe?
What is the main symptom of Nephrolithiasis when severe?
What is the most common cause of renal disease leading to kidney transplantation?
What is the most common cause of renal disease leading to kidney transplantation?
What characterizes Grade III Hydronephrosis?
What characterizes Grade III Hydronephrosis?
How is Urolithiasis primarily diagnosed?
How is Urolithiasis primarily diagnosed?
What is a significant sonographic finding of acute transplant rejection?
What is a significant sonographic finding of acute transplant rejection?
What describes the typical waveform of a normal renal artery during diastole?
What describes the typical waveform of a normal renal artery during diastole?
What is a common complication of renal trauma?
What is a common complication of renal trauma?
Which finding suggests renal artery stenosis?
Which finding suggests renal artery stenosis?
What symptom is commonly associated with renal artery thrombosis?
What symptom is commonly associated with renal artery thrombosis?
What is a common complication seen in CKD patients receiving hemodialysis?
What is a common complication seen in CKD patients receiving hemodialysis?
Which of the following indicates transplant dysfunction based on the resistive index?
Which of the following indicates transplant dysfunction based on the resistive index?
What does a small, slow pulse characterize in renal evaluations?
What does a small, slow pulse characterize in renal evaluations?
What typically causes renal vein thrombosis?
What typically causes renal vein thrombosis?
What is the most common solid renal mass in adults?
What is the most common solid renal mass in adults?
Which sonographic finding is associated with renal artery thrombosis?
Which sonographic finding is associated with renal artery thrombosis?
What is a common treatment necessary for end-stage renal disease?
What is a common treatment necessary for end-stage renal disease?
What is the primary function of the urinary bladder?
What is the primary function of the urinary bladder?
What anatomical feature outlines the trigone region of the urinary bladder?
What anatomical feature outlines the trigone region of the urinary bladder?
Where are the ureters located in relation to the bladder?
Where are the ureters located in relation to the bladder?
What is the average length of the male urethra?
What is the average length of the male urethra?
What triggers the conscious desire to expel urine?
What triggers the conscious desire to expel urine?
What is one possible consequence of bladder catheterization?
What is one possible consequence of bladder catheterization?
What are the constriction points of the ureters?
What are the constriction points of the ureters?
What is the external urethral orifice in females characterized by?
What is the external urethral orifice in females characterized by?
What role do parasympathetic fibers play in micturition?
What role do parasympathetic fibers play in micturition?
What is the shape of the bladder when it is empty?
What is the shape of the bladder when it is empty?
Which part of the male urethra courses through the prostate?
Which part of the male urethra courses through the prostate?
What results in urinary incontinence?
What results in urinary incontinence?
What anatomical structure is anterior to the female urethra?
What anatomical structure is anterior to the female urethra?
How does the bladder's size and position change?
How does the bladder's size and position change?
What is the bladder's relationship to the umbilicus?
What is the bladder's relationship to the umbilicus?
Which of the following structures is described as the functional unit of the kidney?
Which of the following structures is described as the functional unit of the kidney?
What is the name of the fibrous sheath that encloses the kidney and adrenal gland?
What is the name of the fibrous sheath that encloses the kidney and adrenal gland?
Which of the following renal arteries is typically difficult to obtain an ideal spectral waveform due to its perpendicular orientation to the Doppler sound beam?
Which of the following renal arteries is typically difficult to obtain an ideal spectral waveform due to its perpendicular orientation to the Doppler sound beam?
What is the sonographic appearance of the renal medulla?
What is the sonographic appearance of the renal medulla?
What is the sonographic appearance of a junctional parenchymal defect?
What is the sonographic appearance of a junctional parenchymal defect?
Which of the following renal variations is characterized by prominent renal cortical parenchyma extending between two medullary pyramids?
Which of the following renal variations is characterized by prominent renal cortical parenchyma extending between two medullary pyramids?
Which of the following is NOT a physiological function of the kidneys?
Which of the following is NOT a physiological function of the kidneys?
Which of the following is considered a lab test used to evaluate renal function?
Which of the following is considered a lab test used to evaluate renal function?
