Podcast
Questions and Answers
Which of the following is the primary goal of drug therapy for rheumatoid arthritis (RA)?
Which of the following is the primary goal of drug therapy for rheumatoid arthritis (RA)?
- Eradicating the autoimmune response.
- Curing RA completely.
- Decreasing joint pain and inflammation. (correct)
- Reversing joint deformities.
Which drug categories are typically used in the treatment of rheumatoid arthritis(RA)?
Which drug categories are typically used in the treatment of rheumatoid arthritis(RA)?
- Antifungals, antivirals, and antibiotics.
- Antihistamines, decongestants, and antitussives.
- Diuretics, antiarrhythmics, and antihypertensives.
- NSAIDS, glucocorticoids, and disease-modifying antirheumatic drugs (DMARDs). (correct)
What is the primary mechanism of action of nonbiologic DMARDs in treating rheumatoid arthritis (RA)?
What is the primary mechanism of action of nonbiologic DMARDs in treating rheumatoid arthritis (RA)?
- Stimulating the production of synovial fluid.
- Interfering with normal B and T lymphocytes activity to exert an immunosuppressive effect. (correct)
- Blocking pain signals in the brain.
- Directly repairing damaged joint tissue.
Which of the following best describes the mechanism of action of biologic DMARDs?
Which of the following best describes the mechanism of action of biologic DMARDs?
A patient is prescribed methotrexate for rheumatoid arthritis. What important monitoring should the nurse implement?
A patient is prescribed methotrexate for rheumatoid arthritis. What important monitoring should the nurse implement?
Which of the following instructions is most important for a nurse to provide to a patient starting on methotrexate?
Which of the following instructions is most important for a nurse to provide to a patient starting on methotrexate?
A patient taking methotrexate should be instructed to also take which of the following supplements?
A patient taking methotrexate should be instructed to also take which of the following supplements?
Which of the following nursing interventions is crucial when administering nonbiologic DMARDs?
Which of the following nursing interventions is crucial when administering nonbiologic DMARDs?
A patient is prescribed etanercept (Enbrel) for rheumatoid arthritis. What is an important instruction to include in the patient's education?
A patient is prescribed etanercept (Enbrel) for rheumatoid arthritis. What is an important instruction to include in the patient's education?
Prior to initiating etanercept (Enbrel) therapy, which of the following tests is most important for the nurse to ensure has been performed?
Prior to initiating etanercept (Enbrel) therapy, which of the following tests is most important for the nurse to ensure has been performed?
Which of the following assessment findings would be most concerning in a patient receiving etanercept (Enbrel)?
Which of the following assessment findings would be most concerning in a patient receiving etanercept (Enbrel)?
Which of the following instructions should be included in the teaching plan for a patient who is newly prescribed etanercept?
Which of the following instructions should be included in the teaching plan for a patient who is newly prescribed etanercept?
When providing education to a patient about raloxifene (Evista), what should the nurse emphasize regarding health promotion?
When providing education to a patient about raloxifene (Evista), what should the nurse emphasize regarding health promotion?
What is the primary goal of drug therapy for osteoporosis?
What is the primary goal of drug therapy for osteoporosis?
Calcitonin is prescribed for a patient with osteoporosis. What allergy should the nurse assess for?
Calcitonin is prescribed for a patient with osteoporosis. What allergy should the nurse assess for?
A patient is prescribed alendronate (Fosamax) for osteoporosis. Which instruction is most important for the nurse to provide to the patient?
A patient is prescribed alendronate (Fosamax) for osteoporosis. Which instruction is most important for the nurse to provide to the patient?
A patient taking alendronate (Fosamax) reports new onset of dysphagia and severe heartburn. What action should the nurse take?
A patient taking alendronate (Fosamax) reports new onset of dysphagia and severe heartburn. What action should the nurse take?
A patient with osteoporosis is prescribed calcitonin-salmon nasal spray. Which of the following is an important instruction for the nurse to include when teaching the patient about this medication?
