Podcast
Questions and Answers
Which of the following cells are known to display MHC II molecules?
Which of the following cells are known to display MHC II molecules?
- Neutrophils
- Helper T cells (correct)
- B cells (correct)
- Cytotoxic T cells
What role does C3b play in the immune system?
What role does C3b play in the immune system?
- Anaphylatoxin
- Chemotactic factor
- Opsonin (correct)
- Cytotoxic agent
Which immune cells are primarily responsible for combating parasitic infections?
Which immune cells are primarily responsible for combating parasitic infections?
- Neutrophils
- Basophils
- Eosinophils (correct)
- Mast cells
What is the effect of a deficiency in extravasation of white blood cells?
What is the effect of a deficiency in extravasation of white blood cells?
Which type of hypersensitivity is directly linked to the action of basophils and mast cells?
Which type of hypersensitivity is directly linked to the action of basophils and mast cells?
What molecules do helper T cells display on their surface?
What molecules do helper T cells display on their surface?
Which of the following best describes the function of eosinophils?
Which of the following best describes the function of eosinophils?
Which immune response pathway involves C3 convertases?
Which immune response pathway involves C3 convertases?
What is the role of opsonins in phagocytosis?
What is the role of opsonins in phagocytosis?
Which statement about the complement system's split-products is incorrect?
Which statement about the complement system's split-products is incorrect?
Natural defense mechanisms include all the following except:
Natural defense mechanisms include all the following except:
Which statement accurately differentiates between acquired immune responses and innate immunity?
Which statement accurately differentiates between acquired immune responses and innate immunity?
What component is crucial for enabling white blood cells to exit the bloodstream?
What component is crucial for enabling white blood cells to exit the bloodstream?
Among these immune cells, which one primarily functions as a major phagocyte?
Among these immune cells, which one primarily functions as a major phagocyte?
Which class of antibodies is produced during humoral adaptive immunity?
Which class of antibodies is produced during humoral adaptive immunity?
Which of the following statements regarding lymphocyte characteristics is correct?
Which of the following statements regarding lymphocyte characteristics is correct?
Which of the following components is associated with anaphylatoxic activity in the immune system?
Which of the following components is associated with anaphylatoxic activity in the immune system?
Which of the following is NOT a characteristic of opsonins?
Which of the following is NOT a characteristic of opsonins?
What is a primary function of the complement system's MAC complex?
What is a primary function of the complement system's MAC complex?
What distinguishes the classic pathway of complement activation?
What distinguishes the classic pathway of complement activation?
Which natural defense mechanism provides the first line of protection against pathogens?
Which natural defense mechanism provides the first line of protection against pathogens?
Which immune cells primarily mediate the response to allergens through IgE?
Which immune cells primarily mediate the response to allergens through IgE?
Which of the following describes a role of the acidic pH in natural defense mechanisms?
Which of the following describes a role of the acidic pH in natural defense mechanisms?
In the context of white blood cell function, what does extravasation specifically enable?
In the context of white blood cell function, what does extravasation specifically enable?
Which feature best differentiates acquired immune responses from innate immunity?
Which feature best differentiates acquired immune responses from innate immunity?
Which of the following lymphocytes is primarily involved in humoral adaptive immunity?
Which of the following lymphocytes is primarily involved in humoral adaptive immunity?
What is the primary role of histamine released by basophils and mast cells?
What is the primary role of histamine released by basophils and mast cells?
Which complement component is both anaphylatoxic and chemotactic for neutrophils?
Which complement component is both anaphylatoxic and chemotactic for neutrophils?
Which type of immunity involves specific antigen receptors and has memory?
Which type of immunity involves specific antigen receptors and has memory?
Which immune cell type primarily contributes to the innate immune response?
Which immune cell type primarily contributes to the innate immune response?
What is the primary function of opsonins in the immune response?
What is the primary function of opsonins in the immune response?
Which lymphocyte subset displays CD4 molecules and plays a key role in regulating immune responses?
