Podcast
Questions and Answers
Which characteristic distinguishes gametes from other body cells?
Which characteristic distinguishes gametes from other body cells?
- Gametes are involved in maintaining body organs.
- Gametes do not require a body system to survive.
- Gametes produce hormones affecting the immune system.
- Gametes directly contribute to the development of offspring. (correct)
What is the primary role of the testes in the male reproductive system?
What is the primary role of the testes in the male reproductive system?
- Producing sperm and hormones. (correct)
- Delivering sperm to the female.
- Protecting and regulating the temperature of sperm.
- Nourishing and transporting sperm cells.
How do interstitial cells support male reproductive function?
How do interstitial cells support male reproductive function?
- By producing male sex hormones (correct)
- By transporting sperm to the epididymis
- By providing structural support to seminiferous tubules
- By regulating the temperature of the testes
What is the role of the epididymis in the male reproductive system?
What is the role of the epididymis in the male reproductive system?
What is the combined function of fructose and prostaglandins in semen?
What is the combined function of fructose and prostaglandins in semen?
Which structural adaptation of the scrotum supports sperm production?
Which structural adaptation of the scrotum supports sperm production?
How does nitric oxide (NO) facilitate an erection?
How does nitric oxide (NO) facilitate an erection?
What event occurs during emission in the male reproductive process?
What event occurs during emission in the male reproductive process?
Which cells directly result from the first meiotic division during spermatogenesis?
Which cells directly result from the first meiotic division during spermatogenesis?
What is the function of the acrosome in a mature sperm cell?
What is the function of the acrosome in a mature sperm cell?
How does inhibin regulate male reproductive function?
How does inhibin regulate male reproductive function?
Which of the following is a direct action of testosterone?
Which of the following is a direct action of testosterone?
What occurs when blood testosterone concentration increases?
What occurs when blood testosterone concentration increases?
What is the essential role of the ovaries in the female reproductive system?
What is the essential role of the ovaries in the female reproductive system?
How do fimbriae facilitate fertilization?
How do fimbriae facilitate fertilization?
Which layer of the uterus is responsible for the cyclical changes during the menstrual cycle?
Which layer of the uterus is responsible for the cyclical changes during the menstrual cycle?
What is the primary structural function of the labia majora?
What is the primary structural function of the labia majora?
How does nitric oxide (NO) contribute to female sexual function?
How does nitric oxide (NO) contribute to female sexual function?
What event signifies the completion of meiosis II in oogenesis?
What event signifies the completion of meiosis II in oogenesis?
During follicle maturation, what role do granulosa cells play?
During follicle maturation, what role do granulosa cells play?
What hormonal change triggers ovulation?
What hormonal change triggers ovulation?
How do estrogens influence the uterine lining during the menstrual cycle?
How do estrogens influence the uterine lining during the menstrual cycle?
What occurs in the absence of fertilization during the menstrual cycle?
What occurs in the absence of fertilization during the menstrual cycle?
Which change signifies the beginning of menopause?
Which change signifies the beginning of menopause?
What distinguishes a lactiferous duct from other structures in the mammary glands?
What distinguishes a lactiferous duct from other structures in the mammary glands?
Which birth control method relies on preventing sperm from entering the vagina?
Which birth control method relies on preventing sperm from entering the vagina?
How do combined hormone contraceptives prevent pregnancy?
How do combined hormone contraceptives prevent pregnancy?
What is the mechanism of action for intrauterine devices (IUDs) in preventing pregnancy?
What is the mechanism of action for intrauterine devices (IUDs) in preventing pregnancy?
Which of the following STIs is associated with the symptom of painful urination and intercourse, along with a mucous discharge?
Which of the following STIs is associated with the symptom of painful urination and intercourse, along with a mucous discharge?
A patient presents with fever, weakness, infections and suspected immune deficiency. Which STI is most likely indicated by these symptoms?
A patient presents with fever, weakness, infections and suspected immune deficiency. Which STI is most likely indicated by these symptoms?