A patient with osteoporosis is prescribed calcitonin-salmon nasal spray. Which of the following is an important instruction for the nurse to include when teaching the patient about this medication?
What is the primary mechanism of action of bisphosphonates in treating osteoporosis?
What is the primary mechanism of action of bisphosphonates in treating osteoporosis?
Why should calcium supplements not be taken at the same time as bisphosphonates? (Select all that apply.)
Why should calcium supplements not be taken at the same time as bisphosphonates? (Select all that apply.)
The nurse anticipates which follow-up test after a postmenopausal woman presents with a tibial fracture confirmed by x-ray?
The nurse anticipates which follow-up test after a postmenopausal woman presents with a tibial fracture confirmed by x-ray?
What are the most important supplements for bone health for patients of advancing age?
What are the most important supplements for bone health for patients of advancing age?
The nurse understands which of the following is implicated in the development of osteoporosis?
The nurse understands which of the following is implicated in the development of osteoporosis?
A patient taking raloxifene (Evista) reports experiencing hot flashes. How should the nurse respond?
A patient taking raloxifene (Evista) reports experiencing hot flashes. How should the nurse respond?
When educating a patient about taking calcium supplements, what advice should the nurse provide to enhance absorption?
When educating a patient about taking calcium supplements, what advice should the nurse provide to enhance absorption?
Which of the following laboratory values should the nurse monitor in a patient taking calcium supplements?
Which of the following laboratory values should the nurse monitor in a patient taking calcium supplements?
A patient with significant risk factors for osteoporosis is prescribed raloxifene (Evista). Which risk factors would make the nurse question the order? (Select all that apply.)
A patient with significant risk factors for osteoporosis is prescribed raloxifene (Evista). Which risk factors would make the nurse question the order? (Select all that apply.)
A patient with osteoporosis is prescribed alendronate (Fosamax). Which of the following pre-existing conditions would be a contraindication for this medication, requiring the nurse to consult the provider? (Select all that apply.)
A patient with osteoporosis is prescribed alendronate (Fosamax). Which of the following pre-existing conditions would be a contraindication for this medication, requiring the nurse to consult the provider? (Select all that apply.)
What is the rationale for avoiding alcohol in client instructions, while taking Nonbiologic DMARDs?
What is the rationale for avoiding alcohol in client instructions, while taking Nonbiologic DMARDs?
What nursing intervention is a priority for a patient taking Biologic DMARDs?
What nursing intervention is a priority for a patient taking Biologic DMARDs?
What client instruction is a must know for Biologic DMARDs?
What client instruction is a must know for Biologic DMARDs?
True or False: Biologic DMARDs can cause reactivation of latent TB.
True or False: Biologic DMARDs can cause reactivation of latent TB.
True or False: Biologic DMARDs are typically a weekly injection
True or False: Biologic DMARDs are typically a weekly injection
Which client instruction is important to report to the provider ASAP when taking Biologic DMARDs?
Which client instruction is important to report to the provider ASAP when taking Biologic DMARDs?
What is the correct Pharmacological Class for the Biologic DMARD etanercept.
What is the correct Pharmacological Class for the Biologic DMARD etanercept.
True or False: Nonbiologic DMARDs are pregnancy safe to take.
True or False: Nonbiologic DMARDs are pregnancy safe to take.
A patient has been prescribed raloxifene. Which health promotion instructions is MOST important? (Select all that apply)
A patient has been prescribed raloxifene. Which health promotion instructions is MOST important? (Select all that apply)
True or False: Alendronate is best taken with a full glass of water and sit/stand for 30
True or False: Alendronate is best taken with a full glass of water and sit/stand for 30
Flashcards
Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA)
An inflammatory, systemic, autoimmune disease primarily affecting synovial joints.
Disease-Modifying Antirheumatic Drugs (DMARDs)
Disease-Modifying Antirheumatic Drugs (DMARDs)
These drugs modify or slow down the progression of rheumatoid arthritis.