Which lymphocyte subset displays CD4 molecules and plays a key role in regulating immune responses?
What deficiency may lead to a decreased ability to leave blood vessels during an immune response?
What deficiency may lead to a decreased ability to leave blood vessels during an immune response?
What is the role of lysozyme in the body's defense mechanisms?
What is the role of lysozyme in the body's defense mechanisms?
In the context of complement pathways, which component acts as a convertase in the alternative pathway?
In the context of complement pathways, which component acts as a convertase in the alternative pathway?
Study Notes
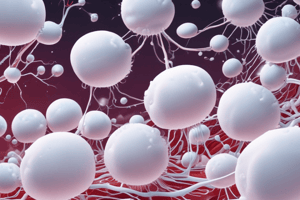
Lymphocytes
- Natural Killer (NK) cells: Innate immune lymphocytes without antigen-specific receptors
- B cells: Display B-cell receptors (BCR) on their surface. Express both MHC I and MHC II molecules.
- Cytotoxic T cells: Display T-cell receptors (TCR) and CD8 molecules on their surface.
- Helper T cells: Display TCR and CD4 molecules on their surface.
MHC I and MHC II
- MHC I: Present on all nucleated cells.
- MHC II: Present on B cells, macrophages, and dendritic cells.
Basophils and Mast Cells
- Release histamine and other inflammatory mediators.
- Involved in type I hypersensitivity reactions like allergies.
Eosinophils
- Primarily involved in anti-parasitic immunity.
Neutrophils
- Part of innate immunity.
- Most abundant white blood cell (WBC).
- Major phagocytes.
Extravasation
- Process that allows WBCs to leave blood vessels and enter tissues.
- Deficiencies in extravasation increase susceptibility to bacterial infections.
Opsonization and Phagocytosis:
- Opsonization: Process of coating pathogens with opsonins to enhance phagocytosis.
- Innate Immunity Opsonins: C3b, C4b (complement components), C-reactive protein (CRP) produced by hepatocytes.
- Adaptive Immunity Opsonin: IgG antibody.
Immune System Benefits and Harmful Effects
- Benefits: Defends against pathogens, removes damaged cells, contributes to tissue repair.
- Harmful Effects: Autoimmune diseases (attacks own body), allergies, transplant rejection.
Complement System Split-Products
- C3a and C5a: Anaphylatoxins (induce mast cell degranulation and inflammation).
- C3b and C4b: Opsonins (enhance phagocytosis).
- C5a: Also a chemotactic factor (attracts neutrophils).
- C5b: Component of the membrane attack complex (MAC).
- MAC (C5b678(9)6): Final product of the complement cascade, forms a pore in target cells.
Complement Pathways:
- Classic Pathway: Activated by antigen-antibody complexes.
- Alternative Pathway: Activated by bacterial surfaces.
- C3 Convertases: Enzymes that cleave C3 into C3a and C3b.
- Classic Pathway C3 Convertase: C4b2a
- Alternative Pathway C3 Convertase: C3bBb
- C5 Convertases: Enzymes that cleave C5 into C5a and C5b.
- Classic Pathway C5 Convertase: C4b2a3b
- Alternative Pathway C5 Convertase: C3bBb3b
Activators of Complement Pathways:
- Classic Pathway: Antigen-antibody complexes, certain viral and bacterial components.
- Alternative Pathway: Microbial surfaces (lipopolysaccharides), certain immune complexes.
B Cell Development and Activation
- Antigen-independent processes: Proliferation, differentiation of B cells into different sub-types, creating a diverse pool of B cells.
- Antigen-dependent processes: Clone selection (specific B cell recognizing antigen is activated), proliferation of that specific B cell clone, and differentiation into plasma cells (produce antibodies) and memory cells (provide long-term immunity).
Natural Defense Mechanisms
- Physical barriers: Skin, mucous membranes, and cilia.
