Podcast
Questions and Answers
What may be present in acute myocarditis?
What may be present in acute myocarditis?
- Mural thrombus (correct)
- Murine thrombosis
- Myocardial infarction
- Necrosis
What may cause myocardial disease?
What may cause myocardial disease?
- Nutritional deficiencies
- Viral infections
- Drugs and certain hormones (correct)
- Bacterial infections
What is characterized by edema, interstitial lymphocytic infiltrates, and myocyte injury?
What is characterized by edema, interstitial lymphocytic infiltrates, and myocyte injury?
- Myocardial infarction
- Acute myocarditis (correct)
- Chronic myocarditis
- Cardiotoxicity
What is a complication of cancer therapy?
What is a complication of cancer therapy?
What is often associated with cardiac complications of cancer therapy?
What is often associated with cardiac complications of cancer therapy?
What is a feature of advanced stages of myocardial disease?
What is a feature of advanced stages of myocardial disease?
What is a characteristic of myocardial disease?
What is a characteristic of myocardial disease?
What may be seen in the heart in acute myocarditis?
What may be seen in the heart in acute myocarditis?
What is the primary consequence of inadequate cardiac output in right-sided heart failure?
What is the primary consequence of inadequate cardiac output in right-sided heart failure?
What is the main reason for dyspnea on exertion in patients with right-sided heart failure?
What is the main reason for dyspnea on exertion in patients with right-sided heart failure?
What is the pathophysiological mechanism underlying orthopnea in right-sided heart failure?
What is the pathophysiological mechanism underlying orthopnea in right-sided heart failure?
What is the consequences of backward failure in right-sided heart failure?
What is the consequences of backward failure in right-sided heart failure?
What is the compensatory mechanism that occurs once right-sided heart failure appears?
What is the compensatory mechanism that occurs once right-sided heart failure appears?
What is the primary symptom of right-sided heart failure?
What is the primary symptom of right-sided heart failure?
What is the effect of right-sided heart failure on the diaphragm?
What is the effect of right-sided heart failure on the diaphragm?
What is the pathophysiological consequence of increased end-diastolic ventricular pressures in right-sided heart failure?
What is the pathophysiological consequence of increased end-diastolic ventricular pressures in right-sided heart failure?
In the provided text, what is the primary reason for the cross-reactive immune response mentioned?
In the provided text, what is the primary reason for the cross-reactive immune response mentioned?
What is the primary cause of restrictive cardiomyopathy, according to the provided text?
What is the primary cause of restrictive cardiomyopathy, according to the provided text?
What is the primary location of the fibrosis in endomyocardial fibrosis, as described in the text?
What is the primary location of the fibrosis in endomyocardial fibrosis, as described in the text?
Which of the following is NOT a potential cause of myocarditis, as mentioned in the text?
Which of the following is NOT a potential cause of myocarditis, as mentioned in the text?
Which of the following conditions is described as a non-viral cause of myocarditis in the text?
Which of the following conditions is described as a non-viral cause of myocarditis in the text?
The text suggests that endomyocardial fibrosis is prevalent in which geographical region?
The text suggests that endomyocardial fibrosis is prevalent in which geographical region?
Based on the text, what is the most common type of restrictive cardiomyopathy?
Based on the text, what is the most common type of restrictive cardiomyopathy?
The text mentions that endomyocardial fibrosis often involves which specific structures of the heart?
The text mentions that endomyocardial fibrosis often involves which specific structures of the heart?
Which of the following can cause a reduction in arterial contribution to ease progression?
Which of the following can cause a reduction in arterial contribution to ease progression?
What is the outcome of decompensated heart failure on the renin-angiotensin-aldosterone system?
What is the outcome of decompensated heart failure on the renin-angiotensin-aldosterone system?
What is the effect of reduced renal perfusion on the heart?
What is the effect of reduced renal perfusion on the heart?
Which of the following can lead to increased norepinephrine release by the adrenal glands?
Which of the following can lead to increased norepinephrine release by the adrenal glands?
What is the outcome of increased sympathetic nervous system activity on the heart?
What is the outcome of increased sympathetic nervous system activity on the heart?
Which of the following can lead to pulmonary edema?
Which of the following can lead to pulmonary edema?
What is the effect of reduced ventricular stroke volume on the heart?
What is the effect of reduced ventricular stroke volume on the heart?
Which of the following can lead to cardiac complications?
Which of the following can lead to cardiac complications?
What is a common consequence of left-sided heart failure?
What is a common consequence of left-sided heart failure?
Which condition is typically associated with congestive heart failure?
Which condition is typically associated with congestive heart failure?
What primarily causes increased tissue demands leading to left-sided heart failure?
What primarily causes increased tissue demands leading to left-sided heart failure?
What is one of the early signs of left-sided heart failure?
What is one of the early signs of left-sided heart failure?
In chronic heart failure, which of the following is a typical physiological change?
