Podcast
Questions and Answers
What is the normal range for Right Atrial Pressure (RAP)?
What is the normal range for Right Atrial Pressure (RAP)?
- 15-25 cm (correct)
- 20-30 cm
- 10-20 cm
- 30-40 cm
During a left thoracotomy with OLV, where would the catheter tip most likely be?
During a left thoracotomy with OLV, where would the catheter tip most likely be?
- In the main pulmonary artery
- In the right atrium
- In the dependent lung (correct)
- In the non-dependent lung
What is the upper safety limit for Pulmonary Artery Pressure (PAP) during a right thoracotomy?
What is the upper safety limit for Pulmonary Artery Pressure (PAP) during a right thoracotomy?
- 30 mmHg
- 33 mmHg (correct)
- 25 mmHg
- 40 mmHg
What does SvO2 reflect?
What does SvO2 reflect?
What is the significance of an abnormal CVP/PA waveform?
What is the significance of an abnormal CVP/PA waveform?
What is the distance from the Right Internal Jugular (RIJ) vein to the Pulmonary Artery?
What is the distance from the Right Internal Jugular (RIJ) vein to the Pulmonary Artery?
What is the main advantage of using oximetry principles in SvO2 measurement?
What is the main advantage of using oximetry principles in SvO2 measurement?
Why may SvO2 not be an accurate indicator of ischemia in a specific organ?
Why may SvO2 not be an accurate indicator of ischemia in a specific organ?
What is the significance of the Dicrotic notch in the Pulmonary Artery Pressure waveform?
What is the significance of the Dicrotic notch in the Pulmonary Artery Pressure waveform?
What is the purpose of Intraoperative Monitoring using a Pulmonary Artery Catheter?
What is the purpose of Intraoperative Monitoring using a Pulmonary Artery Catheter?
Flashcards are hidden until you start studying
Study Notes
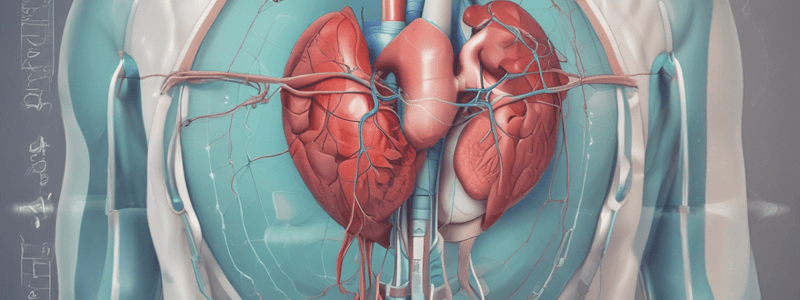
Invasive Cardiac Monitoring
- Pulmonary Artery (PA) Catheter: measures cardiac output (CO) by thermodilution; valuable post-op when Transesophageal Echocardiography (TEE) not available; can also measure mixed venous saturation
- Contraindications: complete heart block (CHB), pacemaker in last 6 weeks, knotting or entanglement with chordae tendinae
- Complications: distal ischemia, pseudoaneurysm, arteriovenous fistula, hemorrhage, arterial embolization, infection, peripheral neuropathy, misinterpretation of data, misuse of equipment
Cardiac Output
- Thermodilution: change in temperature sensed by thermistor in PA catheter
- Continuous Cardiac Output: blood randomly heated and change in temperature measured
- Arterial Pressure Cardiac Output: CO measured from arterial line; good correlation with standard methods
Arterial Pressure Monitoring
- Indications: continuous real-time blood pressure monitoring, anticipated pharmacologic or mechanical cardiovascular manipulation, repeated blood sampling, failure of indirect arterial blood pressure measurement, supplementary diagnostic information from arterial waveform
- Complications: distal ischemia, pseudoaneurysm, arteriovenous fistula, hemorrhage, arterial embolization, infection, peripheral neuropathy, misinterpretation of data, misuse of equipment
- Interpretation: arterial waveform components include upstroke, systolic peak, gradual downslope, dicrotic notch
Invasive Arterial Pressure Monitoring
- Indications: continuous real-time blood pressure monitoring, anticipated pharmacologic or mechanical cardiovascular manipulation, repeated blood sampling, failure of indirect arterial blood pressure measurement, supplementary diagnostic information from arterial waveform
- Contraindications: relative (atherosclerosis, severe peripheral vasoconstriction, compromised collateral circulation, Reynaud's disease, Buerger's disease); absolute (infection, severe bleeding, and vascular injury)
- Complications: infection, ischemia, skin necrosis, bleeding, arteriovenous fistulas
- Techniques: direct cannulation, transfixation, Seldinger
- Locations: radial artery, ulnar artery, brachial artery, axillary artery, femoral artery, dorsalis pedis artery
Central Venous Monitoring
- Indications: central venous pressure monitoring, pulmonary artery catheterization and monitoring, transvenous cardiac pacing, temporary hemodialysis, drug administration, rapid infusion of fluids, aspiration of air emboli, inadequate peripheral intravenous access, sampling site for repeated blood testing
- Contraindications: thrombosed veins, LBBB, infection at insertion site, cardiac mass, coagulopathies
- Complications: mechanical (vascular injury, respiratory compromise, nerve injury, arrhythmias), infectious (insertion site infection, catheter infection, bloodstream infection, endocarditis), thromboembolic (venous thrombosis, pulmonary embolism, arterial thrombosis and embolism, catheter or guidewire embolism)
- Locations: internal jugular vein, subclavian vein, external jugular vein (last resort)
- Techniques: Seldinger technique, landmarks, ultrasound guided
Pulmonary Artery Catheters
- Complications: arrhythmias, complete heart block, endobronchial hemorrhage, pulmonary infarction, catheter knotting, valve damage
- Contraindications: similar to those for central line
- Advancement: with a change in waveform could indicate distance from the RT internal jugular vein to distal cardiac and pulmonary structures
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.