What is the primary function of sustentacular (Sertoli) cells within the seminiferous tubules?
What is the primary function of sustentacular (Sertoli) cells within the seminiferous tubules?
If a male's interstitial cells were unable to produce testosterone, which of the following would NOT occur?
If a male's interstitial cells were unable to produce testosterone, which of the following would NOT occur?
What would be the most likely outcome if the bulbourethral glands failed to secrete mucus during sexual stimulation?
What would be the most likely outcome if the bulbourethral glands failed to secrete mucus during sexual stimulation?
Which physiological response would be impaired if the vas deferens were blocked?
Which physiological response would be impaired if the vas deferens were blocked?
How would a drug that inhibits the action of prostaglandins affect male fertility?
How would a drug that inhibits the action of prostaglandins affect male fertility?
What is the underlying reason that the testes are located in the scrotum rather than inside the abdominal cavity?
What is the underlying reason that the testes are located in the scrotum rather than inside the abdominal cavity?
Why is capacitation necessary for sperm to fertilize an egg?
Why is capacitation necessary for sperm to fertilize an egg?
If sustentacular cells were unable to produce inhibin, what would be the most likely consequence?
If sustentacular cells were unable to produce inhibin, what would be the most likely consequence?
If the fimbriae of the uterine tubes were non-functional, what would be the most likely consequence?
If the fimbriae of the uterine tubes were non-functional, what would be the most likely consequence?
How would a drug that blocks the secretion of GnRH from the hypothalamus affect female reproduction?
How would a drug that blocks the secretion of GnRH from the hypothalamus affect female reproduction?
Which of the following is a direct effect of declining estrogen levels during menopause?
Which of the following is a direct effect of declining estrogen levels during menopause?
Why is the timing of emergency contraception critical for preventing pregnancy?
Why is the timing of emergency contraception critical for preventing pregnancy?
The reproductive organs fully mature during the physiological timeframe known as
The reproductive organs fully mature during the physiological timeframe known as
The ______ sex organs in males are the two testes, in which sperm cells and the male sex hormones are formed. The ______ sex organs are the internal and external reproductive organs.
The ______ sex organs in males are the two testes, in which sperm cells and the male sex hormones are formed. The ______ sex organs are the internal and external reproductive organs.
Indicate which glands secrete hormones that control male reproductive functions. (Select all that apply)
Indicate which glands secrete hormones that control male reproductive functions. (Select all that apply)
Androgens and the 'andr-' root refer to ______ sex hormones.
Androgens and the 'andr-' root refer to ______ sex hormones.
Flashcards
Reproductive System
Reproductive System
The body system not needed to survive, but essential for reproduction.
Gonads
Gonads
Organs that produce gametes (sex cells) and hormones.
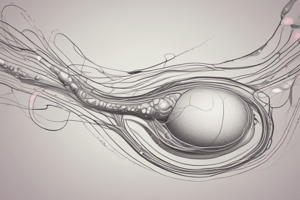
Sperm
Sperm
Male sex cells.