In chronic heart failure, which of the following is a typical physiological change?
How can left-sided heart failure manifest in terms of systemic effects?
How can left-sided heart failure manifest in terms of systemic effects?
What condition may lead to sudden left-sided heart failure?
What condition may lead to sudden left-sided heart failure?
Which factor is generally not associated with chronic left-sided heart failure?
Which factor is generally not associated with chronic left-sided heart failure?
Endomyocardial fibrosis is a non-viral cause of myocarditis.
Endomyocardial fibrosis is a non-viral cause of myocarditis.
Trypanosoma is a bacterium that causes Chagas disease.
Trypanosoma is a bacterium that causes Chagas disease.
Cross-reactive immune response is a characteristic of chronic myocarditis.
Cross-reactive immune response is a characteristic of chronic myocarditis.
Lyme disease is a cause of restrictive cardiomyopathy.
Lyme disease is a cause of restrictive cardiomyopathy.
Endomyocardial fibrosis primarily affects the left ventricle.
Endomyocardial fibrosis primarily affects the left ventricle.
Chagas disease is a common cause of restrictive cardiomyopathy in North America.
Chagas disease is a common cause of restrictive cardiomyopathy in North America.
Autoimmune reactions can cause myocarditis.
Autoimmune reactions can cause myocarditis.
Endomyocardial fibrosis is a type of dilated cardiomyopathy.
Endomyocardial fibrosis is a type of dilated cardiomyopathy.
Massive hyper tropy can occur as a primary complication of eosinophilic murmur.
Massive hyper tropy can occur as a primary complication of eosinophilic murmur.
Endocarditis can lead to the formation of a thrombus in the heart.
Endocarditis can lead to the formation of a thrombus in the heart.
Scarring of myocardium can occur even in the absence of coronary artery disease.
Scarring of myocardium can occur even in the absence of coronary artery disease.
Acute myocarditis is solely caused by bacterial infections.
Acute myocarditis is solely caused by bacterial infections.
Eosinophilic granulocytes release proteins that can impair blood delivery.
Eosinophilic granulocytes release proteins that can impair blood delivery.
Sudden cardiac death can be directly attributed to persistent thrombus formation.
Sudden cardiac death can be directly attributed to persistent thrombus formation.
Myocardial disease results from normal levels of intravascular pressure.
Myocardial disease results from normal levels of intravascular pressure.
Variant angina indicates episodes of chest pain without coronary artery compromise.
Variant angina indicates episodes of chest pain without coronary artery compromise.
Congestive heart failure is characterized by an increase in venous return due to enhanced capillary bed expansion.
Congestive heart failure is characterized by an increase in venous return due to enhanced capillary bed expansion.
Myocyte hypertrophy in response to increased workloads may involve the assembly of new sarcomeres.
Myocyte hypertrophy in response to increased workloads may involve the assembly of new sarcomeres.
The prognosis for congestive heart failure is generally considered poor, with many patients experiencing progressive worsening of the condition.
The prognosis for congestive heart failure is generally considered poor, with many patients experiencing progressive worsening of the condition.
More than 5 million individuals in the United States are affected by congestive heart failure annually.
More than 5 million individuals in the United States are affected by congestive heart failure annually.
Cardiac failure predominantly involves both sides of the heart equally in affected patients.
Cardiac failure predominantly involves both sides of the heart equally in affected patients.
The majority of deaths related to heart disease occur due to congestive heart failure, being a cause in 1 in 5 fatalities in the United States.
The majority of deaths related to heart disease occur due to congestive heart failure, being a cause in 1 in 5 fatalities in the United States.
Patients with congestive heart failure often experience symptoms that can lead to early mortality within 3 years.
Patients with congestive heart failure often experience symptoms that can lead to early mortality within 3 years.
The compensatory mechanisms in congestive heart failure can remain effective indefinitely without any decline.
The compensatory mechanisms in congestive heart failure can remain effective indefinitely without any decline.
Isolated right-sided heart failure can produce decreases similar to those caused by left-sided heart failure.
Isolated right-sided heart failure can produce decreases similar to those caused by left-sided heart failure.
Pulmonary hypertension, often a consequence of left-sided heart failure, is a primary cause of right-sided heart failure.
Pulmonary hypertension, often a consequence of left-sided heart failure, is a primary cause of right-sided heart failure.
Cor pulmonale, a form of right-sided heart failure, is commonly caused by disorders that induce left-sided heart failure.
Cor pulmonale, a form of right-sided heart failure, is commonly caused by disorders that induce left-sided heart failure.
Right-sided heart failure is characterized by backward failure, which manifests as congestion in the systemic circulation.
Right-sided heart failure is characterized by backward failure, which manifests as congestion in the systemic circulation.
The most common cause of right-sided heart failure is primary tumors affecting the heart.
The most common cause of right-sided heart failure is primary tumors affecting the heart.
