Podcast
Questions and Answers
What are the two types of implant supported fixed prostheses?
What are the two types of implant supported fixed prostheses?
- subperiosteal and transosteal
- endosteal and subperiosteal
- submucosal and endosteal
- transosteal and endosteal (correct)
The success of an implant depends on the quality of bone.
The success of an implant depends on the quality of bone.
True (A)
Which of the following is NOT a contraindication for implants?
Which of the following is NOT a contraindication for implants?
- Systemic illness
- Lack of operator experience
- Pregnancy
- Good oral hygiene (correct)
What type of implant is used for partially edentulous patients?
What type of implant is used for partially edentulous patients?
What is the most important factor to consider when placing an implant?
What is the most important factor to consider when placing an implant?
What is the minimum distance between two implants?
What is the minimum distance between two implants?
What is the minimum distance between an implant and a natural tooth?
What is the minimum distance between an implant and a natural tooth?
A healing cap is used to protect the implant during the healing process.
A healing cap is used to protect the implant during the healing process.
What is the material of choice currently for implants?
What is the material of choice currently for implants?
Implants can be threaded or non-threaded.
Implants can be threaded or non-threaded.
What is the process of direct attachment and connection of osseous tissues to an implant?
What is the process of direct attachment and connection of osseous tissues to an implant?
A threaded implant provides better stability in the bone.
A threaded implant provides better stability in the bone.
What is the purpose of a radiographic reference stent?
What is the purpose of a radiographic reference stent?
What is the purpose of probing during implant planning?
What is the purpose of probing during implant planning?
The healing screw is placed at the end of the first stage surgery.
The healing screw is placed at the end of the first stage surgery.
What is the purpose of the healing abutment?
What is the purpose of the healing abutment?
Which of the following is NOT an advantage of screw-retained abutments?
Which of the following is NOT an advantage of screw-retained abutments?
Which of the following is a contraindication for cement-retained abutments?
Which of the following is a contraindication for cement-retained abutments?
Angled abutments can be used to correct angulation problems for esthetic purposes.
Angled abutments can be used to correct angulation problems for esthetic purposes.
Wide-based abutments allow teeth with larger cross sections to be restored.
Wide-based abutments allow teeth with larger cross sections to be restored.
UCLA abutments have a one-piece prosthetic component.
UCLA abutments have a one-piece prosthetic component.
Computer-generated abutments are custom made by CAD-CAM systems
Computer-generated abutments are custom made by CAD-CAM systems
The success of an implant restoration depends on the skill of the surgical procedure
The success of an implant restoration depends on the skill of the surgical procedure
The transfer coping is used to create an impression of the implant with the cast
The transfer coping is used to create an impression of the implant with the cast
The laboratory analogue represents the implant fixture for the impression
The laboratory analogue represents the implant fixture for the impression
Distal extension implant restoration is ideal for a completely edentulous arch
Distal extension implant restoration is ideal for a completely edentulous arch
What are the benefits of hybrid prostheses?
What are the benefits of hybrid prostheses?
Occlusion is important for implant success because it minimizes damaging forces on the implant-bone interface
Occlusion is important for implant success because it minimizes damaging forces on the implant-bone interface
Excessive occlusal forces can cause bone loss
Excessive occlusal forces can cause bone loss
The use of multiple implants helps to distribute forces evenly across the implant-bone interface
The use of multiple implants helps to distribute forces evenly across the implant-bone interface
Connecting implants to natural teeth is a concern because of the difference in mobility between the two
Connecting implants to natural teeth is a concern because of the difference in mobility between the two
Which of the following is NOT a common complication of implants?
Which of the following is NOT a common complication of implants?
What is the most common cause of implant failure?
What is the most common cause of implant failure?
Flashcards
Implant
Implant
An alloplastic material embedded in oral tissues to support dental prosthetics.
Osseointegration
Osseointegration
The process of bone integrating directly with an inert implant material, vital for stability.