What is the typical sonographic appearance of an extrarenal pelvis?
What is the typical sonographic appearance of an extrarenal pelvis?
Which of the following is considered a normal sonographic finding of the renal pelvis?
Which of the following is considered a normal sonographic finding of the renal pelvis?
Which of the following renal arteries is the first branch of the main renal arteries?
Which of the following renal arteries is the first branch of the main renal arteries?
Which of the following factors may influence the serum creatinine threshold levels?
Which of the following factors may influence the serum creatinine threshold levels?
What is the significance of visualizing the liver and spleen along with the kidneys during an ultrasound examination?
What is the significance of visualizing the liver and spleen along with the kidneys during an ultrasound examination?
Which of the following is NOT a factor that can cause increased serum BUN?
Which of the following is NOT a factor that can cause increased serum BUN?
Which of the following conditions is associated with a GFR < 15 mL/min?
Which of the following conditions is associated with a GFR < 15 mL/min?
Which of the following is a common scanning tip for visualizing the renal arteries and veins?
Which of the following is a common scanning tip for visualizing the renal arteries and veins?
Flashcards
Kidneys Anatomy
Kidneys Anatomy
Paired organs located retroperitoneally, producing urine.
Ureters Function
Ureters Function
Tubes that convey urine from kidneys to the bladder.
Urethra Purpose
Urethra Purpose
Drains urine from the bladder to the outside of the body.
Metanephros
Metanephros
Signup and view all the flashcards
Kidney Size
Kidney Size
Signup and view all the flashcards
Hilum Anatomy
Hilum Anatomy
Signup and view all the flashcards
Renal Cortex
Renal Cortex
Signup and view all the flashcards
Renal Medulla
Renal Medulla
Signup and view all the flashcards
Renal pelvis
Renal pelvis
Signup and view all the flashcards
Renal hilum
Renal hilum
Signup and view all the flashcards
Major calyces
Major calyces
Signup and view all the flashcards
Minor calyces
Minor calyces
Signup and view all the flashcards
Nephron
Nephron
Signup and view all the flashcards
Renal corpuscle
Renal corpuscle
Signup and view all the flashcards
Renal vasculture
Renal vasculture
Signup and view all the flashcards
Blood flow sequence
Blood flow sequence
Signup and view all the flashcards
Echogenicity
Echogenicity
Signup and view all the flashcards
Medullary pyramids
Medullary pyramids
Signup and view all the flashcards
Erythropoietin
Erythropoietin
Signup and view all the flashcards
Blood urea nitrogen (BUN)
Blood urea nitrogen (BUN)
Signup and view all the flashcards
Estimated Glomerular Filtration Rate (eGFR)
Estimated Glomerular Filtration Rate (eGFR)
Signup and view all the flashcards
Stages of CKD
Stages of CKD
Signup and view all the flashcards
Normal Renal Artery Flow
Normal Renal Artery Flow
Signup and view all the flashcards
Doppler Sample Volume
Doppler Sample Volume
Signup and view all the flashcards
Doppler Angle
Doppler Angle
Signup and view all the flashcards
Wall Filter Setting
Wall Filter Setting
Signup and view all the flashcards
Pulse Repetition Frequency (PRF)
Pulse Repetition Frequency (PRF)
Signup and view all the flashcards
Resistive Index (RI)
Resistive Index (RI)
Signup and view all the flashcards
RI Calculation
RI Calculation
Signup and view all the flashcards
Diastolic Flow Loss
Diastolic Flow Loss
Signup and view all the flashcards
Bilateral Renal Agenesis
Bilateral Renal Agenesis
Signup and view all the flashcards
Unilateral Renal Agenesis
Unilateral Renal Agenesis