- Chemical barriers: Acidic pH of the stomach, Lysozyme (enzyme breaking down bacterial cell walls), antimicrobial peptides.
- Microflora: Beneficial bacteria compete with pathogens.
Comparing Innate and Adaptive Immunity
- Innate Immunity:
- First line of defense.
- No antigen-specific receptors (uses pattern recognition receptors to recognize broad patterns).
- Rapid response.
- No memory.
- Adaptive Immunity:
- Specific response to pathogens.
- Antigen-specific receptors (BCRs and TCRs).
- Slower initial response but develops memory.
Humoral and Cell-Mediated Immunity:
- Humoral Immunity:
- Mediated by antibodies produced by B cells.
- Targets extracellular pathogens.
- Key antibody: IgG, produced by plasma cells.
- Cell-mediated Immunity:
- Mediated by T cells (cytotoxic T cells and helper T cells).
- Targets intracellular pathogens, viruses, cancer cells.
- Cytotoxic T cells (Tc): Directly kill infected cells.
- Helper T cells (Th): Help activate other immune cells (B cells and macrophages).
Lymphocytes
- Natural Killer (NK) cells are lymphocytes with no antigen-specific receptor, belonging to the innate immune system.
- B cells display B cell receptors (BCR) on their surface, and express both MHC I and MHC II.
- Cytotoxic T cells express T cell receptors (TCR) and CD8 molecules on their surface.
- Helper T cells express TCR and CD4 molecules on their surface.
MHC
- MHC I is expressed by all nucleated cells.
- MHC II is present on B cells, macrophages, and dendritic cells.
Other Immune Cells
- Basophils and mast cells degranulate in response to IgE binding, releasing histamine and other inflammatory mediators. This is involved in Type I hypersensitivity reactions.
- Eosinophils are important for anti-parasitic activity.
- Neutrophils are the most common white blood cells, are part of the innate immune system, and are major phagocytes.
Extravasation and Opsonization
- Extravasation is the process by which white blood cells leave blood vessels. Its deficiency results in increased susceptibility to bacterial infections.
- Opsonization enhances phagocytosis by coating microbes with opsonins.
- Innate immunity opsonins: C3b, C4b (complement components), C-reactive protein (CRP; produced by hepatocytes)
- Adaptive immunity opsonin: IgG
Immune System Benefits and Harmful Effects
- Benefits: Protection against pathogens, removal of damaged cells, removal of cancerous cells.
- Harmful effects: Allergies, autoimmune diseases, graft rejection.
Complement System
- Split-products of complement:
- C3a is ananaphylatoxin, stimulating mast cell degranulation.
- C3b and C4b are opsonins.
- C5a is an anaphylatoxin and chemotactic for neutrophils.
- C5b is a component of the membrane attack complex (MAC).
- MAC (C5b678(9)n) is the final product of the complement cascade, forming a pore in the target cell membrane.
Complement Pathways
- Classic pathway: Activated by antigen-antibody complexes (immune complexes).
- Alternative pathway: Activated by microbial surface components.
- C3 convertases: Cleave C3, generating C3a and C3b.
- Classic pathway C3 convertase: C4b2a
- Alternative pathway C3 convertase: C3bBb
- C5 convertases: Cleave C5, generating C5a and C5b.
- Classic pathway C5 convertase: C4b2a3b
- Alternative pathway C5 convertase: C3bBb3b
B cell Development
- Antigen-independent processes:
- Clone selection: B cells with unique BCRs are generated in the bone marrow.
- Proliferation: B cells clone and expand when they recognize self-antigens.
- Antigen-dependent processes:
- Ag specificity: BCR specificity to specific epitope.
- Clonal selection: B cells with specific BCRs are activated and proliferate upon antigen encounter.
