Podcast
Questions and Answers
What is the primary role of luteinizing hormone (LH) in the male reproductive system?
What is the primary role of luteinizing hormone (LH) in the male reproductive system?
- Stimulating sperm production directly within the seminiferous tubules.
- Facilitating the descent of the testes from the abdominal cavity into the scrotum.
- Stimulating the secretion of testosterone by cells located between the seminiferous tubules. (correct)
- Regulating the temperature within the scrotum to optimize sperm development.
Why is the temperature inside the scrotum lower than the internal body temperature?
Why is the temperature inside the scrotum lower than the internal body temperature?
- To promote the process of meiosis in sperm production.
- To ensure the proper development and survival of sperm cells. (correct)
- To facilitate the production of testosterone by Leydig cells.
- To protect the sperm from the immune system.
Which of the following correctly describes the process of sperm formation in the male reproductive system?
Which of the following correctly describes the process of sperm formation in the male reproductive system?
- Sperm form through mitosis in the lining of the vas deferens.
- Sperm form through meiosis in the interstitial cells surrounding the seminiferous tubules.
- Sperm form through meiosis in the specialized lining of the seminiferous tubules. (correct)
- Sperm form through mitosis in the specialized lining of the seminiferous tubules.
If a drug inhibited the action of Follicle-Stimulating Hormone (FSH) in males, what would be the most likely direct effect?
If a drug inhibited the action of Follicle-Stimulating Hormone (FSH) in males, what would be the most likely direct effect?
What is the outcome of meiosis in cells that produce sperm within the testes?
What is the outcome of meiosis in cells that produce sperm within the testes?
Which of the following best describes the function of the seminiferous tubules?
Which of the following best describes the function of the seminiferous tubules?
A male patient has a condition where his Sertoli cells are not functioning correctly. Which of the following is the most likely consequence of this condition?
A male patient has a condition where his Sertoli cells are not functioning correctly. Which of the following is the most likely consequence of this condition?
If the scrotum's temperature regulation mechanism failed, and the testes were consistently at the normal body temperature of 37°C, what would be the most likely result?
If the scrotum's temperature regulation mechanism failed, and the testes were consistently at the normal body temperature of 37°C, what would be the most likely result?
What is the primary function of the enzymes located in the head region of a mature sperm?
What is the primary function of the enzymes located in the head region of a mature sperm?
Which structure provides the energy required for a sperm to reach an egg?
Which structure provides the energy required for a sperm to reach an egg?
What changes occur to sperm while they are in the epididymis?
What changes occur to sperm while they are in the epididymis?
What is the role of the vas deferens in the male reproductive system?
What is the role of the vas deferens in the male reproductive system?
Which of the following is NOT a gland that secretes fluids which mix with sperm in the urethra?
Which of the following is NOT a gland that secretes fluids which mix with sperm in the urethra?
What component of semen stimulates contractions in the female reproductive tract to aid sperm movement?
What component of semen stimulates contractions in the female reproductive tract to aid sperm movement?
What is the primary purpose of the alkaline fluid secreted by the prostate gland?
What is the primary purpose of the alkaline fluid secreted by the prostate gland?
Why is it important the bulbourethral glands secrete alkaline fluid before sperm leave the body?
Why is it important the bulbourethral glands secrete alkaline fluid before sperm leave the body?
What physiological change occurs in the penis to enable sperm deposition in the female reproductive system?
What physiological change occurs in the penis to enable sperm deposition in the female reproductive system?
Despite the large number of sperm released during ejaculation, why do relatively few reach the site of fertilization?
Despite the large number of sperm released during ejaculation, why do relatively few reach the site of fertilization?
Flashcards
Testes
Testes
The gamete-producing organs of the male reproductive system.
Seminiferous Tubules
Seminiferous Tubules
Tightly coiled tubules within the testes where sperm forms through meiosis.
Scrotum
Scrotum
The external sac that holds the testes.