Oocytes
Oocytes
Signup and view all the flashcards
Testes
Testes
Signup and view all the flashcards
Scrotum
Scrotum
Signup and view all the flashcards
Seminiferous Tubules
Seminiferous Tubules
Signup and view all the flashcards
Spermatogenic Cells
Spermatogenic Cells
Signup and view all the flashcards
Interstitial (Leydig) Cells
Interstitial (Leydig) Cells
Signup and view all the flashcards
Epididymis
Epididymis
Signup and view all the flashcards
Ductus (Vas) Deferens
Ductus (Vas) Deferens
Signup and view all the flashcards
Ejaculatory Duct
Ejaculatory Duct
Signup and view all the flashcards
Seminal Vesicles
Seminal Vesicles
Signup and view all the flashcards
Prostate Gland
Prostate Gland
Signup and view all the flashcards
Bulbourethral (Cowper's) Glands
Bulbourethral (Cowper's) Glands
Signup and view all the flashcards
Semen
Semen
Signup and view all the flashcards
Capacitation
Capacitation
Signup and view all the flashcards
Scrotum
Scrotum
Signup and view all the flashcards
Penis
Penis
Signup and view all the flashcards
Corpora Cavernosa
Corpora Cavernosa
Signup and view all the flashcards
Glans Penis
Glans Penis
Signup and view all the flashcards
Prepuce
Prepuce
Signup and view all the flashcards
Erection
Erection
Signup and view all the flashcards
Emission
Emission
Signup and view all the flashcards
Ejaculation
Ejaculation
Signup and view all the flashcards
Orgasm
Orgasm
Signup and view all the flashcards
Androgens
Androgens
Signup and view all the flashcards
Testosterone
Testosterone
Signup and view all the flashcards
Spermatogonia
Spermatogonia
Signup and view all the flashcards
Primary Spermatocyte
Primary Spermatocyte
Signup and view all the flashcards
Meiosis
Meiosis
Signup and view all the flashcards
Spermatids
Spermatids
Signup and view all the flashcards
Sperm Cell
Sperm Cell
Signup and view all the flashcards
Gonadotropin-releasing hormone (GnRH)
Gonadotropin-releasing hormone (GnRH)
Signup and view all the flashcards
Luteinizing hormone (LH)
Luteinizing hormone (LH)
Signup and view all the flashcards
Follicle-stimulating hormone (FSH)
Follicle-stimulating hormone (FSH)
Signup and view all the flashcards
Lumen of Seminiferous Tubules
Lumen of Seminiferous Tubules
Signup and view all the flashcards
Study Notes
Introduction to the Reproductive Systems
- The reproductive system develops and maintains organs for production of offspring.
- It is the only body system not needed for survival.
- Gonads (testes and ovaries) produce gametes (sex cells and hormones).
- Male sex cells are sperm, while female sex cells are oocytes.
- The male system produces sperm and delivers them to the female.
- The female system houses and nourishes a developing embryo and fetus.
Organs of the Male Reproductive System
- Primary sex organs (gonads) of the male are the testes which produce sperm and hormones.
- Accessory (secondary) sex organs of the male include internal and external reproductive organs
Testes
- Testes are ovoid structures suspended by the spermatic cord outside the trunk in a sac called the scrotum.
Structure of the Testes
- Each testis consists of 250 lobules separated by connective tissue septa.
- Each lobule holds 1 to 4 coiled seminiferous tubules.
- Seminiferous tubules are lined with stratified epithelium containing spermatogenic cells that give rise to sperm cells.
- Channels leading from the seminiferous tubules carry sperm to the epididymis, which continues into the ductus deferens.
- Interstitial cells (cells of Leydig) lie between the seminiferous tubules and produce the male sex hormones.
Male Internal Accessory Reproductive Organs
- Nurture and transport sperm cells.
- Each testis is associated with an epididymis, a ductus deferens, and a seminal vesicle.
- Other internal accessory organs include the prostate gland and bulbourethral glands.
Epididymis and Ductus Deferens
- The epididymis is a tightly coiled tube connected to the testis, leading to the ductus deferens.
- This tube begins at the top of the testis, descends, then turns upward as the ductus deferens, and serves as the site of sperm maturation.
- Sperm become motile and develop the ability to fertilize an egg in the epididymis.
- The Ductus (Vas) Deferens is a muscular tube, 45 cm long, that transports sperm from the epididymis through the inguinal canal into the pelvic cavity.
- It unites with the seminal vesicle duct to form the ejaculatory duct.
- The ejaculatory duct travels through the prostate gland and empties its contents into the urethra.
Seminal Vesicles and Prostate Gland
- Seminal Vesicles are saclike structures attached to the vas deferens near the base of the urinary bladder.
- During emission, seminal vesicles secrete a fluid that makes up a large portion of the semen, contains fructose to nourish sperm, and has prostaglandins to cause muscular contractions in the female tract.