Signup and view all the flashcards
VACTERL Syndrome
VACTERL Syndrome
Signup and view all the flashcards
Complete Duplex Kidney
Complete Duplex Kidney
Signup and view all the flashcards
Ectopic Kidney
Ectopic Kidney
Signup and view all the flashcards
Horseshoe Kidney
Horseshoe Kidney
Signup and view all the flashcards
Crossed Fused Renal Ectopia
Crossed Fused Renal Ectopia
Signup and view all the flashcards
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
Signup and view all the flashcards
Complications of ADPKD
Complications of ADPKD
Signup and view all the flashcards
Autosomal Recessive Polycystic Kidney Disease (ARPKD)
Autosomal Recessive Polycystic Kidney Disease (ARPKD)
Signup and view all the flashcards
Sonographic findings in ARPKD
Sonographic findings in ARPKD
Signup and view all the flashcards
Multicystic Dysplastic Kidneys (MCDK)
Multicystic Dysplastic Kidneys (MCDK)
Signup and view all the flashcards
Medullary Sponge Kidney
Medullary Sponge Kidney
Signup and view all the flashcards
Renal Cyst
Renal Cyst
Signup and view all the flashcards
Simple Renal Cyst Characteristics
Simple Renal Cyst Characteristics
Signup and view all the flashcards
Complex Renal Cyst
Complex Renal Cyst
Signup and view all the flashcards
Sonographic Features of Complex Cysts
Sonographic Features of Complex Cysts
Signup and view all the flashcards
Parapelvic Cyst
Parapelvic Cyst
Signup and view all the flashcards
Cysts in Liver and Pancreas with ADPKD
Cysts in Liver and Pancreas with ADPKD
Signup and view all the flashcards
Pulmonary hypoplasia in ARPKD
Pulmonary hypoplasia in ARPKD
Signup and view all the flashcards
Renal Calculi
Renal Calculi
Signup and view all the flashcards
Hypertension in ADPKD
Hypertension in ADPKD
Signup and view all the flashcards
Metastatic Renal Tumors
Metastatic Renal Tumors
Signup and view all the flashcards
Lymphoma in Kidneys
Lymphoma in Kidneys
Signup and view all the flashcards
Hypoechoic Masses
Hypoechoic Masses
Signup and view all the flashcards
Hydronephrosis
Hydronephrosis
Signup and view all the flashcards
Caliectasis
Caliectasis
Signup and view all the flashcards
Pelvicaliectasis
Pelvicaliectasis
Signup and view all the flashcards
Intrinsic Causes of Hydronephrosis
Intrinsic Causes of Hydronephrosis
Signup and view all the flashcards
Extrinsic Causes of Hydronephrosis
Extrinsic Causes of Hydronephrosis
Signup and view all the flashcards
Nephrolithiasis
Nephrolithiasis
Signup and view all the flashcards
Types of Calculi
Types of Calculi
Signup and view all the flashcards
Nephrocalcinosis
Nephrocalcinosis
Signup and view all the flashcards
Renal Trauma Types
Renal Trauma Types
Signup and view all the flashcards
Subcapsular Hematoma
Subcapsular Hematoma
Signup and view all the flashcards
Infarction in Kidneys
Infarction in Kidneys
Signup and view all the flashcards
Symptoms of Urolithiasis
Symptoms of Urolithiasis
Signup and view all the flashcards
Acquired Cystic Disease
Acquired Cystic Disease
Signup and view all the flashcards
Von Hippel-Lindau Disease
Von Hippel-Lindau Disease
Signup and view all the flashcards
Tuberous Sclerosis
Tuberous Sclerosis
Signup and view all the flashcards
Angiomyolipoma (AML)
Angiomyolipoma (AML)
Signup and view all the flashcards
Renal Cell Carcinoma (RCC)
Renal Cell Carcinoma (RCC)
Signup and view all the flashcards
Wilms Tumor
Wilms Tumor
Signup and view all the flashcards
Hematuria
Hematuria
Signup and view all the flashcards
Urothelial Carcinoma
Urothelial Carcinoma
Signup and view all the flashcards
Benign Neoplasms
Benign Neoplasms
Signup and view all the flashcards
Sonographer's Role
Sonographer's Role
Signup and view all the flashcards
Transitional Cell Carcinoma (TCC)