Natural Defense Mechanisms
- Innate immunity:
- Acidic pH of the stomach
- Skin
- Lysozyme
- Microflora
- Enzymes
Innate vs. Adaptive Immunity
| Feature | Innate Immunity | Adaptive Immunity |
|---|---|---|
| Ag-receptors | Pattern Recognition Receptors (PRRs) | Antigen-specific receptors (BCRs, TCRs) |
| Specificity | Limited | Highly specific |
| Memory | No | Yes |
Adaptive Immunity
- Humoral adaptive immunity:
- Mediated by antibodies produced by B cells.
- IgG is a major antibody isotype, produced by plasma cells (differentiated B cells).
- Cell-mediated adaptive immunity:
- Mediated by cytotoxic T cells (Tc) and helper T cells.
- Tc cells directly kill infected or cancerous cells.
- Helper T cells activate other immune cells, including B cells and Tc cells.
Lymphocytes
- Natural Killer (NK) cells: Innate immunity lymphocytes that lack antigen-specific receptors.
- B cells: Display B cell receptors (BCR) on their surface. Express both MHC I and MHC II.
- Cytotoxic T cells (CTL): Express T cell receptors (TCR) and CD8 molecules on their surface.
- Helper T cells: Express TCR and CD4 molecules on their surface.
Major Histocompatibility Complex (MHC)
- MHC I: Present on all nucleated cells.
- MHC II: Present on B cells, macrophages, and dendritic cells.
Immune Cells
- Basophils and mast cells: Involved in type I hypersensitivity reactions. Degranulate in response to IgE, releasing histamine and other effectors.
- Eosinophils: Primarily involved in anti-parasitic activity.
- Neutrophils: Most abundant white blood cell (WBC) in the body. Play a major role in innate immunity as phagocytes.
Extravasation
- Enables WBCs to leave blood vessels.
- Deficiency in extravasation increases susceptibility to bacterial infections.
Opsonization
- Innate Immunity Opsonins:
- C3b and C4b (complement components)
- C-reactive protein (CRP) (produced by hepatocytes)
- Adaptive Immunity Opsonin:
- IgG
Immune System Benefits and Harmful Effects
- Benefits: Protects against pathogens, eliminates damaged cells, and promotes tissue repair.
- Harmful Effects: Can cause autoimmune diseases and allergies.
Complement System
- Functions of Complement Split Products:
- C3a and C5a: Anaphylatoxins (trigger inflammation)
- C3b and C4b: Opsonins (facilitate phagocytosis)
- C5a: Chemotactic for neutrophils (attracts them to the site of infection)
- C5b: Component of the Membrane Attack Complex (MAC)
- MAC (C5b678(9)6): Final product of the complement cascade, forms pores in target cell membranes.
Complement Pathways
- C3 Convertases:
- Alternative Pathway: C3bBb
- Classic Pathway: C4b2a
- C5 Convertases:
- Alternative Pathway: C3bBbC3b
- Classic Pathway: C4b2a3b
Complement Activator
- Classic Pathway:
- Antigen-antibody immune complexes
- Alternative Pathway:
- Microbial surfaces (lipopolysaccharide)
- C-reactive protein
B Cell Development
- Antigen-Independent Processes:
- Clone selection: B cells with specific BCRs are selected for survival and proliferation.
- Proliferation: Selected B cells multiply to create a large population.
- Antigen-Dependent Processes:
- Antigen specificity: B cells with BCRs that bind to a specific antigen are activated.
Natural Defense Mechanisms
- First Line of Defense:
- Acidic pH of the stomach: Inhibits bacterial growth.
- Skin: Physical barrier against pathogens.
- Lysozyme: Enzyme found in tears and saliva that breaks down bacterial cell walls.
- Microflora: Beneficial bacteria that compete with pathogens.
- Other enzymes: Contribute to the breakdown of pathogens.
Acquired vs. Innate Immunity
| Feature | Acquired Immunity | Innate Immunity |
|---|---|---|
| Antigen Receptors | Specific receptors (TCR, BCR) | Pattern Recognition Receptors (PRRs) |
| Specificity | Highly specific to particular antigens | Broadly specific to pathogen associated molecular patterns (PAMPs) |
| Memory | Develops long-lasting memory to previously encountered antigens | No memory |
Humoral and Cell-mediated Immunity
- Humoral Adaptive Immunity:
- IgG: Most abundant antibody in serum, produced by plasma cells.