- The alkaline pH helps regulate pH in the male reproductive tract and the vagina of the female reproductive tract.
- The Prostate Gland is a chestnut-shaped structure surrounding the urethra at the base of the urinary bladder.
- Secretes a milky fluid that contributes to the volume of the semen and contains citrate, a nutrient for sperm, and prostate-specific antigen (PSA), an enzyme which helps to liquefy semen.
Bulbourethral Glands and Semen
- The bulbourethral glands (Cowper's glands) are small glands located inferior to the prostate gland and secrete mucus into the urethra to lubricate the tip of the penis during sexual stimulation.
- Semen is reproductive fluid transported through the urethra to the outside of the body during ejaculation.
- Semen contains sperm cells (120 million per milliliter) and the secretions of the seminal vesicles, prostate gland, and bulbourethral glands.
- Sperm cells cannot fertilize an egg until they undergo capacitation within the female reproductive tract.
- Semen is slightly alkaline, to protect sperm from acids in male and female tracts, and capacitation involves weakening of the acrosomal membrane of the sperm.
Male External Accessory Reproductive Organs
- Scrotum: a pouch of skin and subcutaneous tissue that houses the testes, suspended from the lower abdomen and protects and helps regulate the temperature of the testes (sperm production needs temperature 5°F cooler than core).
- Penis: Cylindrical organ that conveys both urine and semen to the outside.
- It contains specialized erectile tissue (corpora cavernosa and corpus spongiosum), which stiffens for sexual intercourse.
- The corpus spongiosum (encircles the urethra) enlarges at its distal end to form the glans penis, which is covered by a loose fold of skin (prepuce).
Erection, Orgasm, and Ejaculation
- During sexual arousal, parasympathetic impulses trigger the release of nitric oxide (NO), which increases blood flow into erectile tissues of the penis.
- Vasodilation of arteries in erectile tissue and compression of veins leading out of this tissue cause the penis to swell and elongate, resulting in erection.
- Emission involves the movement of sperm cells and accessory gland secretions into the urethra, where they blend to form semen and is controlled by sympathetic impulses
- Ejaculation involves forcing semen through the urethra to the outside of the body.
- After ejaculation, sympathetic impulses constrict the arteries and the penis returns to a flaccid state.
- Orgasm is the culmination of sexual stimulation and is a feeling of psychological and physiological release.
Functions of the Male Reproductive Organs
- Testis: Produce sperm cells and secrete male sex hormones.
- Epididymis: Promotes sperm cell maturation, stores sperm cells, conveys sperm cells to ductus deferens.
- Ductus Deferens: Conveys sperm cells to ejaculatory duct.
- Seminal Vesicle: Secretes an alkaline fluid containing nutrients and prostaglandins that helps regulate pH semen.
- Prostate Gland: Secretes a fluid that contains citrate, a nutrient for sperm.
- Bulbourethral gland: Secretes lubricating fluid.
- Scrotum: Encloses, protects, and regulates temperature of testes.
- Penis: Conveys urine and semen to outside of body; inserted into vagina during sexual intercourse. The glans penis supplied with sensory nerve endings associated with feelings of pleasure during sexual stimulation.
Spermatogenesis
- Epithelium of the seminiferous tubules contains sustentacular (Sertoli) cells and spermatogenic cells.
- Sustentacular (Sertoli) cells support, nourish, and regulate spermatogenic cells.
- In a male embryo, spermatogenic cells are undifferentiated cells called spermatogonia, each containing 46 chromosomes.
- Hormones stimulate spermatogonia to undergo mitosis to produce the following cells, starting during embryonic development:
- Type A cell remains a spermatogonium to maintain the supply.
- Type B cell becomes a primary spermatocyte, and will undergo meiosis to become a sperm.
- Spermatogenesis is now arrested until puberty.
Formation of Sperm Cells
- Mitosis resumes at puberty, new spermatogonia are produced, and some spermatogonia mature into primary spermatocytes.
- Under the influence of testosterone, primary spermatocytes undergo a special sex cell division called meiosis.
