Podcast
Questions and Answers
How does a keloid scar differ from a normal linear scar in terms of growth pattern?
How does a keloid scar differ from a normal linear scar in terms of growth pattern?
- Linear scars exhibit significant growth and thickening over time, while keloid scars remain relatively stable.
- Both keloid and linear scars demonstrate similar growth patterns, with neither extending beyond the original wound.
- Keloid scars remain confined to the original wound area, while linear scars spread beyond it.
- Keloid scars grow beyond the boundaries of the original wound, while linear scars stay within it. (correct)
Which characteristic is most indicative of a hypertrophic scar (keloid) compared to a normal healing scar?
Which characteristic is most indicative of a hypertrophic scar (keloid) compared to a normal healing scar?
- A significant elevation above the surrounding skin and irregular shape. (correct)
- A lighter pigmentation compared to surrounding skin.
- A flat, smooth surface that blends with the skin.
- A shrinking size over time.
What visual cue primarily distinguishes a keloid from a typical scar?
What visual cue primarily distinguishes a keloid from a typical scar?
- A keloid appears as a sunken area, while a typical scar is raised.
- A keloid has a pale, almost translucent appearance, unlike a typical scar.
- A keloid extends beyond the initial wound site, unlike a typical scar. (correct)
- A keloid is characterized by a perfectly smooth and even surface, unlike a typical scar.
What does the term 'overgrown scar' specifically refer to in the context of scar formation?
What does the term 'overgrown scar' specifically refer to in the context of scar formation?
Considering the visual characteristics of keloid scars, which description most accurately represents their typical appearance in the early stages of formation?
Considering the visual characteristics of keloid scars, which description most accurately represents their typical appearance in the early stages of formation?
Which of the following complications of fibrosis would most directly lead to difficulty in swallowing?
Which of the following complications of fibrosis would most directly lead to difficulty in swallowing?
A patient with advanced liver cirrhosis develops intestinal obstruction. Which complication of fibrosis is MOST likely the cause?
A patient with advanced liver cirrhosis develops intestinal obstruction. Which complication of fibrosis is MOST likely the cause?
A 25-year-old patient presents with a surgical wound. Which factor would MOST effectively promote optimal healing?
A 25-year-old patient presents with a surgical wound. Which factor would MOST effectively promote optimal healing?
An elderly patient with a history of diabetes and peripheral vascular disease has a leg ulcer. Which of these factors would MOST significantly delay the healing process?
An elderly patient with a history of diabetes and peripheral vascular disease has a leg ulcer. Which of these factors would MOST significantly delay the healing process?
A patient develops limited range of motion in their elbow following a burn injury. Which of the listed complications of fibrosis is MOST likely responsible for this?
A patient develops limited range of motion in their elbow following a burn injury. Which of the listed complications of fibrosis is MOST likely responsible for this?
A patient undergoing chemotherapy for cancer treatment develops a skin wound. How does chemotherapy MOST likely affect the healing process?
A patient undergoing chemotherapy for cancer treatment develops a skin wound. How does chemotherapy MOST likely affect the healing process?
How do collagen fibers contribute to the development of contractures in fibrotic tissue?
How do collagen fibers contribute to the development of contractures in fibrotic tissue?
Which of the following is the BEST description of stenosis as a complication of fibrosis?
Which of the following is the BEST description of stenosis as a complication of fibrosis?
Which of the following conditions would have the MOST POSITIVE impact on wound healing?
Which of the following conditions would have the MOST POSITIVE impact on wound healing?
A patient taking glucocorticoids for a chronic inflammatory condition sustains a minor injury. How do glucocorticoids affect wound healing?
A patient taking glucocorticoids for a chronic inflammatory condition sustains a minor injury. How do glucocorticoids affect wound healing?
Following an injury, which process results in the complete restoration of both structure and function in the affected tissue?
Following an injury, which process results in the complete restoration of both structure and function in the affected tissue?
Under what circumstances does fibrosis typically occur during the healing process?
Under what circumstances does fibrosis typically occur during the healing process?