Indication for Implants
Indication for Implants
Criteria for implant application, such as missing single tooth or long edentulous span.
Contraindications for Implants
Contraindications for Implants
Signup and view all the flashcards
Endosteal Implant
Endosteal Implant
Signup and view all the flashcards
Two-stage Implant Procedure
Two-stage Implant Procedure
Signup and view all the flashcards
C.T Scan in Implant Planning
C.T Scan in Implant Planning
Signup and view all the flashcards
Bone Sounding
Bone Sounding
Signup and view all the flashcards
Soft Tissue Contours
Soft Tissue Contours
Signup and view all the flashcards
Single Tooth Implant
Single Tooth Implant
Signup and view all the flashcards
Healing Cap
Healing Cap
Signup and view all the flashcards
Abutment
Abutment
Signup and view all the flashcards
Occlusion
Occlusion
Signup and view all the flashcards
Implant Mobility Check
Implant Mobility Check
Signup and view all the flashcards
Bone Loss
Bone Loss
Signup and view all the flashcards
Prosthetic Failure
Prosthetic Failure
Signup and view all the flashcards
Screw-retained Abutments
Screw-retained Abutments
Signup and view all the flashcards
Cement-retained Abutments
Cement-retained Abutments
Signup and view all the flashcards
Tilted Implants
Tilted Implants
Signup and view all the flashcards
Diagnostic Cast Examination
Diagnostic Cast Examination
Signup and view all the flashcards
Prosthodontic Failure
Prosthodontic Failure
Signup and view all the flashcards
Telescopic Copings
Telescopic Copings
Signup and view all the flashcards
Hydroxyapatite Coating
Hydroxyapatite Coating
Signup and view all the flashcards
Implant Size Criteria
Implant Size Criteria
Signup and view all the flashcards
Maxillary Sinus Consideration
Maxillary Sinus Consideration
Signup and view all the flashcards
Recall Visits for Maintenance
Recall Visits for Maintenance
Signup and view all the flashcards
Cutting and Splinting during Surgery
Cutting and Splinting during Surgery
Signup and view all the flashcards
Implant Planning Process
Implant Planning Process
Signup and view all the flashcards
Patient Education
Patient Education
Signup and view all the flashcards
Study Notes
Implant Supported Fixed Prosthesis
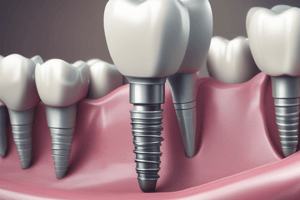
- Alloplastic material is implanted beneath the oral tissues (mucosal/periosteal layer) and/or within the bone to provide retention and support for a fixed or removable prosthesis.
- Devices are inserted into or onto bone to replace missing teeth.
- Alloplastic materials originate from non-living sources to surgically replace missing tissue or augment remaining tissue.
- Osseointegration is the process of direct attachment and connection of osseous tissues to an inert alloplastic material without intervening fibrous soft tissues.
Indications
- Missing single tooth in an intact dentition
- Long edentulous span
- Inability to create a fixed partial denture (FPD) or removable partial denture (RPD).
- Unfavorable number or location of natural abutments
Contraindications
- Systemic illnesses
- Radiation therapy to the implant site
- Lack of patient motivation
- Patient inexperience
- Pregnancy
- Uncontrolled metabolic disease
- Unrealistic patient expectations
Advantages (Surgical)
- Documented success rate
- Precise implant site preparation
- Reversibility in case of implant failure
- Multiple restorative options (screw-retained or cement-retained).
- Versatility of second-stage components
- Retrievability in case of prosthodontic failure
Advantages (Prosthetic)
- In-office procedure
- Adaptable to multiple intraoral locations
- Angle correction
- Aesthetics
- Crown contours
Implant Classifications (by position)
- Subperiosteal: Supported by bone under the mucosal layer, used for complete dentures.
- Transosteal: Passes through the bone used for complete dentures.