- Meiosis has 2 successive divisions: these are the first and second meiotic divisions
- Meiosis 1 (first meiotic division): Separation of homologous (like) chromosome pairs, containing the same genes on both chromatids (strands) of the pair.
- Some genes on the 2 chromatids are not identical.
- Primary spermatocytes divide to form secondary spermatocytes, with 23 chromosomes. Each contains 1 member of each homologous pair, and is a haploid cell.
- Meiosis 2:
- Secondary spermatocytes divide by separating chromatids of each pair and produces 2 spermatids.
- Once the chromatids are separated, each is considered a complete chromosome.
- Each spermatid matures into a sperm cell.
- Each primary spermatocyte that begins meiosis I produces 4 sperm with 23 single-stranded chromosomes.
- Spermatogenesis occurs continually in a male, starting at puberty.
- Sperm collect in the lumen of seminiferous tubules, then move into the epididymis to mature.
Sperm Cell Structure
- A mature sperm is shaped like a tadpole.
- The head consists of an oval haploid nucleus and an acrosome with digestive enzymes for eroding tissues around the female egg cell.
- A midpiece (body) contains mitochondria and a flagellum (tail) provides lashing movements to propel sperm.
Hormonal Control of Male Reproductive Functions
- The hypothalamus, anterior pituitary, and testes control male reproductive function through hormones.
- Hormones control the development and maintenance of secondary sexual characteristics and sperm cell production.
- Gonadotropin-releasing hormone (GnRH): Secreted by the hypothalamus, GnRH triggers the production of gonadotropins from the anterior pituitary gland.
- The actions of GnRH result in the development of interstitial cells of the testes; these cells then secrete male hormones (especially testosterone), and cause sustentacular cells of seminiferous tubules to responds to testosterone.
Male Sex Hormones
- Androgens are male sex hormones, chief among them testosterone.
- Secretion occurs in a fetus until birth, then nearly ceases during childhood, increasing rapidly at puberty, then continuing throughout life.
- Actions of testosterone: Stimulates male reproductive organ development, responsible for male secondary sexual characteristics such as deep voice, body hair, etc.
- These actions also increase the rate of metabolism and red blood cell production and stimulate sexual activity.
- Development of male secondary sexual characteristics depends on amount of testosterone secreted.
- A negative feedback system involving the hypothalamus regulates testosterone production.
Organs of the Female Reproductive System
- Produce and maintain sex cells (egg cells, oocytes).
- Transport these cells to the site of fertilization.
- Provide environment for a developing fetus..
- Transport offspring to the outside.
- Produce female sex hormones..
- Considered primary sex organs (gonads): the ovaries which produce the sex cells and hormones.
- Secondary (accessory) sex organs consist of the external and internal reproductive organs.
Ovaries
- These are solid, ovoid structures, located within the lateral wall of the pelvic cavity.
- They are subdivided into an inner medulla and an outer cortex:
- Medulla has connective tissue, blood vessels, lymphatic vessels, and nerves.
- Cortex contains ovarian follicles and is covered by cuboidal (germinal) epithelium.
- Ovaries are held in place by ligaments.
Primordial Follicles
- Millions of primordial follicles form from groups of cells in the ovarian cortex during prenatal development.
- Each consists of a primary oocyte surrounded by a single layer of simple squamous epithelial cells, also called follicular cells.
- Early in fetal development, primary oocytes begin meiosis, but it stops until puberty.
- No new primordial follicles are produced in a female's lifetime, and oocyte degeneration causes a continuous decline.
Female Internal Accessory Reproductive Organs
- Includes uterine tubes, uterus, and vagina.
- Uterine tubes (oviducts or fallopian tubes) lead from the ovary to the uterus.
- The tubes expand near ovaries to form an infundibulum with fingerlike fimbriae on its margins.
- Cells lining the tubes have cilia which beat in unison, drawing egg cell into the uterine tube – which is the normal site of fertilization.
Uterus
- A hollow, muscular, pear-shaped organ.