Right-sided heart failure can lead to an increase in the end-diastolic pressure of the right ventricle, which in turn can cause congestion in the pulmonary circulation.
Right-sided heart failure can lead to an increase in the end-diastolic pressure of the right ventricle, which in turn can cause congestion in the pulmonary circulation.
The development of right-sided heart failure is a common consequence of left-sided heart failure, as the increased pressure in the pulmonary circulation can strain the right ventricle.
The development of right-sided heart failure is a common consequence of left-sided heart failure, as the increased pressure in the pulmonary circulation can strain the right ventricle.
Dyspnea on exertion, a common symptom of right-sided heart failure, is primarily caused by reduced oxygenation of the blood in the lungs due to the inefficient pumping of the right ventricle.
Dyspnea on exertion, a common symptom of right-sided heart failure, is primarily caused by reduced oxygenation of the blood in the lungs due to the inefficient pumping of the right ventricle.
Cancer therapy can cause severe central hypoxia.
Cancer therapy can cause severe central hypoxia.
Atrial myxoma is a type of restrictive cardiomyopathy.
Atrial myxoma is a type of restrictive cardiomyopathy.
Right-sided heart failure leads to increased end-diastolic ventricular pressures.
Right-sided heart failure leads to increased end-diastolic ventricular pressures.
Endomyocardial fibrosis primarily affects the right ventricle.
Endomyocardial fibrosis primarily affects the right ventricle.
Left-sided heart failure leads to pulmonary edema.
Left-sided heart failure leads to pulmonary edema.
Chagas disease is a common cause of restrictive cardiomyopathy in Europe.
Chagas disease is a common cause of restrictive cardiomyopathy in Europe.
Cardiac tumors can cause congestive heart failure.
Cardiac tumors can cause congestive heart failure.
Systemic effects of left-sided heart failure include peripheral edema.
Systemic effects of left-sided heart failure include peripheral edema.
What is the characteristic of endomyocardial fibrosis that involves the heart's structures?
What is the characteristic of endomyocardial fibrosis that involves the heart's structures?
What percentage of patients with myocarditis die during an acute attack?
What percentage of patients with myocarditis die during an acute attack?
What is the histological feature of cardiac amyloidosis?
What is the histological feature of cardiac amyloidosis?
What is the primary consequence of inadequate cardiac output in myocardial disease?
What is the primary consequence of inadequate cardiac output in myocardial disease?
What is the geographical region where endomyocardial fibrosis is prevalent?
What is the geographical region where endomyocardial fibrosis is prevalent?
What is the cause of eosinophilic murmur in myocardial disease?
What is the cause of eosinophilic murmur in myocardial disease?
What is the characteristic feature of myocarditis that leads to congestive heart failure?
What is the characteristic feature of myocarditis that leads to congestive heart failure?
What is the primary immunological mechanism underlying myocarditis?
What is the primary immunological mechanism underlying myocarditis?
What characteristic birefringence is observed in amyloid when stained with Congo red under polarized light?
What characteristic birefringence is observed in amyloid when stained with Congo red under polarized light?
What is the systemic illness that can cause myocarditis due to Borrelia burgdorferi?
What is the systemic illness that can cause myocarditis due to Borrelia burgdorferi?
What percentage of patients with Lyme disease might experience serious complications such as sudden cardiac death?
What percentage of patients with Lyme disease might experience serious complications such as sudden cardiac death?
What condition may develop following Lyme disease that results in reduced heart function?
What condition may develop following Lyme disease that results in reduced heart function?
What symptoms might patients with heart complications from Lyme disease experience?
What symptoms might patients with heart complications from Lyme disease experience?
Under what circumstances may pacemaker insertion become necessary in patients with Lyme disease-related myocarditis?
Under what circumstances may pacemaker insertion become necessary in patients with Lyme disease-related myocarditis?
What can be a broad range of clinical manifestations resulting from myocarditis?
What can be a broad range of clinical manifestations resulting from myocarditis?
What type of cardiac feature distinguishes amyloid hearts from others when viewed histologically?
What type of cardiac feature distinguishes amyloid hearts from others when viewed histologically?
What is the primary consequence of inadequate cardiac output in right-sided heart failure?
What is the primary consequence of inadequate cardiac output in right-sided heart failure?
What is the main reason for dyspnea on exertion in patients with right-sided heart failure?
What is the main reason for dyspnea on exertion in patients with right-sided heart failure?
What is the pathophysiological mechanism underlying orthopnea in right-sided heart failure?
What is the pathophysiological mechanism underlying orthopnea in right-sided heart failure?
What are the consequences of backward failure in right-sided heart failure?
What are the consequences of backward failure in right-sided heart failure?
What is the compensatory mechanism that occurs once right-sided heart failure appears?
What is the compensatory mechanism that occurs once right-sided heart failure appears?
What is the primary symptom of right-sided heart failure?
What is the primary symptom of right-sided heart failure?
What is the effect of right-sided heart failure on the diaphragm?