Transitional Cell Carcinoma (TCC)
Signup and view all the flashcards
Renal Oncocytoma
Renal Oncocytoma
Signup and view all the flashcards
Acquired renal cysts
Acquired renal cysts
Signup and view all the flashcards
Angiomyolipoma Appearance
Angiomyolipoma Appearance
Signup and view all the flashcards
Acute Tubular Necrosis
Acute Tubular Necrosis
Signup and view all the flashcards
Intrinsic Renal Failure
Intrinsic Renal Failure
Signup and view all the flashcards
Acute Kidney Injury (AKI)
Acute Kidney Injury (AKI)
Signup and view all the flashcards
Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD)
Signup and view all the flashcards
End-Stage Kidney Disease
End-Stage Kidney Disease
Signup and view all the flashcards
Renal Transplantation
Renal Transplantation
Signup and view all the flashcards
Hematoma
Hematoma
Signup and view all the flashcards
Parvus Tardus
Parvus Tardus
Signup and view all the flashcards
Renal Artery Stenosis
Renal Artery Stenosis
Signup and view all the flashcards
Renal Artery Thrombosis
Renal Artery Thrombosis
Signup and view all the flashcards
Renal Vein Thrombosis
Renal Vein Thrombosis
Signup and view all the flashcards
Renal Cell Carcinoma
Renal Cell Carcinoma
Signup and view all the flashcards
Wilm’s Tumor
Wilm’s Tumor
Signup and view all the flashcards
Mesoblastic Nephroma
Mesoblastic Nephroma
Signup and view all the flashcards
Lower Urinary Tract
Lower Urinary Tract
Signup and view all the flashcards
Urinary Bladder
Urinary Bladder
Signup and view all the flashcards
Bladder Anatomy
Bladder Anatomy
Signup and view all the flashcards
Rugae
Rugae
Signup and view all the flashcards
Trigone
Trigone
Signup and view all the flashcards
Ureters
Ureters
Signup and view all the flashcards
Male Urethra
Male Urethra
Signup and view all the flashcards
Female Urethra
Female Urethra
Signup and view all the flashcards
Micturition
Micturition
Signup and view all the flashcards
Incontinence
Incontinence
Signup and view all the flashcards
Retention
Retention
Signup and view all the flashcards
Catheterization
Catheterization
Signup and view all the flashcards
Urethral Orifice
Urethral Orifice
Signup and view all the flashcards
Detrusor Muscle
Detrusor Muscle
Signup and view all the flashcards
Acute Pyelonephritis
Acute Pyelonephritis
Signup and view all the flashcards
Emphysematous Pyelonephritis
Emphysematous Pyelonephritis
Signup and view all the flashcards
Chronic Pyelonephritis
Chronic Pyelonephritis
Signup and view all the flashcards
Renal Injury
Renal Injury
Signup and view all the flashcards
Prerenal Failure
Prerenal Failure
Signup and view all the flashcards
Postrenal Failure
Postrenal Failure
Signup and view all the flashcards
Pyonephrosis
Pyonephrosis
Signup and view all the flashcards
Xanthogranulomatous Pyelonephritis (XGP)
Xanthogranulomatous Pyelonephritis (XGP)
Signup and view all the flashcards
Renal Imaging
Renal Imaging
Signup and view all the flashcards
Fungal Infections
Fungal Infections
Signup and view all the flashcards
Ultrasound Findings in Pyelonephritis
Ultrasound Findings in Pyelonephritis
Signup and view all the flashcards
Study Notes
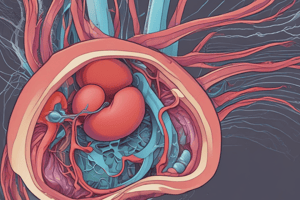
Kidney Anatomy and Physiology
- Paired kidneys lie in the retroperitoneum, against deep back muscles, lateral to the vertebrae.
- The right kidney is typically positioned slightly more inferior than the left.
- Kidneys produce urine.
- Paired ureters transport urine from the kidneys to the bladder.
- The urinary bladder stores urine.
- The urethra drains urine from the bladder to the body exterior.
Kidney Embryology
- Three pairs of kidneys form during development.
- Pronephros (fore kidney): Non-functional and disappears by the 4th week.