- It receives embryo from uterine tube, and maintains development of the embryo and then fetus.
- The upper two-thirds (body) has a dome-shaped top (fundus).
- The lower one-third is the cervix, which extends into the vagina Uterine wall has three layers including an inner endometrium, a muscular myometrium, and an outer perimetrium.
- It usually bends forward over the urinary bladder.
Vagina
- A fibromuscular tube that extends from the uterus to the outside of the body.
- The vaginal orifice is partially covered by a membrane called the hymen.
- The vaginal wall has 3 layers including an inner mucosal layer, middle muscular layer, and an outer fibrous layer
- It conveys uterine secretions, receives the penis during sexual intercourse, and serves as passageway for birth.
Female External Accessory Reproductive Organs
- Includes labia majora, labia minora, clitoris, and vestibular glands.
- Structures surrounding openings of urethra and vagina make up the vulva.
- Labia Majora: enclose and protect other external organs and correspond to the scrotum of the male.
- They consist of folds of adipose tissue covered by skin, which meet to form the mons pubis, which covers the pubic symphysis.
- The Labia Minora: flattened, longitudinal folds between the labia majora. They merge with labia majora and form a hood around the clitoris.
- Clitoris: small projection at anterior end of vulva, between labia minora and has a similar structure to the penis, and it contains columns of erectile tissue.
- Vestibule: a space enclosed by the labia minora, into which the vagina and urethra open. Vestibular glands lie on either side of the vaginal opening and correspond to bulbourethral glands.
Erection, Lubrication, Orgasm
- During periods of sexual stimulation, the erectile tissues of the clitoris and vaginal opening engorge due to action of nitric oxide (NO).
- The vestibular glands secrete mucus into the vestibule for lubrication.
- Sexual stimulation causes nerve fibers in the clitoris to respond, culminating in orgasm.
- During orgasm, muscles of the perineum, uterine wall, and uterine tubes contract rhythmically.
- This helps convey sperm through the female to the uterine tubes.
Functions of the Female Reproductive Organs
- Ovary produces oocytes and female sex hormones.
- Uterine tube conveys secondary oocyte toward uterus.
- Uterus protects and sustains embryo during pregnancy.
- Vagina is a passageway for offspring during birth.
- Labia majora encloses and protect other external reproductive organs.
- Labia minora form margins of vestibule and protect openings of vagina and urethra.
- Clitoris produces pleasure during sensory stimulation due to abundant sensory nerve endings in the glans.
- and openings of vagina/urethra: vestibular – space between labia minora that contains vaginal urethral/glands secreate lubrication.
Oogenesis and Ovarian Cycle
- This is the process of oocyte (egg cell) formation.
- Beginning at puberty, some primary oocytes continue meiosis produce a cell with half the number of chromosomes as the parent cells.
- Division of primary oocytes produces a secondary oocyte and a first polar body.
- Upon fertilization, 2nd oocyte undergoes 2nd division and becomes a ovum Sperm chromosomes unite with ovum becoming a zygote.
- After fertilization and forming zygote, the 2 polar bodies degenerate Haploid oocyte produce the large amounts of cytoplasm
Oogenesis
- Oogonia give rise to oocytes. Before birth, oogonia multiply by mitosis.
- During development of the fetus, many oogonia begin meiosis stop in prophase 1 and are now called primary.
- They remain in this state until puberty, becoming surrounded by a single layer of flattened follicular cells that create a primordial follicle.
- After puberty, follicles develop into primary and after fluid fill form they are named antral follicles.
- After puberty, one follicle becomes a dominant antral follicle and the primary oocyte completes Meiosis 1 creating secondary oocyte, the secondary oocyte begines meiosis 2 until metaphase 2
- If the sperm manages to reach the fallopian tubes and combines with the secondary oocyte forming fertilization then meiosis 2 will continue.
- After ovulation, the granulosa turns into corpus luteum, the corpus luteum degenerates and scar to corpus albicans
Follicle Maturation
- At puberty, follicle stimulating hormone (FSH) secreation leads to enlargement.