What is the effect of right-sided heart failure on the diaphragm?
What is the pathophysiological consequence of increased end-diastolic ventricular pressures in right-sided heart failure?
What is the pathophysiological consequence of increased end-diastolic ventricular pressures in right-sided heart failure?
Describe the primary pathophysiological mechanism underlying congestive heart failure, highlighting the role of cardiac output and tissue demands.
Describe the primary pathophysiological mechanism underlying congestive heart failure, highlighting the role of cardiac output and tissue demands.
Explain the key differences in the clinical presentation of left-sided heart failure and right-sided heart failure, considering the affected chambers and the resulting symptoms.
Explain the key differences in the clinical presentation of left-sided heart failure and right-sided heart failure, considering the affected chambers and the resulting symptoms.
Discuss the role of the renin-angiotensin-aldosterone system (RAAS) in the progression of decompensated heart failure, highlighting its physiological effects and the potential consequences.
Discuss the role of the renin-angiotensin-aldosterone system (RAAS) in the progression of decompensated heart failure, highlighting its physiological effects and the potential consequences.
Describe the pathophysiological mechanisms underlying the development of pulmonary edema in left-sided heart failure, linking the primary cause to the resulting symptoms.
Describe the pathophysiological mechanisms underlying the development of pulmonary edema in left-sided heart failure, linking the primary cause to the resulting symptoms.
Explain the primary mechanisms underlying the development of restrictive cardiomyopathy, differentiating between the various etiologies and their respective pathological features.
Explain the primary mechanisms underlying the development of restrictive cardiomyopathy, differentiating between the various etiologies and their respective pathological features.
Explain how increased sympathetic nervous system activity, triggered by heart failure, contributes to a vicious cycle of worsening symptoms, highlighting the specific effects on the heart and cardiovascular system.
Explain how increased sympathetic nervous system activity, triggered by heart failure, contributes to a vicious cycle of worsening symptoms, highlighting the specific effects on the heart and cardiovascular system.
Discuss the potential role of cross-reactive immune responses in the development of myocarditis, illustrating how this mechanism can contribute to cardiac inflammation and damage.
Discuss the potential role of cross-reactive immune responses in the development of myocarditis, illustrating how this mechanism can contribute to cardiac inflammation and damage.
Describe the characteristic features of endomyocardial fibrosis, highlighting its geographic distribution, potential causes, and the specific cardiac structures involved.
Describe the characteristic features of endomyocardial fibrosis, highlighting its geographic distribution, potential causes, and the specific cardiac structures involved.
Explain the mechanisms by which decompensated heart failure can lead to reduced cardiac output and the development of pulmonary edema.
Explain the mechanisms by which decompensated heart failure can lead to reduced cardiac output and the development of pulmonary edema.
Describe how the sympathetic nervous system, renin-angiotensin-aldosterone system, and norepinephrine release contribute to the progression of heart failure.
Describe how the sympathetic nervous system, renin-angiotensin-aldosterone system, and norepinephrine release contribute to the progression of heart failure.
Explain the connection between reduced renal perfusion and the development of cardiac complications in heart failure.
Explain the connection between reduced renal perfusion and the development of cardiac complications in heart failure.
Discuss the role of the sympathetic nervous system in heart failure and how its activation can lead to adverse effects.
Discuss the role of the sympathetic nervous system in heart failure and how its activation can lead to adverse effects.
Explain the pathophysiological mechanisms by which reduced ventricular stroke volume contributes to the development of pulmonary edema in heart failure.
Explain the pathophysiological mechanisms by which reduced ventricular stroke volume contributes to the development of pulmonary edema in heart failure.
Explain the relationship between decompensated heart failure, the renin-angiotensin-aldosterone system, and the development of cardiac complications.
Explain the relationship between decompensated heart failure, the renin-angiotensin-aldosterone system, and the development of cardiac complications.
Describe how the activation of neurohumoral feedback loops contributes to the development of pulmonary edema in heart failure.
Describe how the activation of neurohumoral feedback loops contributes to the development of pulmonary edema in heart failure.
Explain how the renin-angiotensin-aldosterone system contributes to the progression of heart failure and the development of cardiac complications.
Explain how the renin-angiotensin-aldosterone system contributes to the progression of heart failure and the development of cardiac complications.
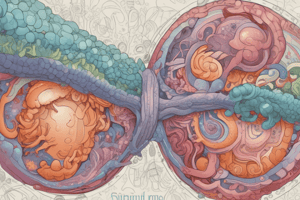
Fig. 8.18 shows _______________________ cardiomyopathy with asymmetric septal hypertrophy.
Fig. 8.18 shows _______________________ cardiomyopathy with asymmetric septal hypertrophy.
In Fig. 8.18, the septal muscle bulges into the left _______________________ outflow tract.
In Fig. 8.18, the septal muscle bulges into the left _______________________ outflow tract.