DMARD Use
DMARD Use
Decreasing joint inflammation and subsequent damage.
Methotrexate
Methotrexate
Signup and view all the flashcards
Nonbiologic DMARD administration
Nonbiologic DMARD administration
Signup and view all the flashcards
Biologic DMARDs
Biologic DMARDs
Signup and view all the flashcards
Etanercept (Enbrel)
Etanercept (Enbrel)
Signup and view all the flashcards
Etanercept: Avoid Live Vaccines
Etanercept: Avoid Live Vaccines
Signup and view all the flashcards
Osteoporosis
Osteoporosis
Signup and view all the flashcards
Selective Estrogen Receptor Modulators (SERMs)
Selective Estrogen Receptor Modulators (SERMs)
Signup and view all the flashcards
Bisphosphonates
Bisphosphonates
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
Calcium Supplements
Calcium Supplements
Signup and view all the flashcards
Normal Calcium Range
Normal Calcium Range
Signup and view all the flashcards
Bisphosphonates: Decrease Esophagitis
Bisphosphonates: Decrease Esophagitis
Signup and view all the flashcards
Calcium Supplements Use
Calcium Supplements Use
Signup and view all the flashcards
SERMs Side effects
SERMs Side effects
Signup and view all the flashcards
Gabapentin Use
Gabapentin Use
Signup and view all the flashcards
Study Notes
- The musculoskeletal system will be discussed with reference to the conditions rheumatoid arthritis and osteoporosis, as well as gabapentin.
- The musculoskeletal system is being covered in NU 307 Pharmacology at Endicott College.
Rheumatoid Arthritis
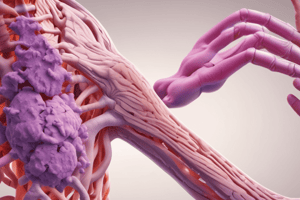
- Rheumatoid Arthritis (RA) is an inflammatory, systemic, autoimmune disease.
- RA primarily affects the synovial joints, but can occur anywhere connective tissue is widespread.
- RA causes joint stiffness, pain, swelling, and deformities.
- RA impacts mostly young to middle-aged women.
- RA is caused by environmental and genetic factors.
- The goal of drug therapy for RA is to decrease joint pain and inflammation.
- Symptoms of RA include pain and stiffness in more than one joint, morning joint stiffness, joint tenderness and swelling, decreased range of motion, fatigue/malaise, and low-grade fever.
Drug Therapy for RA
- Main drug categories for RA treatment include NSAIDs, glucocorticoids, and disease-modifying antirheumatic drugs (DMARDs).
- DMARDs are divided into two categories: nonbiologic (traditional) and biologic.
Nonbiologic DMARDs
- Nonbiologic DMARDs have an immunosuppressive effect by interfering with normal B and T lymphocytes activity.
- The common nonbiologic DMARD methotrexate (Rheumatrexate} is a folate antagonist with an antineoplastic therapeutic class.
- Nonbiologic DMARDs decrease joint inflammation and subsequent joint damage, and cause an immunosuppressive effect.
- Nonbiologic DMARDs can suppress bone marrow, making the patient more susceptible to infection.
- Monitor labs (RBC, WBC, platelets) for bone marrow suppression.
- A lot of ADR are caused by Nonbiologic DMARDs, like infection, liver damage, Gl ulcers, pulmonary fibrosis, and dizziness.
- Nursing interventions for nonbiologic DMARDs include monitoring for low platelets, RBC, and WBC; monitoring for signs and symptoms of infection; monitoring LFTs and observing for jaundice; monitoring for GI bleeding; monitoring for respiratory distress and decreased oxygen; and monitoring for abdominal pain and N/V/D.
- Nonbiologic DMARDs are administered orally, SC, or IM, once a week.
- Folic acid may also be taken to decrease toxicity.