- Endosteal: Placed within the jawbone, useful for both partial and complete dentures.
Implant Classifications (by form)
- Blade: Wedge or rectangular shaped implant
- Root/Cylindrical: Direct connection with bone ("osseointegration"), has a diameter of 3-6 mm and length of 8-20 mm, often with external threads
Surgical Procedures (based on implant integration)
- One-stage implant: Implant is placed in bone, immediately projects through the mucosa into oral cavity.
- Two-stage implant: Fixture placed in the bone, oral mucosa is sutured over the implant for a healing period (3 months for mandible, 6 months for maxilla). In the second surgery, mucosa is reflected and an extension collar/healing cap is fixed firmly to the implant.
Implant Materials
- Metallic Implants: Titanium, titanium alloy (common choice for whole implant systems, can be threaded or non-threaded).
- Surface treatment (grit-blasted, acid-etched): Increases surface area for bone contact.
Clinical Examination & Implant Treatment Planning
- Determine sufficient bone quantity and quality
- Identify anatomical structures & flabby tissues.
- Panoramic radiographs: Crucial for visualization of vital structures (maxillary sinus) and allowing for magnification control.
- Periapical radiographs: Evaluate implant placement areas
- Cephalometric radiographs: Assess bone width in anterior and posterior maxilla/mandible regions.
- CBCT scans: Visualize maxillary sinus, inferior alveolar canals, & other vital structures.
Restorative Considerations
- Implants should be placed entirely within bone, avoiding anatomical features.
- Ideal vertical bone thickness: 10 mm, ideal horizontal thickness: 6 mm.
- Considerations for sufficient space (1-3 mm) between implants and teeth/adjacent implants
Clinical Implant Components
- Implant Body/Fixture Body: Placed in the bone, contains internally threaded portion to accept second-stage components.
- Healing Screw/Cover Screw: Screwed over the implant body after surgery to cover the implant surface and manage bone/soft tissue integration
- Healing Cap & Healing Abutment: dome-shaped component (2-10mm) that projects through the soft tissue; enables tissue healing after placement of the implant.
- Abutment: component that connects the implant to the restoration; made from titanium, titanium alloys, or zirconium; screw retained or cement retained.
Implant types
- Screw-retained "standard" abutments: Used where retrievability is critical; involve two screws to connect the abutment to the implant and restoration, resulting in supra-gingival (above gum) or sub-gingival (below gum) lengths to suit the case.
- Cement-retained "fixed" abutments: Retained by cement to support the restoration; typically have a smooth, polished, and straight-sided finish to mimic natural teeth; requires a temporary cement for allowing for retrievability
Indications for Angled and Tapered Abutments
- Corrective of angular issues or esthetic/biomechanical concerns
- Improve aesthetics
- Facilitate oral hygiene
- Minimize harm to existing anatomical structures
Non-segmented/UCLA Abutments
- One-piece prosthetic component which means the restorations are directly placed on the implant (without additional parts needing connection) this is useful in cases of limited interarch distance or minimal soft tissue thickness
Implant Restorative Options (for various situations):
- Single tooth implants: Restore individual missing teeth, emphasis on esthetics.
- Multiple implants: For long edentulous spans where one or more teeth are missing; often create a fixed bridge (FPD) supported by the implants.
- Full arch restorations: Utilize multiple implants to replace all teeth; often combined with a FPD bridge structure.
Implant restoration maintenance
- Post-surgical visits (typically every 3 months during the first year).
- Oral hygiene instructions
- Evaluation of implant mobility, framework, and occlusion
Complications
- Bone loss (exceeding 0.2mm/year is a concern - factors: implant size, shape, amount of bone, or occlusal forces).
- Prosthetic component failure: Fatigue from biomechanical overload.
Systemic Factors Influencing Implant Success
- Patients with certain systemic health conditions like tobacco use or diabetes require extra care, as these affect healing and implant success.
- Inadequate oral hygiene is an important negative factor
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.