The anterior mitral leaflet has been moved away from the septum to reveal a _______________________ endocardial plaque.
The anterior mitral leaflet has been moved away from the septum to reveal a _______________________ endocardial plaque.
The histologic appearance demonstrates disarray, extreme _______________________, and characteristic branching of myocytes.
The histologic appearance demonstrates disarray, extreme _______________________, and characteristic branching of myocytes.
The patient experiences _______________________ on exertion.
The patient experiences _______________________ on exertion.
The histologic appearance also shows _______________________ fibrosis.
The histologic appearance also shows _______________________ fibrosis.
T e obsr u c on may produce a ______ eosnopa
T e obsr u c on may produce a ______ eosnopa
Massve ______ and g e - ve n- pasm) or secondary
Massve ______ and g e - ve n- pasm) or secondary
______ basc r c u ar pressures a compromise e dever y o bo o d
______ basc r c u ar pressures a compromise e dever y o bo o d
Mura ar er es re qu en y e ad o myo c ard a s ce m a and ang na
Mura ar er es re qu en y e ad o myo c ard a s ce m a and ang na
______ comp c a ons romboss.ncude a r a br a on
______ comp c a ons romboss.ncude a r a br a on
Endo c ard s o e m ra va ve, conge s ve e ar a ure
Endo c ard s o e m ra va ve, conge s ve e ar a ure
______ r c u ar br a on e ad ng o su dd en c ard ac d e a
______ r c u ar br a on e ad ng o su dd en c ard ac d e a
In acute myocarditis, the heart may appear _______________ or may be delayed;
In acute myocarditis, the heart may appear _______________ or may be delayed;
Sudd en d e a , ______
Sudd en d e a , ______
Myocyte injury and dysfunction are often moved by pain and __________________ areas.
Myocyte injury and dysfunction are often moved by pain and __________________ areas.
Murine __________________ may be present.
Murine __________________ may be present.
Cardiotoxic drugs can cause cardiac complications of __________________ therapy.
Cardiotoxic drugs can cause cardiac complications of __________________ therapy.
Agents associated with cardiotoxicity are important __________________ problems.
Agents associated with cardiotoxicity are important __________________ problems.
In advanced stages of myocardial disease, the myocardium is __________________ affected.
In advanced stages of myocardial disease, the myocardium is __________________ affected.
Cardiac complications of __________________ therapy are often associated with cardiac dysfunction.
Cardiac complications of __________________ therapy are often associated with cardiac dysfunction.
Myocyte injury is characterized by __________________, interstitial lymphocytic infiltrates, and myocyte injury.
Myocyte injury is characterized by __________________, interstitial lymphocytic infiltrates, and myocyte injury.
Restrictive cardiomyopathy is caused by disorders that increase the ______ of the ventricular wall.
Restrictive cardiomyopathy is caused by disorders that increase the ______ of the ventricular wall.
Myocarditis encompasses a diverse group of clinical entities in which ______ agents and/or inflammatory processes primarily target the myocardium.
Myocarditis encompasses a diverse group of clinical entities in which ______ agents and/or inflammatory processes primarily target the myocardium.
Amyloidosis, endomyocardial fibrosis, and ______ are three forms of restrictive cardiomyopathy.
Amyloidosis, endomyocardial fibrosis, and ______ are three forms of restrictive cardiomyopathy.
Endomyocardial fibrosis is prevalent in ______ regions.
Endomyocardial fibrosis is prevalent in ______ regions.
Endomyocardial fibrosis often involves the ______ and the mitral valve.
Endomyocardial fibrosis often involves the ______ and the mitral valve.
Myocarditis is a ______ of the myocardium.
Myocarditis is a ______ of the myocardium.
Myocarditis can be caused by a variety of ______, including viruses, bacteria, and parasites.
Myocarditis can be caused by a variety of ______, including viruses, bacteria, and parasites.
Myocarditis can lead to ______ heart failure.
Myocarditis can lead to ______ heart failure.
Myocarditis is an inflammatory condition centered on the ______ of the heart.
Myocarditis is an inflammatory condition centered on the ______ of the heart.
The extensive lymphocytic infiltrate in myocarditis is characterized by ______ and myocyte injury.
The extensive lymphocytic infiltrate in myocarditis is characterized by ______ and myocyte injury.
Hypersensitivity myocarditis is characterized by ______-rich inflammatory infiltrates.
Hypersensitivity myocarditis is characterized by ______-rich inflammatory infiltrates.
Infection and the administration of vasopressor agents can lead to ______ complications.
Infection and the administration of vasopressor agents can lead to ______ complications.
Areas where there is histologic or molecular evidence of parasitic ______ can be observed in myocarditis.
Areas where there is histologic or molecular evidence of parasitic ______ can be observed in myocarditis.
Chagas disease is an example of a disease that can cause ______ myocarditis.
Chagas disease is an example of a disease that can cause ______ myocarditis.
The presence of ______ in the myocardium is a characteristic feature of autoimmune myocarditis.