Which of the following processes involves the replacement of dead cells with new cells of the same type?
Which of the following processes involves the replacement of dead cells with new cells of the same type?
In a scenario where a minor skin abrasion heals completely without any scarring, which healing process is most likely responsible?
In a scenario where a minor skin abrasion heals completely without any scarring, which healing process is most likely responsible?
Why is the formation of a blood clot essential at the beginning of the healing process?
Why is the formation of a blood clot essential at the beginning of the healing process?
Which of the following best describes the role of macrophages during the second stage of wound healing by both first and second intention?
Which of the following best describes the role of macrophages during the second stage of wound healing by both first and second intention?
In wound healing by first intention, what is the primary mechanism that leads to the closure of the wound?
In wound healing by first intention, what is the primary mechanism that leads to the closure of the wound?
How does the role of new capillaries forming relate to wound healing?
How does the role of new capillaries forming relate to wound healing?
Which of the following is a key difference between healing by first intention and healing by second intention?
Which of the following is a key difference between healing by first intention and healing by second intention?
What is the primary purpose of scab formation in both first and second intention wound healing?
What is the primary purpose of scab formation in both first and second intention wound healing?
Which process is most directly associated with the action of fibroblasts during the granulation tissue stage?
Which process is most directly associated with the action of fibroblasts during the granulation tissue stage?
What role do neutrophils play in the initial stage of both first and second intention wound healing?
What role do neutrophils play in the initial stage of both first and second intention wound healing?
How does contraction of fibrous tissue aid in the healing process?
How does contraction of fibrous tissue aid in the healing process?
A patient with a history of gastritis requires an analgesic. Which of the following medications would be LEAST suitable, considering their potential to exacerbate the patient's condition?
A patient with a history of gastritis requires an analgesic. Which of the following medications would be LEAST suitable, considering their potential to exacerbate the patient's condition?
A patient experiencing both inflammation and pain needs a medication that addresses both symptoms but also minimizes the risk of delayed blood clotting. Which medication should be avoided?
A patient experiencing both inflammation and pain needs a medication that addresses both symptoms but also minimizes the risk of delayed blood clotting. Which medication should be avoided?
Which medication used to treat inflammation is LEAST likely to provide pain relief?
Which medication used to treat inflammation is LEAST likely to provide pain relief?
A patient with a known hypersensitivity to aspirin needs an antipyretic medication. Which of the following would be the MOST appropriate and safe choice?
A patient with a known hypersensitivity to aspirin needs an antipyretic medication. Which of the following would be the MOST appropriate and safe choice?
A patient presents symptoms of inflammation, pain, and fever, but has a high risk of cardiovascular events. Considering the adverse effect profiles, which of the following medications should be administered with the MOST caution?
A patient presents symptoms of inflammation, pain, and fever, but has a high risk of cardiovascular events. Considering the adverse effect profiles, which of the following medications should be administered with the MOST caution?
Following a minor cut, a patient experiences redness and warmth around the wound. Which of the following mechanisms BEST explains these early signs of acute inflammation?
Following a minor cut, a patient experiences redness and warmth around the wound. Which of the following mechanisms BEST explains these early signs of acute inflammation?
How does the cellular composition of chronic inflammation differ from that of acute inflammation?
How does the cellular composition of chronic inflammation differ from that of acute inflammation?
A patient presents with persistent joint pain and swelling lasting several months. Which of the following processes is MOST likely contributing to the patient's chronic inflammation?
A patient presents with persistent joint pain and swelling lasting several months. Which of the following processes is MOST likely contributing to the patient's chronic inflammation?
What is the primary reason for increased fibrosis (scarring) in chronic inflammation compared to acute inflammation?
What is the primary reason for increased fibrosis (scarring) in chronic inflammation compared to acute inflammation?
A patient who has undergone surgery is experiencing significant pain around the incision site. How does the inflammatory process contribute MOST directly to this sensation of pain?
A patient who has undergone surgery is experiencing significant pain around the incision site. How does the inflammatory process contribute MOST directly to this sensation of pain?
