Podcast
Questions and Answers
Which of the following statements about the urinary system is TRUE?
Which of the following statements about the urinary system is TRUE?
- Excretion includes the contraction of smooth muscle to move urine along passageways and transport urine outside the body. (correct)
- Nephrons are responsible for fluid balance and elimination, but not excretion.
- Small, organic compounds are filtered by the renal corpuscle, except glucose, which is mostly secreted.
- During secretion, wastes move from the blood, into the interstitial space, then into the tubular fluid. (correct)
- The arteries and veins that reach the glomeruli enter at the kidney by penetrating the outer fibrous capsule. (correct)
Which of the following scenarios is TRUE? Since the podocytes prevent the excretion of larger organic compounds (like blood cells and large proteins), but still allow smaller organic compounds and ions through.
Which of the following scenarios is TRUE? Since the podocytes prevent the excretion of larger organic compounds (like blood cells and large proteins), but still allow smaller organic compounds and ions through.
- Ion concentrations in the filtrate and plasma are isotonic.
- Colloid pressure depends on ion concentrations, causing water to remain in the blood.
- Glucose and amino acids are more concentrated in the filtrate than in the blood.
- Glucose and amino acids are more concentrated in the blood than in the filtrate. (correct)
Which of the following statements is TRUE about filtration? The filtration of substances out of the blood and into the glomerular capsule is directed and coordinated by difference in glomerular hydrostatic pressure.
Which of the following statements is TRUE about filtration? The filtration of substances out of the blood and into the glomerular capsule is directed and coordinated by difference in glomerular hydrostatic pressure.
- Arterial pressure affects GHP, but the afferent and efferent arterioles can dilate or constrict to mitigate major changes in GFR. (correct)
- Dilating the efferent arterioles and constricting the afferent arteriole will increase GHP.
- A drop in blood pressure would result in a lower OP, ultimately decreasing the net filtration rate.
- OP increases when the concentration of plasma proteins is decreased.
What is the most accurate measurement of GFR?
What is the most accurate measurement of GFR?
What is the common indicator of renal failure?
What is the common indicator of renal failure?
Which of the following is NOT a type of acute renal failure?
Which of the following is NOT a type of acute renal failure?
Chronic kidney disease is often associated with permanent damage to the nephrons.
Chronic kidney disease is often associated with permanent damage to the nephrons.
The most common risk factors for chronic kidney disease are diabetes and hypertension
The most common risk factors for chronic kidney disease are diabetes and hypertension
Life-supporting treatments for kidney failure include dialysis and kidney transplantation.
Life-supporting treatments for kidney failure include dialysis and kidney transplantation.
Creatinine clearance is more accurate than inulin clearance for measuring GFR
Creatinine clearance is more accurate than inulin clearance for measuring GFR
The urinary system has three important functions: excretion, homeostatic regulation, and elimination. Which of the following statements about the urinary system is TRUE?
The urinary system has three important functions: excretion, homeostatic regulation, and elimination. Which of the following statements about the urinary system is TRUE?
Nephrons are the basic functional units of the kidneys. Their proper functioning is crucial to the maintenance of homeostasis. Since the podocytes prevent the excretion of larger organic compounds (like blood cells and large proteins), but still allow smaller organic compounds and ions through, which of the following scenarios is TRUE?
Nephrons are the basic functional units of the kidneys. Their proper functioning is crucial to the maintenance of homeostasis. Since the podocytes prevent the excretion of larger organic compounds (like blood cells and large proteins), but still allow smaller organic compounds and ions through, which of the following scenarios is TRUE?
The filtration of substances out of the blood and into the glomerular capsule is directed and coordinated by differences in glomerular hydrostatic pressure. Which of the following statements is TRUE about filtration? (GHP = glomerular hydrostatic pressure, CP = colloid pressure, GFR = glomerular filtration rate).
The filtration of substances out of the blood and into the glomerular capsule is directed and coordinated by differences in glomerular hydrostatic pressure. Which of the following statements is TRUE about filtration? (GHP = glomerular hydrostatic pressure, CP = colloid pressure, GFR = glomerular filtration rate).
What is the main function of the kidney?
What is the main function of the kidney?
What is the name of the functional unit of the kidney?
What is the name of the functional unit of the kidney?
What is the difference between acute and chronic kidney failure?
What is the difference between acute and chronic kidney failure?
What is Glomerular Filtration Rate (GFR) and what does it indicate?
What is Glomerular Filtration Rate (GFR) and what does it indicate?
Kidney disease is always a result of diabetes or hypertension.
Kidney disease is always a result of diabetes or hypertension.
End-stage kidney disease requires life-supporting treatments.
End-stage kidney disease requires life-supporting treatments.
Flashcards
Kidney Function
Kidney Function
Excretion, elimination, and homeostatic regulation of fluids and electrolytes in the body.
Excretion
Excretion
Filtering solutes from blood into tubular fluid, primarily nitrogenous wastes.
Elimination
Elimination
Transporting urine outside the body.