- Instructions to give clients taking Nonbiologic DMARD include reporting abnormal bleeding, reporting signs/symptoms of infection immediately, avoiding alcohol, reporting jaundice/signs/symptoms of liver damage, reporting SOB or difficulty breathing, and drinking at least 2L per day for help.
- Contraindications for nonbiologic DMARDs: Pregnancy, renal insufficiency, and liver insufficiency or hepatitis.
- Precautions for Nonbiologic DMARDs include: peptic ulcers/ulcerative colitis, active infections, can affect digoxin, caffeine may reduce effectiveness, alcohol use will increase hepatotoxicity and risk for bleeding, and using with warfarin.
Biologic DMARDs
- Biologic DMARDs bind to tumor necrosis factor, which prevents attachment to the cells of joint tissue, preventing inflammation.
- The common biologic DMARD etanercept (Enbrel) is a TNF blocker (tumor necrosis factor) with an immunosuppressant therapeutic class.
- Biologic DMARDs are still for treat and decrease joint inflammation and cause immunosuppressive effects.
- Biologic DMARDs increases patient susceptibility to infection.
- Biologic DMARDs may cause reactivation of latent TB.
- A TB test should be administered prior to starting therapy.
- Patients should avoid live vaccines.
- Biologic DMARDs are typically given as a weekly injection.
- Nursing interventions for Biologic DMARDs (etanercept (Enbrel)) include assessing for infection before injection, monitoring for s/s during therapy, monitoring for skin reactions, monitoring for redness, warmth, and itching at the injection site, and monitoring for s/s of heart failure - cough, SOB, pink sputum, and high HR and BP.
- Biologic DMARDs are administered via SC injection.
- The injection site of Biologic DMARDs must be monitored after for redness, pain, and swelling.
- Instructions to give clients taking Biologic DMARD include reporting signs/symptoms of infection immediately, avoiding immunizations and live vaccines, reporting skin rashes ASAP, and reporting signs/symptoms of heart failure.
- Contraindications for Biologic DMARDs include active infections, hematologic disease, and malignancy.
- Precautions for Biologic DMARDs include autoimmune disorders, live vaccines, and heart failure.
- Interactions with Biologic DMARDs include chemotherapeutic drugs and live vaccines.
Goal of RA Therapy
- There is no cure for RA.
- The goals of RA therapy are to control disease activity, stop/slow further damage, and improve quality of life.
- Quality of life relates to pain, inflammation, stiffness, and complications.
- Only 66% of patients with rheumatoid arthritis are adherent to DMARDs.
- Nonadherence is associated with disease flares, increased disability, and health care costs in rheumatoid arthritis.
- Modifiable factors associated with adherence in rheumatoid arthritis are the patient-physician relationship, patients' beliefs about medications, knowledge about their disease, and self-efficacy.
Osteoporosis
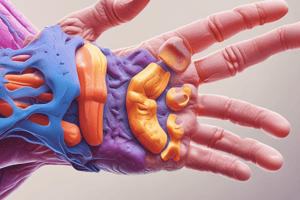
- Osteoporosis is a progressive disease resulting in reduced bone mass (through absorption), decreased bone density, and increased risk for fractures.
- Causes of osteoporosis include aging, menopause, overuse of alcohol, caffeine and tobacco, and long-term glucocorticoid therapy.
- The goal of drug therapy is to increase bone strength and decrease risk for fractures.
- There are four main drug categories to prevent or treat osteoporosis: Selective Estrogen Receptor Modulators (SERMs), Bisphosphonates, Calcitonin, and Calcium Supplements.
- Selective Estrogen Receptor Modulators (SERMs) activate estrogen receptors in tissue needed to decrease bone loss and increase bone density.
- Bisphosphonates inhibit osteoclasts and decrease bone resorption.
- Calcitonin decreases bone resorption by inhibiting osteoclasts.
- Calcium Supplements are a non-dietary source of calcium to promote bone growth.
Calcium Review
- Normal range for calcium is 9-11 mg/dL.
- Hypocalcemia is below 9 mg/dL.