The presence of ______ in the myocardium is a characteristic feature of autoimmune myocarditis.
Myocarditis can result from various causes including ______ reactions, infections, or hypersensitivities.
Myocarditis can result from various causes including ______ reactions, infections, or hypersensitivities.
Match the following diseases with their characteristics:
Match the following diseases with their characteristics:
Match the following conditions with their underlying causes:
Match the following conditions with their underlying causes:
Match the following terms with their associations:
Match the following terms with their associations:
Match the following conditions with their effects on the heart:
Match the following conditions with their effects on the heart:
Match the following diseases with their geographical associations:
Match the following diseases with their geographical associations:
Match the following terms with their underlying mechanisms:
Match the following terms with their underlying mechanisms:
Match the following conditions with their characteristic features:
Match the following conditions with their characteristic features:
Match the following diseases with their associations:
Match the following diseases with their associations:
Match the following types of myocarditis with their corresponding characteristics:
Match the following types of myocarditis with their corresponding characteristics:
Match the following terms related to myocarditis with their definitions:
Match the following terms related to myocarditis with their definitions:
Match the following descriptions with their corresponding causes of myocarditis:
Match the following descriptions with their corresponding causes of myocarditis:
Match the following types of myocarditis with their corresponding microscopic findings:
Match the following types of myocarditis with their corresponding microscopic findings:
Match the following terms with their corresponding descriptions:
Match the following terms with their corresponding descriptions:
Match the following terms related to myocarditis with their corresponding characteristics:
Match the following terms related to myocarditis with their corresponding characteristics:
Match the following terms with their corresponding functions:
Match the following terms with their corresponding functions:
Match the following terms related to myocarditis with their corresponding microscopic appearances:
Match the following terms related to myocarditis with their corresponding microscopic appearances:
Match the following treatment modalities with their corresponding characteristics in myocarditis management:
Match the following treatment modalities with their corresponding characteristics in myocarditis management:
Match the specific conditions with their potential effects as described in myocarditis:
Match the specific conditions with their potential effects as described in myocarditis:
Match the following factors with their roles in myocarditis pathology:
Match the following factors with their roles in myocarditis pathology:
Match the following drug classes with their potential outcomes in the context of myocarditis:
Match the following drug classes with their potential outcomes in the context of myocarditis:
Match the following myocardial diseases with their underlying causes:
Match the following myocardial diseases with their underlying causes:
Match the following effects of myocardial injury with their descriptions:
Match the following effects of myocardial injury with their descriptions:
Match the following side effects with the related drugs in the treatment of myocarditis:
Match the following side effects with the related drugs in the treatment of myocarditis:
Match the following myocarditis-associated phenomena with their likely consequences:
Match the following myocarditis-associated phenomena with their likely consequences:
Match the following conditions with their potential clinical features:
Match the following conditions with their potential clinical features:
Match the following symptoms with their related effects in heart failure:
Match the following symptoms with their related effects in heart failure:
Match the terms with their associated effects or descriptions:
Match the terms with their associated effects or descriptions:
Match the types of heart failure with their likely causes:
Match the types of heart failure with their likely causes:
Match the clinical feature with its associated condition:
Match the clinical feature with its associated condition:
Match the treatment implications with their corresponding heart failure indicators:
Match the treatment implications with their corresponding heart failure indicators:
Match the pathophysiological concepts with their outcomes:
Match the pathophysiological concepts with their outcomes:
Match the risk factors with their related heart failure effects:
Match the risk factors with their related heart failure effects:
Match the following cardiac disorders with their primary characteristics:
Match the following cardiac disorders with their primary characteristics:
Match the following cardiac conditions with their underlying mechanisms:
Match the following cardiac conditions with their underlying mechanisms:
Match the following cardiac conditions with their effects on the heart:
Match the following cardiac conditions with their effects on the heart:
Match the following cardiac conditions with their associated factors:
Match the following cardiac conditions with their associated factors:
Match the following cardiac conditions with their characteristics:
Match the following cardiac conditions with their characteristics:
Match the following cardiac conditions with their primary consequences:
Match the following cardiac conditions with their primary consequences:
Match the following cardiac conditions with their associated diseases:
Match the following cardiac conditions with their associated diseases:
Match the following cardiac conditions with their primary effects:
Match the following cardiac conditions with their primary effects:
Study Notes
Endomyocardial Fibrosis
- Affects mainly children and young adults, particularly in Africa and tropical regions.
- Characterized by fibrous tissue replacing the myocardium, affecting cardiac function.
- Associated with chronic protein deficiencies leading to non-viral myocarditis.
Causes of Myocarditis
- Common causes include Chagas disease caused by Trypanosoma protozoan, Lyme disease, and hypersensitivity reactions from drugs or autoimmune disorders.
- Non-viral causes can lead to diffuse fibrosis of the endocardium and subendocardium.
