Podcast
Questions and Answers
What is a primary symptom of rheumatoid arthritis that typically occurs in the morning?
What is a primary symptom of rheumatoid arthritis that typically occurs in the morning?
- Morning stiffness (correct)
- Fever
- Joint swelling
- Weight gain
Which joints are most commonly involved in rheumatoid arthritis?
Which joints are most commonly involved in rheumatoid arthritis?
- Elbow joints
- Shoulder joints
- Metacarpophalangeal (MCP) joints (correct)
- Distal interphalangeal (DIP) joints
Which of the following is NOT a common symptom of rheumatoid arthritis?
Which of the following is NOT a common symptom of rheumatoid arthritis?
- Fatigue
- Severe joint pain localized to one joint (correct)
- Depression
- Weight loss
What is one of the goals of treatment in managing rheumatoid arthritis?
What is one of the goals of treatment in managing rheumatoid arthritis?
Which of the following symptoms is considered an extra-articular manifestation of rheumatoid arthritis?
Which of the following symptoms is considered an extra-articular manifestation of rheumatoid arthritis?
What is a potential adverse effect of treatments for rheumatoid arthritis that requires monitoring?
What is a potential adverse effect of treatments for rheumatoid arthritis that requires monitoring?
What type of pain pattern is typical in rheumatoid arthritis?
What type of pain pattern is typical in rheumatoid arthritis?
Which of the following statements about rheumatoid arthritis is true?
Which of the following statements about rheumatoid arthritis is true?
Which laboratory finding is NOT typically associated with rheumatoid arthritis (RA)?
Which laboratory finding is NOT typically associated with rheumatoid arthritis (RA)?
What is the primary goal of treatment for rheumatoid arthritis?
What is the primary goal of treatment for rheumatoid arthritis?
Which of the following is NOT considered a non-drug intervention in the management of rheumatoid arthritis?
Which of the following is NOT considered a non-drug intervention in the management of rheumatoid arthritis?
What does an increase in C-reactive protein (CRP) indicate in the context of rheumatoid arthritis?
What does an increase in C-reactive protein (CRP) indicate in the context of rheumatoid arthritis?
Which of the following is a significant risk factor associated with higher mortality rates in rheumatoid arthritis?
Which of the following is a significant risk factor associated with higher mortality rates in rheumatoid arthritis?
Which type of anaemia is commonly observed in individuals with rheumatoid arthritis?
Which type of anaemia is commonly observed in individuals with rheumatoid arthritis?
What lifestyle change is recommended to individuals managing rheumatoid arthritis?
What lifestyle change is recommended to individuals managing rheumatoid arthritis?
What is a common characteristic of changes observed in joint radiographs of rheumatoid arthritis patients?
What is a common characteristic of changes observed in joint radiographs of rheumatoid arthritis patients?
What is the primary purpose of biological DMARDs?
What is the primary purpose of biological DMARDs?
Which biological DMARD is NOT a TNF-α inhibitor?
Which biological DMARD is NOT a TNF-α inhibitor?
What should be avoided to minimize risks associated with biological DMARDs?
What should be avoided to minimize risks associated with biological DMARDs?
What type of infections should patients on biological DMARDs be monitored for?
What type of infections should patients on biological DMARDs be monitored for?
Which of the following vaccines is particularly significant for patients on biological DMARDs?
Which of the following vaccines is particularly significant for patients on biological DMARDs?
TNF-α inhibitors are contraindicated in which condition?
TNF-α inhibitors are contraindicated in which condition?
Which of the following is NOT a common adverse effect of TNF-α inhibitors?
Which of the following is NOT a common adverse effect of TNF-α inhibitors?
Which of these methods is important before starting treatment with TNF-α inhibitors?
Which of these methods is important before starting treatment with TNF-α inhibitors?
What is the primary goal in the early treatment of rheumatoid arthritis using synthetic DMARDs?
What is the primary goal in the early treatment of rheumatoid arthritis using synthetic DMARDs?
What is the initial dosing regimen for Sulfasalazine in mild disease?
What is the initial dosing regimen for Sulfasalazine in mild disease?
Which condition should be excluded before starting Hydroxychloroquine?
Which condition should be excluded before starting Hydroxychloroquine?
What is the typical onset time for Sulfasalazine to show effects?
What is the typical onset time for Sulfasalazine to show effects?
What side effect risk is specifically associated with Hydroxychloroquine?
What side effect risk is specifically associated with Hydroxychloroquine?
Which biological DMARD has the longest onset time before effects may be seen?
Which biological DMARD has the longest onset time before effects may be seen?
What is the primary route of administration for Tofacitinib?
What is the primary route of administration for Tofacitinib?
Which of the following options requires monitoring of lipid levels as part of its management?
Which of the following options requires monitoring of lipid levels as part of its management?
Which adverse effect is common across most biological DMARDs?
Which adverse effect is common across most biological DMARDs?