After suffering a superficial skin abrasion, the damaged tissue is fully restored with the same cell type. Which healing process is MOST accurately described in this scenario?
After suffering a superficial skin abrasion, the damaged tissue is fully restored with the same cell type. Which healing process is MOST accurately described in this scenario?
Why does chronic inflammation typically result in greater tissue destruction compared to acute inflammation?
Why does chronic inflammation typically result in greater tissue destruction compared to acute inflammation?
How does the presence of granulomas contribute to the characteristics of chronic inflammation?
How does the presence of granulomas contribute to the characteristics of chronic inflammation?
A patient sustains a deep wound to their arm. If the healing process results in the formation of scar tissue, which component of the inflammatory response was MOST likely insufficient to restore the original tissue structure and function?
A patient sustains a deep wound to their arm. If the healing process results in the formation of scar tissue, which component of the inflammatory response was MOST likely insufficient to restore the original tissue structure and function?
A biopsy of a tissue sample reveals a significant presence of lymphocytes, macrophages, and fibroblasts. Which type of inflammatory response is MOST likely occurring in this tissue?
A biopsy of a tissue sample reveals a significant presence of lymphocytes, macrophages, and fibroblasts. Which type of inflammatory response is MOST likely occurring in this tissue?
During an inflammatory response, how does the alteration in plasma protein levels, specifically increased fibrinogen, contribute to the elevated ESR (erythrocyte sedimentation rate)?
During an inflammatory response, how does the alteration in plasma protein levels, specifically increased fibrinogen, contribute to the elevated ESR (erythrocyte sedimentation rate)?
Following a myocardial infarction (heart attack), which blood test result would be MOST indicative of cardiac tissue damage, based on the changes observed in blood during inflammation?
Following a myocardial infarction (heart attack), which blood test result would be MOST indicative of cardiac tissue damage, based on the changes observed in blood during inflammation?
A patient presents with symptoms of systemic inflammation. While awaiting specific diagnostic results, which initial blood test would provide the MOST general indication of an inflammatory process?
A patient presents with symptoms of systemic inflammation. While awaiting specific diagnostic results, which initial blood test would provide the MOST general indication of an inflammatory process?
How does leukocytosis, characterized by an increase in white blood cells, primarily aid in the body's response to inflammation?
How does leukocytosis, characterized by an increase in white blood cells, primarily aid in the body's response to inflammation?
In a patient experiencing chronic inflammation, why might monitoring C-reactive protein (CRP) levels be more useful than monitoring cell enzyme levels for assessing disease activity?
In a patient experiencing chronic inflammation, why might monitoring C-reactive protein (CRP) levels be more useful than monitoring cell enzyme levels for assessing disease activity?
During the process of wound healing, granulation tissue serves to directly replace which of the following?
During the process of wound healing, granulation tissue serves to directly replace which of the following?
The high vascularity of granulation tissue, resulting from angiogenesis, is most directly important for which aspect of wound healing?
The high vascularity of granulation tissue, resulting from angiogenesis, is most directly important for which aspect of wound healing?
Fibroblasts play a critical role in scar formation by performing which of the following actions?
Fibroblasts play a critical role in scar formation by performing which of the following actions?
Compared to normal tissue, scar tissue is characterized by which of the following properties?
Compared to normal tissue, scar tissue is characterized by which of the following properties?
Which of the following best describes the inherent fragility of granulation tissue in the context of wound healing?
Which of the following best describes the inherent fragility of granulation tissue in the context of wound healing?
Flashcards
Hypertrophic Scar
Hypertrophic Scar
A raised scar that remains within the original wound boundaries.
Keloid
Keloid
A type of scar that is raised and extends beyond the original wound area.
Linear Scar
Linear Scar
A thin, raised scar that follows a straight line pattern.