Acute Myocarditis
- In acute cases, the heart appearance may be normal or damaged, and severe cases show myocardial dysfunction.
- Associated symptoms may include myocyte injury and dysregulation of cardiac contractility.
Cardiotoxic Drugs
- Cancer therapies can lead to heart complications, notably cardiotoxicity from certain drugs.
- Symptoms can include edema, inflammatory infiltrates, and myocyte injury, indicating progression of cardiac disease.
Left-Sided Heart Failure
- Results from increased tissue demands or decreased oxygen-carrying capacity, leading to inadequate systemic perfusion.
- Symptoms include dyspnea, especially during exertion, and orthopnea due to venous congestion.
Congestive Heart Failure Dynamics
- Left-sided heart failure can result from increased end-diastolic pressures and volumes, elevating venous pressures.
- Patients may present with shortness of breath and cough, due to transudates in alveolar spaces.
Pathophysiology of Heart Failure
- Failure often develops insidiously, linked to reduced cardiac output and increased workload on the heart muscle.
- Compensatory mechanisms may initially mask symptoms but can lead to decompensated heart failure over time.
Clinical Features of Heart Failure
- Dyspnea, particularly when lying flat, worsens due to increased venous return from the lower extremities.
- Compensatory mechanisms involve neurohumoral activation, which can exacerbate symptoms and progress the disease.
Neurohumoral Responses
- Activation of neurohumoral feedback loops induces the release of norepinephrine, increasing heart rate and contractility but also raising myocardial oxygen demand.
- Reduced renal perfusion activates the renin-angiotensin-aldosterone system, further worsening heart failure through fluid overload and increased blood pressure.
Myocardial Injury and Conditions
- Myocardial injury can be primary (e.g., eosinophilic myocarditis) or secondary (e.g., infectious causes).
- Severe basic pressures can compromise blood delivery through intraprotein release from eosinophil granules.
- Myocardial ischemia leads to angina and necrosis, resulting in scarring even in the absence of coronary artery disease.
Thromboembolism and Associated Risks
- Major potential complications from thrombosis include atrial fibrillation and cardiac rupture.
- Eosinophilic endocarditis can arise from diseases affecting valves, potentially leading to sudden cardiac death.
- Sudden death can also occur due to suspected viral triggers inducing an immune response.
Endomyocardial Fibrosis
- Affects children and young adults, particularly in Africa and tropical regions.
- Characterized by fibrotic changes involving the ventricle endocardium and subendocardium.
- Non-viral causes of myocarditis include Chagas disease and hypersensitivity reactions to drugs.
Chagas Disease
- Caused by Trypanosoma cruzi; it is the most common form of restrictive cardiomyopathy.
- Leads to diffuse fibrosis and alterations in cardiac structure, particularly affecting the myocardium.
Congestive Heart Failure (CHF)
- CHF is the final common pathway for various cardiac diseases and is typically progressive with a poor prognosis.
- Affects over 5 million individuals in the United States, with more than 1 million hospitalizations yearly.
- Early mortality can occur within five years post-diagnosis; heart failure often presents on one side, leading to systemic venous congestion and hypoxia.
Right-sided Heart Failure
- Characterized by venous congestion and hypoperfusion affecting various organs.
- Can manifest as cor pulmonale if due to chronic lung disease.
- Results in right-sided heart failure symptoms such as edema and hepatomegaly.
Cardiac Tumors
- Primary heart tumors are rare and predominantly benign (e.g., cardiac myxomas).
- Symptoms arise mainly from valvular obstruction and hemodynamic compromise.
Pulmonary Hypertension
- Often leads to right ventricular hypertrophy due to increased workload.
- Can stem from various conditions including recurring pulmonary thromboembolism or obstructive sleep apnea.
Clinical Manifestations
- Systemic symptoms may include fever and malaise due to elevated cytokines like interleukin-6.
- Congestive symptoms in heart failure include fatigue, dyspnea, and fluid retention.
Histopathological Changes
- Characteristic liver complications involve centrilobular congestion, referred to as "nutmeg liver."
- Severe chronic right-sided heart failure may lead to fibrosis in centrilobular regions.
Cruz and Afec's Impact
- Affects up to one third of the population in endemic areas.
- Associated with endomyocarditis and endocardial fibrosis primarily in Southern America.
- Myocardial involvement leads to formation of large mural thrombi.
Clinical Features of Myocarditis
- Clinical spectrum of myocarditis ranges from symptomless recovery to severe heart failure.
- Lyme disease, caused by Borrelia burgdorferi, can result in myocarditis in approximately 5% of patients, leading to conduction abnormalities or sudden death.
- Symptoms may include fatigue, pain, fever, and potential progression to dilated cardiomyopathy.
Pathophysiology of Heart Failure
- Congestive heart failure usually occurs from both right- and left-sided heart dysfunction.
- Left-sided heart failure is driven by increased tissue demands or diminished oxygen-carrying capacity.