- Hypercalcemia is above 11 mg/dL.
Selective Estrogen Receptor Modulators (SERMs)
- Common Drug: raloxifene (Evista)
- SERMs are used for the prevention or treatment of postmenopausal osteoporosis.
- SERMs are administered orally daily.
- SERMs increases the risk of DVT, pulmonary emboli, and stroke.
- Patients may report hot flashes (due to estrogen blockage in other tissues!).
- Intervene and educate about the risk for clots in the legs and lungs, and stroke.
- Legs: cramps, redness, swelling, warmth, unilateral
- Lungs: SOB, decreased oxygen saturation, difficulty breathing
- This is caused by an issue with hormone interference with FIBROGEN - so monitor RBC AND COAGS.
- SERMs Health Promotion includes consuming calcium and vitamin D, daily weight bearing (running, weights), using contraception to avoid getting pregnant, and reporting signs/symptoms of clots.
Bisphosphonates
- Common Drug: alendronate (Fosamax)
- Bisphosphonates are used for the prevention or treatment of postmenopausal or glucocorticoid-related osteoporosis.
- Bisphosphonates work by decreasing bone absorption/inhibiting osteoclasts. administer Bisphosphonates orally daily.
- Bisphosphonates should be taken with a full glass of water.
- The patient should remain upright and avoid eating/drinking or taking a calcium supplement for 30 minutes afterwards.
- Bisphosphonates may cause GI upset.
- Bisphosphonates mostly cause GI EFFECTS!, such as nausea, vomiting, ABD pain, and esophagitis.
- The risk of esophagitis can be decreased by staying straight 30 minutes and drinking with lots of water.
- Muscle and joint pain is also a side effect of bisphosphonates.
- If the patient has muscle and joint pain, they may need to stop or take pain medication.
- Monitor for decrease bone resorption to evaluate the medication effectivness.
- Bisphosphonates must be taken with full glass of water and the client must sit/stand for 30 minutes with the drug as it can't be taken with Calcium supplement or antacid.
- Contraindications: Pt already as esophageal strictures, or other disorders calcium inhibits drugs absorption, so don't give within 30 minutes of administration!
Calcitonin
- Common Drug: calcitonin-salmon (Calcimar/Miacalcin)
- Calcitonin is used for the treatment of established postmenopausal osteoporosis or hypercalcemia related to hyperparathyroidism.
- Calcitonin is administered intranasally or as an injection.
- Calcitonin should be avoided in patients with a salmon or other fish protein allergy- anaphylactic reaction. Watch for hypocalcemia when adminstering Calcitonin.
Calcium Supplements
- Common Drug: citrate (Citracal), calcium carbonate (Tums)
- Calcium Supplements are used for the treatment of hypocalcemia, or for osteoporosis prevention in conjunction with another medication.
- Calcium Supplements administered orally - often with vitamin D.
- Watch for hypercalcemia – nausea, vomiting, constipation and monitor for signs of kidney stones.
Gabapentin
- Gabapentin (Neurontin) takes aim at the dysfunctional release of pain-controlling neurotransmitters, decreasing or stabilizing irritated nerve membranes to soften their response.
Connection Check Questions and Answers
- The nurse anticipates which follow-up test after a postmenopausal woman presents with a tibial fracture confirmed by x-ray? D. DEXA scan. Rationale: Use a DEXA scan to check for bone density problems due to loss of estrogen due to menopause, which is implicated in increased fracture risk.
- What are the most important supplements for bone health for patients of advancing age? A. Calcium and vitamin D. Rationale: Adequate calcium levels are associated with bone health. Vitamin D aids in the Gl absorption of calcium.
- The nurse knows that a decrease in estrogen levels is implicated in the development of osteoporosis. Rationale: A decrease in estrogen levels inhibits bone formation. Calcitonin decreases osteoclastic activity. Decreases in parathyroid hormone would decrease osteoclastic activity. A decrease in phosphorus levels is inversely proportional to an increase in calcium levels.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.