Scar Characteristics
Scar Characteristics
Signup and view all the flashcards
Overgrown Scars
Overgrown Scars
Signup and view all the flashcards
Esophageal Scarring
Esophageal Scarring
Signup and view all the flashcards
Adhesions
Adhesions
Signup and view all the flashcards
Contractures
Contractures
Signup and view all the flashcards
Stenosis
Stenosis
Signup and view all the flashcards
Granulation Tissue
Granulation Tissue
Signup and view all the flashcards
Vascular Nature of Granulation Tissue
Vascular Nature of Granulation Tissue
Signup and view all the flashcards
Fibroblasts
Fibroblasts
Signup and view all the flashcards
Collagen
Collagen
Signup and view all the flashcards
Scar Tissue Function
Scar Tissue Function
Signup and view all the flashcards
Factors promoting healing
Factors promoting healing
Signup and view all the flashcards
Youth
Youth
Signup and view all the flashcards
Nutrition's Role
Nutrition's Role
Signup and view all the flashcards
Factors delaying healing
Factors delaying healing
Signup and view all the flashcards
Infection's Impact
Infection's Impact
Signup and view all the flashcards
Healing Process
Healing Process
Signup and view all the flashcards
Resolution
Resolution
Signup and view all the flashcards
Regeneration
Regeneration
Signup and view all the flashcards
Fibrosis
Fibrosis
Signup and view all the flashcards
Scar Formation
Scar Formation
Signup and view all the flashcards
Injury and Inflammation
Injury and Inflammation
Signup and view all the flashcards
Epithelial Regeneration
Epithelial Regeneration
Signup and view all the flashcards
First Intention Healing
First Intention Healing
Signup and view all the flashcards
Second Intention Healing
Second Intention Healing
Signup and view all the flashcards
Scar Contraction
Scar Contraction
Signup and view all the flashcards
Acute Inflammation
Acute Inflammation
Signup and view all the flashcards
Chemical Mediators
Chemical Mediators
Signup and view all the flashcards
Phagocytosis
Phagocytosis
Signup and view all the flashcards
Chronic Inflammation
Chronic Inflammation
Signup and view all the flashcards
Collagen Production
Collagen Production
Signup and view all the flashcards
Granulomas
Granulomas
Signup and view all the flashcards
White Blood Cell Types
White Blood Cell Types
Signup and view all the flashcards
Tissue Destruction
Tissue Destruction
Signup and view all the flashcards
Anti-inflammatory drugs
Anti-inflammatory drugs
Signup and view all the flashcards
Analgesic drugs
Analgesic drugs
Signup and view all the flashcards
Antipyretic drugs
Antipyretic drugs
Signup and view all the flashcards
NSAIDs
NSAIDs
Signup and view all the flashcards
Glucocorticoids
Glucocorticoids
Signup and view all the flashcards
Leukocytosis
Leukocytosis
Signup and view all the flashcards
C-reactive protein (CRP)
C-reactive protein (CRP)
Signup and view all the flashcards
Differential count
Differential count
Signup and view all the flashcards
Increased ESR
Increased ESR
Signup and view all the flashcards
Cell enzymes
Cell enzymes
Signup and view all the flashcards
Study Notes
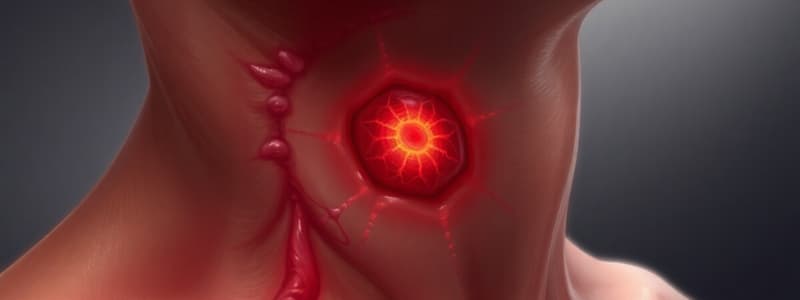
Hypertrophic Scar (Keloid)
- Image A shows a linear scar, Image B shows a raised, hypertrophic scar.
- Hypertrophic scars are raised but do not extend past the original wound boundaries.
- Keloids are raised scars that extend beyond the original wound boundaries.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.