Which drug is used for severe rheumatoid arthritis that does not respond to TNF-α inhibitors?
Which drug is used for severe rheumatoid arthritis that does not respond to TNF-α inhibitors?
What type of adverse effects are associated with Anakinra?
What type of adverse effects are associated with Anakinra?
Which of the following drugs has a contraindication for patients with tuberculosis?
Which of the following drugs has a contraindication for patients with tuberculosis?
What is the onset time for Abatacept to show effects?
What is the onset time for Abatacept to show effects?
Flashcards are hidden until you start studying
Study Notes
Learning Outcomes
- Identify signs, symptoms, and diagnostic lab tests for rheumatoid arthritis (RA).
- Understand the treatment goals for RA management.
- Recognize the management strategies for RA.
- Be aware of monitoring for disease progression and treatment-related adverse effects.
Diagnosis and Clinical Findings
- RA symptoms are gradual and include malaise, fatigue, and musculoskeletal pain.
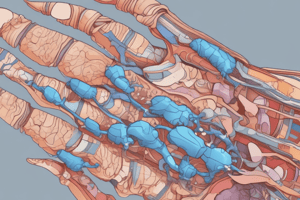
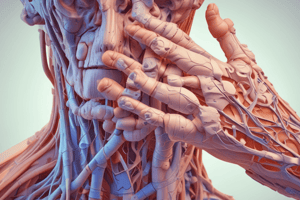
- Joint symptoms typically exhibit a symmetrical pattern: pain, stiffness, swelling, and redness, especially in MCP, PIP, and MTP joints.
- Morning stiffness, weight loss, fever, and depression may also occur as extra-articular symptoms.
Biological DMARDs
- Reserved for patients unresponsive to synthetic DMARDs.
- Commonly combined with methotrexate - using more than one biological DMARD increases infection risk.
- Key biological DMARDs include TNF-α inhibitors, Rituximab, Abatacept, Anakinra, Tocilizumab, and Tofacitinib.
- Vaccination against pneumonia, influenza, hepatitis A and B, and HPV is recommended.
TNF-α Inhibitors
- First-line biological agents: Adalimumab, Certolizumab, Etanercept, Golimumab, Infliximab.
- Rapid onset but contraindicated in patients with TB or hepatitis infections.
- Potential adverse effects: injection site reactions, upper respiratory infections, thrombocytopenia, and malignancies.
- Regular monitoring of FBP, CrCl, and LFT is essential.
Rituximab
- Recommended for severe RA not responding to TNF-α inhibitors.
- Onset of effect takes about 4 months; administered through IV infusion.
- Common side effects include infusion reactions and muscle pain, necessitating monitoring of FBP, LFT, and CrCl.
Abatacept
- For RA unresponsive to TNF-α inhibitors, onset in approximately 14 days; IV administration.
- Notable side effects: hypertension and increased liver enzymes, requiring same monitoring protocols as Rituximab.
Anakinra
- Slower onset (2 weeks) and less effective than TNF-α inhibitors, delivered via SC injection.
- Risks include injection site reactions and neutropenia; monitor FBP and lipid profile.
Tocilizumab
- Onset of action between 2-4 weeks; administered via IV infusion.
- Possible adverse reactions include infections and GI ulcers; monitoring includes FBP, LFT, and lipid levels.
Tofacitinib
- For moderate to severe RA not responding to methotrexate or TNF antagonists.
- Can be used alone or in combination (excluding cyclosporine, azathioprine).
- Watch for adverse effects such as elevated LFT and risk of infections; regular monitoring of FBC, Hb, lipid levels, and LFT required.
Laboratory Findings
- Elevated ESR and C-reactive protein levels; presence of rheumatoid factor, HLA typing, and antibodies such as ANA and CCP.
- Anemia typical, presenting as normocytic/microcytic alongside low serum iron levels.
Prognosis
- Disability is common, significantly impacting quality of life.
- Mortality rates are 2-3 times higher with extra-articular manifestations like infections or cardiovascular diseases.
Treatment Goals
- Primary objective is achieving remission: reduce symptoms, normalize inflammatory markers, and eliminate joint swelling.
- Enhance joint and muscle function, minimize treatment side effects, restore quality of life, and prevent co-morbidities.
Non-Drug Interventions
- Recommendations include physical therapy, exercise, dietary changes, occupational therapy for assistive devices, smoking cessation, and immunisation.
- Omega-3 fatty acids and gamma-linolenic acid supplements may be beneficial.
Synthetic DMARDs
- Introduce early for optimal effectiveness; aims for rapid inflammation control to reduce joint damage.
- Sulfasalazine is first-line for mild disease, with dosage adjustments required based on tolerance and monitoring for blood dyscrasias.
Hydroxychloroquine
- Also first-line for mild disease but primarily used in combination therapy due to its lower efficacy.
- Monitoring for retinopathy and psoriasis worsening is essential; standard dosing is 200 to 400 mg daily.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.