- During reproductive years, primordial follicle grows to form primary with one cubodial ephitheral cell, the oocyte is then enlarged
- As granulosa cells form layers it become secondary
- As organization of outer layer and liquid form and create antrum, structure will named as antral follicle. the oocyte is surrounded by zona pellucida and granulosa cells, also known as corona radiata
Ovulation
- A surge of Luteinzing hormone (LH) from the anterior pituitary causes this.
- Occurs when mature antral ruptures
- Releases secondary oocyte and and 1-2 layers granulosa cell into urine
- Degenerate hours of being released if there a fertilization
Female Sex Hormones
- These Hormones control female development, and ovary
- At 10 year old the hypothalamus will secreate (GnRH) wich produce LH and FSH in the anntior pituitary to product 2 main hormones group
- Estrogen
- Progesterone
Female Hormones, continued.
- Ovaries are main source of estrogen when not pregnant
- Estrogen resposible for sex structure, organ enlargement, adipose tissue and skin vascula
- Ovaries are also main source of progesteronr not pregranted, wich cause uterine changes during menstrual cycle
- Androgen : Puberty, which cause hairs grow and change hips
Menstrual Cycle
- Which lead to menstrual flow
- first reproductive cycle for maturation and organs growth.
Events in the Cycle
- Pituitary glands secreate FSH and LH. FSH stimulate the follicle maturity and granulosa cells stimulate and secreate estrogen
- surge of release for ovulation from anterior to corpus luteum
- Estegen cause uteerine layer devlopment
- Progesterone stimulate endomertrium gland and vascularize, and secreate FSH and LH from anntior pituitary gland
Cycle Cont
- Oocyte no fertilize or degenerates
- Estrogens no longer screate
- Intergrates and sloughing
- The anterior has less of the release and no cycle anymore due to inhlbition; the cycle can be repeated and occur a new antral
Menopause (Female Climacteric)
- Occurs in late 40s or early 50s. Ovaries produces less. Cycles irregular, eventually stops and mark complete year with no cycles as menopause.
- Estrogen causes a decrease in uterine, breast tubes, vasgina adn thinner pubuc ahic and risk to cardiovascular disease
- Bone loss, mood changes, lining also may be involved.
Mammary Glands
- Accessory of organs for reproduction, specialized to produce milk after pregnancy
- Lie in breasts of interior thorax overlying major muscle. The area pigmental skin
- Also known as Areola
- Composited of 15 20 lobes with lactiferous duct
- Dense connective tissue fat separate the lobes
- As puberty happens, glands develop more due to the infulence of ovary hormones, whereas male glands do not progress
Birth Control
- Voluntarily regulate the number of offspring produced
- Using contraception avoid fertilization or prevent the implementation - of a blastocyst
Methods of Contraception
- Coitus in interruption- pull out method
- Abstinence for rhythm cycle - is not effective
- Mechanic barriers = condom and diagphram
- Chemical barrier = spermicides
- Hormone Contraceptive = normal cycle
- Injectable = hormone, 3 months and block cycle
- Contraceptive implant = can prevenrt the hormones and block years
- IUD/Inrauterine Devices: cause death of zygote or block embryo
- Emergency: morning after; after sexual inercourse
- Sterlization method permanently; sperm being relesead - vasectomy / cut the semeni and cut the fillipian tubules ; tubbal ligation
- STIS STD = transmission that can be transmitted , you can also transmit without any symptoms yourself
- High common include simarities : fever, sores, blisters and rashes ; adominanl pains and discharge
Sexual Infections
- Many STIs can have fever, sores, blisters or rashes, lower painful intercourse, or discharge.
- Females can be silent and undetected.
- Possible Complications (STIS (gonorrhea and chlamydia)), infection female infertility sterility (peliv inflame) Acquired deficiency syndrome (AIDS), transmitted sexu transmission. Destructy immune system, cancers can be fatal or harmul.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.