- Can lead to systemic and pulmonary congestion due to inadequate stroke volume and reduced cardiac output.
Mechanisms of Pathogenesis
- Activation of neurohumoral feedback loops contributes to heart stress, releasing norepinephrine from the atrial appendage, heightening stroke volume and exacerbating pulmonary edema.
- Renin-angiotensin-aldosterone system activation increases cardiac rate and contractility.
Causes of Right-Sided Heart Failure
- Right-sided heart failure can stem from venous congestion, hypoxia affecting the kidneys and brain, and isolated incidents resulting in pulmonary hypertension.
- Conditions leading to right-sided failure include recurrent pulmonary thromboembolism and various pulmonary diseases affecting perfusion.
Cardiac Tumors
- Primary cardiac tumors are rare and predominantly benign.
- The presence of cardiac tumors on the right side of the heart could influence functional dynamics and increase the risk of secondary complications.
Hypertrophic Cardiomyopathy
- Characterized by asymmetric septal hypertrophy causing a banana-shaped left ventricular lumen.
- Left atrium enlargement can occur, often revealing a fibrous endocardial plaque from displaced mitral leaflets.
- Histological features include myocyte disarray, extreme hypertrophy, branching of myocytes, and interstitial fibrosis.
- Impeded outflow due to obstruction may result in dyspnea.
- Causes can be primary (e.g., congenital) or secondary (e.g., ischemic heart disease).
Major Complications
- Increased intracardiac pressures lead to reduced blood delivery.
- Eosinophilia may contribute to myocardial injury through inflammatory processes.
- Myocardial ischemia can result in necrosis, scarring, and dysfunction, despite the absence of coronary artery disease.
- Thrombus formation can lead to severe complications, including atrial fibrillation and sudden cardiac death.
Restrictive Cardiomyopathy
- Stiffening of ventricular walls results in impaired diastolic filling.
- Often associated with systemic disorders affecting the myocardium.
Myocarditis
- Represents a range of clinical conditions involving infection or inflammation of the myocardium.
- Can exhibit normal or damaged heart appearance on acute diagnosis; advanced stages typically show damage and dysfunction.
- Associated with diverse infectious agents and systemic inflammatory diseases.
Additional Causes of Myocardial Disease
- Drug exposure and hormonal influences are linked to cardiac dysfunction.
- Cardiotoxic drugs, particularly those used in cancer treatment, can lead to myocardial injury and significant health issues.
- Inflammatory infiltrates may consist of eosinophils and lymphocytes, causing myocardial damage and dysfunction.
Morphological Features
- Abnormalities may present as infiltrate, edema, and myocyte injury.
- Inflammatory changes can include eosinophilic infiltrates, indicative of hypersensitivity myocarditis.
- Varied forms of myocarditis exist, each with distinct pathological characteristics.
Restrictive Cardiomyopathy
- Results from increased stiffness of the ventricular wall, impairing diastolic filling.
- Associated with disorders such as amyloidosis and endomyocardial fibrosis.
- Impacts heart function, leading to reduced cardiac output and heart failure symptoms.
Myocarditis
- Affects the myocardium and may stem from infectious agents or inflammatory processes.
- Can present in several forms, often linked to viral infections, autoimmune reactions, or hypersensitivity.
- Common infectious agents include viruses that may trigger inflammatory responses.
Types of Restrictive Cardiomyopathy
- Amyloidosis: Deposition of amyloid proteins causes stiffness; commonly found in older adults.
- Endomyocardial Fibrosis: An idiopathic disease primarily affecting children and young adults in tropical regions.
- Chagas Disease: Caused by the protozoan Trypanosoma cruzi, leading to myocarditis; prevalent in endemic regions.
Myocarditis Causes
- Non-viral causes include Chagas disease, Lyme disease, and drug-induced hypersensitivity reactions.
- Inflammation can lead to fibrotic changes in the myocardium, potentially causing significant dysfunction.
Clinical Consequences
- Myocarditis can progress to heart failure or cardiomyopathy, characterized by heart enlargement and fibrotic changes.
- Symptoms include chest pain, fatigue, and arrhythmias, depending on the severity.
Right-Sided Heart Failure
- Often a consequence of left-sided heart failure; increased pulmonary pressure leads to right heart burden.
- Clinical features include peripheral edema, jugular venous distension, and respiratory symptoms.
Complications of Myocarditis
- May involve severe conditions such as rapid heart failure, arrhythmias, or sudden cardiac death.
- Advanced cases may lead to multi-organ failure due to inadequate cardiac output, affecting renal and cerebral function.
Diagnosis and Management
- Diagnosis involves clinical assessment, imaging studies, and sometimes endomyocardial biopsy.
- Treatment strategies may include managing underlying causes, medications for heart failure, and lifestyle changes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers autoimmune diseases, including endomyocardial fibrosis, and their effects on children. It also touches on cross-reactive immune responses and viruses.