Homeostatic Regulation
Homeostatic Regulation
Signup and view all the flashcards
Nephron
Nephron
Signup and view all the flashcards
Glomerular Filtration
Glomerular Filtration
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
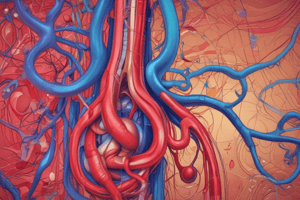
Afferent Arteriole
Afferent Arteriole
Signup and view all the flashcards
Efferent Arteriole
Efferent Arteriole
Signup and view all the flashcards
Peritubular Capillaries
Peritubular Capillaries
Signup and view all the flashcards
Renal Failure
Renal Failure
Signup and view all the flashcards
Acute Renal Failure
Acute Renal Failure
Signup and view all the flashcards
Chronic Renal Failure
Chronic Renal Failure
Signup and view all the flashcards
Azotemia
Azotemia
Signup and view all the flashcards
Creatinine Clearance
Creatinine Clearance
Signup and view all the flashcards
Inulin Clearance
Inulin Clearance
Signup and view all the flashcards
Proximal Convoluted Tubule (PCT)
Proximal Convoluted Tubule (PCT)
Signup and view all the flashcards
Nephron Loop
Nephron Loop
Signup and view all the flashcards
Distal Convoluted Tubule (DCT)
Distal Convoluted Tubule (DCT)
Signup and view all the flashcards
Collecting Duct
Collecting Duct
Signup and view all the flashcards
Glomerular Hydrostatic Pressure
Glomerular Hydrostatic Pressure
Signup and view all the flashcards
Colloid Pressure
Colloid Pressure
Signup and view all the flashcards
Kidney's Main Jobs
Kidney's Main Jobs
Signup and view all the flashcards
Blood Flow Through Kidney
Blood Flow Through Kidney
Signup and view all the flashcards
Afferent vs. Efferent Arteriole
Afferent vs. Efferent Arteriole
Signup and view all the flashcards
What's NOT Filtered?
What's NOT Filtered?
Signup and view all the flashcards
Reabsorption
Reabsorption
Signup and view all the flashcards
Homeostatic Regulation in Nephron
Homeostatic Regulation in Nephron
Signup and view all the flashcards
GFR Measurement
GFR Measurement
Signup and view all the flashcards
Why Inulin is Best
Why Inulin is Best
Signup and view all the flashcards
Prerenal vs. Intrinsic Failure
Prerenal vs. Intrinsic Failure
Signup and view all the flashcards
Postrenal Failure
Postrenal Failure
Signup and view all the flashcards
Stages of Chronic Kidney Disease (CKD)
Stages of Chronic Kidney Disease (CKD)
Signup and view all the flashcards
Proximal Convoluted Tubule (PCT) Role
Proximal Convoluted Tubule (PCT) Role
Signup and view all the flashcards
Nephron Loop Function
Nephron Loop Function
Signup and view all the flashcards
Distal Convoluted Tubule (DCT) Adjustments
Distal Convoluted Tubule (DCT) Adjustments
Signup and view all the flashcards
Collecting Duct's Role
Collecting Duct's Role
Signup and view all the flashcards
Hormonal Influence on Kidney
Hormonal Influence on Kidney
Signup and view all the flashcards
Kidney's Endocrine Role
Kidney's Endocrine Role
Signup and view all the flashcards
Elimination: Urine's Journey
Elimination: Urine's Journey
Signup and view all the flashcards
Study Notes
Kidney Anatomy and Function
- Kidneys perform excretion, elimination, and homeostatic regulation
- Blood is circulated through the kidney, filtered by nephrons, and substances reabsorbed/secreted to maintain solute and water balance.
- Kidneys receive 20-25% of cardiac output for oxygen and nutrient delivery.
- Blood flows through renal arteries, segmental arteries, interlobar arteries, arcuate arteries, cortical radiate arteries, and afferent arterioles to enter glomerular capillaries.
- Waste- and nutrient-poor blood, now oxygenated, flows through peritubular capillaries to nourish nephrons.
- Deoxygenated blood exits via venules and veins
Blood Flow Through the Kidney
- Blood enters the kidney via renal arteries
- Branches into segmental, interlobar, arcuate, cortical radiate arteries, and then afferent arterioles.
- Blood enters the glomerulus (a capillary network) where filtration occurs.
- Blood leaves the glomerulus through efferent arterioles.
- Blood then flows through the peritubular capillaries and is returned to the heart through venules and veins
- Waste products and excess solutes are removed from the blood in nephrons
Nephron Function
- The nephron is the basic functional unit of the kidney.
- Excretion: Filters solutes from blood into tubular fluid (across glomeruli). This includes nitrogenous wastes (urea, creatinine, ammonia, uric acid).
- Homeostatic regulation: reabsorbs useful substances (glucose, amino acids, electrolytes) and secretes excess substances.
- Kidneys regulate levels of sodium, potassium, hydrogen, and bicarbonate ions.
- Water, often following solute concentrations, also adjusted
- Elimination: Urine is transported out of the body.
- Filtration is a key process: substances move from blood into glomerular capsule, driven by glomerular hydrostatic pressure
Glomerular Filtration Rate (GFR)
- GFR: is a measure of kidney function.
- A normal GFR is between 100 and 130 ml/min/1.73m2
- GFR is determined by the volume of serum filtered per minute.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.