- Mesonephros (mid kidney): Partially functional in the first trimester (5th week). Gives rise to mesonephric tubules and ducts; Wolffian ducts in males (male genitalia); Mullerian ducts (paramesonephric ducts) in females (uterus, vagina)
- Metanephros (permanent kidney): Interaction of uretic buds and mesenchyme (blastema) forms the functioning kidney.
Kidney Size and Anatomy
-
Approximately the size of a clenched fist (9-12 cm long, 5-7 cm wide, 2-3 cm thick).
-
Kidneys should be within 2 cm of each other in length.
-
Layers :
- Fibrous renal capsule: Inner layer, smooth giving the kidney its shiny appearance
- Perirenal fat: Middle layer, adipose tissue, cushions and stabilizes
- Renal fascia/Gerota's fascia: Outer layer; dense fibrous tissue encompassing the kidney, fat, and adrenal gland
- Pararenal fat: Outermost (anterior and posterior); further stabilizes.
-
Hilum: The medial indentation where vessels and ureter enter/exit. The vein exits anteriorly, the artery enters between the vein and ureter, and the ureter exits posteriorly.
Kidney Relational Anatomy
-
Right Kidney:
- Superior-medial: Adrenal gland
- Superior-lateral: Liver
- Inferior: Right colic flexure
- Medial: 2nd portion of the duodenum
-
Left Kidney:
- Superior: Adrenal gland and spleen
- Anterior-superior: Pancreatic tail
- Inferior: Left colic flexure
Kidney Internal Anatomy
- Renal Cortex: Outer layer of kidney tissue.
- Renal Medulla: Inner layer of kidney tissue, with pyramids.
- Renal Sinus: Inner hyperechoic region containing fat, calyces, renal pelvis, vessels, and lymphatics.
- Medullary pyramids: Triangles of collecting tubules. Often seen in newborns and pediatrics.
- Renal Pelvis: Funnel-shaped structure collecting urine from major calyces, connecting to the ureter.
- Renal Hilum: The medial opening for entry/exit of the renal artery, vein, and ureter.
- Major Calyces: Extensions of the renal pelvis.
- Minor Calyces: Extensions of major calyces, collecting urine from medullary pyramids. Each minor calyx corresponds to a medullary pyramid.
- Renal Papilla: Tip of the medullary pyramid.
- Gerota's fascia: Fibrous sheath enclosing the kidney and adrenal gland (perirenal space).
- Nephron: Functional unit of the kidney, consisting of glomerulus, Bowman's capsule, tubules, and collecting ducts.
Renal Vasculature
- Kidneys receive blood through the renal artery branch of the aorta.
- At the hilum, the renal artery divides into segmental arteries.
- The segmental arteries divide into interlobar arteries, which run perpendicular to the renal capsule. These arteries travel between renal pyramids.
- Arcuate arteries branch from interlobar arteries at the base of the medullary pyramids and run parallel to the renal capsule.
- Interlobular arteries are the smallest renal arteries, branching off arcuate arteries and running perpendicular to the renal capsule.
Renal Blood Flow
- Main renal artery → segmental arteries → interlobar arteries → arcuate arteries → interlobular arteries.
Sonographic Appearance
- Renal Cortex: Isoechoic or hypoechoic relative to liver and spleen.
- Renal Medulla: Anechoic.
- Renal Sinus: Hyperechoic.
- Echo amplitude ascending order: Renal Medulla < Renal Cortex < Liver < Spleen < Pancreas < Diaphragm < Renal Sinus ≈ Renal Capsule
Anatomic Variants
- Junctional Parenchymal Defect: Triangular hyperechoic area anterior to upper pole of kidney (fetal lobulation).
- Hypertrophic Column of Bertin: Prominent cortical parenchyma extending between medullary pyramids.
- Extrarenal Pelvis: Renal pelvis lying outside the renal sinus.
- Dromedary Hump: A protuberance or bulge on the kidney's outer surface.
- Renal Sinus Lipomatosis: Excessive accumulation of fat in the renal sinus.