- Cell-mediated Adaptive Immunity:
- Tc (Cytotoxic T cells): Kill infected cells directly.
- T helper cells: Support other immune cells (B cells, macrophages, etc.) .
Lymphocytes
- Natural Killer (NK) cells are lymphocytes that lack antigen-specific receptors. They are part of the innate immune system.
- B cells display B cell receptors (BCR) on their surface. They possess both MHC I and MHC II.
- Cytotoxic T cells display T cell receptors (TCR) and CD8 molecules on their surface.
- Helper T cells display TCR and CD4 molecules on their surface.
Major Histocompatibility Complex (MHC)
- All nucleated cells express MHC I.
- MHC II is present on B cells, macrophages, and dendritic cells.
White Blood Cells (WBCs)
- Basophils and mast cells release histamine and other effectors upon degranulation triggered by IgE. They are involved in Type I hypersensitivity reactions.
- Eosinophils play a role in antiparasitic activity.
- Neutrophils are the most common WBCs. They participate in innate immunity and are major phagocytes.
Extravasation and Phagocytosis
- Extravasation allows WBCs to leave blood vessels. Its deficiency increases susceptibility to bacterial infections.
- Opsonization enhances phagocytosis.
- Opsonins are molecules that coat pathogens, making them more attractive to phagocytes.
- Innate Immunity Opsonins: C3b, C4b (Complement), CRP (produced by hepatocytes)
- Adaptive Immunity Opsonin: IgG
Immune System Functions
- The immune system offers protection from pathogens but can also cause harmful effects, such as autoimmune diseases.
Complement System
- Split-products of complement have distinct functions:
- C3a and C5a are anaphylatoxins, triggering mast cell degranulation.
- C3b and C4b serve as opsonins.
- C5a is also chemotactic for neutrophils.
- C5b is a component of the membrane attack complex (MAC).
- MAC (C5b678(9)6) is the final product of the complement cascade.
Complement Pathways
- C3 convertases are key enzymes in the classical and alternative pathways of complement activation:
- Classical pathway C3 convertase: C4b2a
- Alternative pathway C3 convertase: C3bBb
- C5 convertases are responsible for cleaving C5, a vital step in MAC formation:
- Classical pathway C5 convertase: C4b2a3b
- Alternative pathway C5 convertase: C3bBb3b
Complement Activation
- Classic pathway is activated by antigen-antibody complexes.
- Alternative pathway is triggered by microbial surfaces and other molecules.
B Cell Development
- B cell development involves both antigen-dependent and antigen-independent processes:
- Antigen-independent processes: include clone selection and proliferation.
- Antigen-dependent processes: determine antigen specificity.
Natural Defense Mechanisms
- Natural defense mechanisms provide the first line of defense against pathogens:
- Acidic pH of the stomach
- Skin
- Lysozyme
- Microflora
- Enzymes
Comparing Innate and Acquired Immunity
- Innate immunity is the first line of defense. It is non-specific and lacks memory. It relies on pattern recognition receptors (PRRs) to recognize pathogens.
- Acquired immunity is specific, adaptable, and has memory. It relies on antigen receptors (BCR and TCR) to recognize specific antigens.
Adaptive Immunity
- Humoral adaptive immunity involves the production of antibodies (e.g., IgG) by plasma cells.
- Cell-mediated adaptive immunity is mediated by cytotoxic T cells (Tc) and helper T cells, which directly kill infected cells or help other immune cells.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the various types of lymphocytes and their functions in the immune system, including Natural Killer cells, B cells, Cytotoxic T cells, and more. This quiz covers the roles of MHC molecules, basophils, eosinophils, neutrophils, and the process of extravasation in immune responses.