Puberty
Puberty
Signup and view all the flashcards
Luteinizing Hormone (LH)
Luteinizing Hormone (LH)
Signup and view all the flashcards
Testosterone
Testosterone
Signup and view all the flashcards
Follicle-Stimulating Hormone (FSH)
Follicle-Stimulating Hormone (FSH)
Signup and view all the flashcards
Meiosis
Meiosis
Signup and view all the flashcards
Sperm Structure
Sperm Structure
Signup and view all the flashcards
Sperm Head
Sperm Head
Signup and view all the flashcards
Sperm Midpiece
Sperm Midpiece
Signup and view all the flashcards
Epididymis
Epididymis
Signup and view all the flashcards
Vas Deferens
Vas Deferens
Signup and view all the flashcards
Urethra (Male)
Urethra (Male)
Signup and view all the flashcards
Male Exocrine Glands
Male Exocrine Glands
Signup and view all the flashcards
Seminal Vesicles
Seminal Vesicles
Signup and view all the flashcards
Prostate Fluid
Prostate Fluid
Signup and view all the flashcards
Semen
Semen
Signup and view all the flashcards
Study Notes
- Sexual reproduction involves the formation of a diploid zygote from two haploid gametes through fertilization.
- A male's roles in sexual reproduction include producing sperm cells and delivering them to the female reproductive system to fertilize an egg cell.
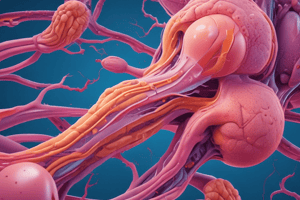
Male Reproductive System
- The male reproductive system contains two egg-shaped testes.
- Testes are the gamete-producing organs.
- Each testis is about 4 cm (1.5 in.) long and 2.5 cm (1 in.) in diameter.
- Each testis has about 250 compartments containing tightly coiled seminiferous tubules.
- Each seminiferous tubule is approximately 80cm (32 in.) long.
- Total length of seminiferous tubules in both testes is about 500m (1,640 ft).
- Sperm form through meiosis in the lining of these tubules.
- Testes develop within the abdominal cavity and descend into the scrotum before birth.
- The scrotum maintains a temperature about 2°C to 3°C cooler than the abdomen.
- This lower temperature is essential for normal sperm development.
- Sperm production begins during puberty.
- Luteinizing hormone (LH) stimulates testosterone secretion.
- Testosterone, the main androgen, is produced by cells between the seminiferous tubules.
- Follicle-stimulating hormone (FSH), along with testosterone, stimulates sperm production.
- Males continue to produce sperm as long as testosterone levels are high enough.
- Meiosis reduces the chromosome number from diploid (2n) to haploid (1n).
- During meiosis in sperm cells, the chromosome number drops from 46 to 23.
- Each cell undergoing meiosis results in four sperm cells.
Sperm Structure
- Mature sperm consists of a head, midpiece, and tail (flagellum).
- The head contains enzymes to penetrate the egg's protective layers during fertilization.
- It also contains 23 chromosomes.
- The midpiece is packed with mitochondria, providing energy for sperm to reach the egg.
- The tail is a flagellum that propels the sperm.
Path of Sperm Through the Male Body
- Mature sperm move through several reproductive structures.
- Sperm move from the seminiferous tubules to the epididymis.
- The epididymis is a long, coiled tubule attached to each testis where sperm mature and gain the ability to swim.
- Sperm are stored in the epididymis.
- Some sperm leave the epididymis and pass through the vas deferens.
- The vas deferens is a duct extending from the epididymis.
- Smooth muscles in the vas deferens contract to move sperm.
- Each vas deferens enters the abdominal cavity, loops around the bladder, and merges with the urethra.
- The urethra is the duct for urine excretion.
- In males, both urine and sperm exit through the urethra, but not simultaneously.
- In the urethra, sperm mix with fluids from the seminal vesicles, prostate gland, and bulbourethral glands.
- These glands secrete fluids that nourish and protect sperm.
- Seminal vesicles produce a sugar-rich fluid for energy.
- The prostate gland secretes an alkaline fluid to neutralize acids in the female reproductive system.
- Bulbourethral glands secrete an alkaline fluid to neutralize acidic urine traces in the urethra.
- Sperm and secretions form semen.
- Semen contains prostaglandins that stimulate contractions in the female reproductive tract.
Delivery of Sperm
- The urethra passes through the penis.
- The penis deposits sperm into the female reproductive system.
- During sexual arousal, spongy tissue in the penis fills with blood, causing an erection.
- Ejaculation is the forceful expulsion of semen from the penis.
- Each ejaculation expels 3 to 4 mL of semen.
- Sperm make up only 10 percent of the semen volume.
- A single ejaculation can expel 300 million to 400 million sperm.
- Few sperm reach the fertilization site due to the acidic environment of the female reproductive tract.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Explore the male reproductive system, focusing on the testes and sperm production. Learn about the structure of the testes, the role of seminiferous tubules, and the importance of temperature regulation for sperm development.