Kidney Function and Labs
- Function: Filters wastes, maintains water/electrolyte balance, releases hormones (renin for blood pressure, erythropoietin for RBC production, Vit D metabolism).
- Labs: Urea nitrogen, creatinine, uric acid evaluate renal function; RBC, WBC, bacteria indicate infection/tumors. Normal values vary by sex, age, region.
- eGFR: Essential for assessment after discovering albuminuria.
- CKD Stages: Normal: GFR >90 mL/min; End-stage: GFR <15 mL/min.
Doppler Evaluation
- Normal renal artery: Continuous forward flow during diastole (low resistance).
- Doppler Exam Techniques: Small sample volume (2-5 mm), <60-degree Doppler angle, low wall filter, smallest possible PRF.
- Resistive Index (RI): Used to assess renal disease, transplant rejection, suspected hydronephrosis. A normal RI is typically < 0.7. RI = (peak systolic velocity - end diastolic velocity) / peak systolic velocity.
Congenital Anomalies
- Agenesis/Hypoplasia: Absence or underdevelopment of one or both kidneys.
- Collecting System Duplication: Complete or incomplete duplication of the collecting system (two ureters).
- Ectopic Kidney: Kidney displaced from its normal position (pelvic, intrathoracic, crossed fused).
- Horseshoe Kidney: Fusion of the lower kidney poles across the midline.
Renal Diseases:
- ADPKD (Autosomal Dominant Polycystic Kidney Disease): Inherited, cysts in kidneys, liver, and potentially other organs.
- ARPKD (Autosomal Recessive Polycystic Kidney Disease): Present at birth, multiple small cysts, often with pulmonary hypoplasia and hepatic fibrosis.
- MCDK (Multicystic Dysplastic Kidney): Multiple non-communicating cysts, absence of renal parenchyma, most common cause of neonatal abdominal mass.
- Medullary Sponge Kidney: Cystic dilatation of medullary pyramids.
- Renal Cysts (Simple): Fluid-filled cysts, common in older adults.
- Renal Cysts (Complex/Atypical): Do not meet criteria of simple cysts, can be hemorrhagic, infected, multilocular, often require further investigation.
- Acquired Cystic Disease: Multiple cysts in chronically failed kidneys (dialysis patients).
- Renal Solid Masses: Benign (oncocytoma, angiomyolipoma, lipoma) or malignant (RCC).
- Wilms Tumor (Nephroblastoma): Most common childhood renal tumor.
- Urothelial Carcinoma: Malignant tumor of the urinary tract lining (Transitional Cell Carcinoma most common).
Kidney Obstruction and Infections:
- Congenital/Acquired obstruction - narrowing or blockage of the urinary tract (Ureteropelvic Junction Obstruction, Ureterocele)
- Hydronephrosis: Dilation of the renal collecting system due to urinary tract obstruction, can be graded (1-3).
- Urolithiasis (Renal Stones) : Calculi in the urinary system, often in kidneys. May be calcium, uric acid, or other types.
- Nephrocalcinosis: Calcium deposits within the renal parenchyma.
- Pyelonephritis (Acute/Chronic): Bacterial infection of the kidney, can result in pyonephrosis (pus in kidney). Xanthogranulomatous pyelonephritis is a chronic type.
- Renal Trauma: Blunt or penetrating trauma.
Renal Infarction and Injury:
- Renal Infarction: Blood supply obstruction to the kidney (e.g., arterial occlusion).
- Renal Injury/AKI: Acute kidney injury, impaired kidney function due to various causes (e.g., pre-renal, intrinsic, post-renal), characterized by reduced urine output, elevated BUN and creatinine.
- CKD/Chronic Renal Failure: Irreversible decline of kidney function over time.
- Renal Transplant evaluation: Transplant rejection or vascular complications are investigated.
###Lower Urinary Tract
Ureters, bladder and urethra are important part in transporting, storing and eliminating urine.
- Urinary Bladder anatomy and function*
- Ureters structure and function*
- Urethra structure and function (male/female)*
- Voiding Mechanism*
- Incontinence/Retention*
Parasympathetic and voluntary nervous system impulses control the bladder and urethra
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.