Podcast
Questions and Answers
Why is hyperthermia harmful in patients with brain injury?
Why is hyperthermia harmful in patients with brain injury?
Hyperthermia increases cerebral metabolic demand by 8–13% per °C, escalates glutamate release, oxygen free radical production, cytoskeletal breakdown, blood-brain barrier disruption, and vasogenic edema.
What temperature threshold should prompt aggressive treatment in post-ischemic patients, and what interventions are recommended?
What temperature threshold should prompt aggressive treatment in post-ischemic patients, and what interventions are recommended?
Temperatures >38°C should be treated with acetaminophen and surface cooling.
What are the neuroprotective mechanisms of therapeutic hypothermia?
What are the neuroprotective mechanisms of therapeutic hypothermia?
Reduces glutamate release, metabolic demand, free radicals, inflammatory cytokines, and programmed cell death.
What target temperature and duration are recommended for comatose adults after cardiac arrest?
What target temperature and duration are recommended for comatose adults after cardiac arrest?
How is cooling initiated per the abbreviated hypothermia protocol?
How is cooling initiated per the abbreviated hypothermia protocol?
What steps are critical to prevent shivering during therapeutic hypothermia?
What steps are critical to prevent shivering during therapeutic hypothermia?
When should rewarming begin, and at what rate?
When should rewarming begin, and at what rate?
According to Fig. 4.3, what actions are taken on Day 0 (ROSC) for neuroprognostication?
According to Fig. 4.3, what actions are taken on Day 0 (ROSC) for neuroprognostication?
What defines a "strong predictor" of poor outcome >72 hours post-normothermia?
What defines a "strong predictor" of poor outcome >72 hours post-normothermia?
What are "moderate predictors" of poor outcome requiring ≥2 findings?
What are "moderate predictors" of poor outcome requiring ≥2 findings?
Why is prognostication unreliable before 72 hours post-cardiac arrest?
Why is prognostication unreliable before 72 hours post-cardiac arrest?
What is the recommended approach to DNR orders in brain injury patients?
What is the recommended approach to DNR orders in brain injury patients?
How should SSEP timing differ between TTM and non-TTM patients?
How should SSEP timing differ between TTM and non-TTM patients?
What is the role of neuron-specific enolase (NSE) in prognostication?
What is the role of neuron-specific enolase (NSE) in prognostication?
What cooling methods are preferred over ice packs or fans?
What cooling methods are preferred over ice packs or fans?
When should therapeutic hypothermia not be used?
When should therapeutic hypothermia not be used?
What is critical to avoid during rewarming?
What is critical to avoid during rewarming?
According to Fig. 4.3, when is brain death evaluation appropriate?
According to Fig. 4.3, when is brain death evaluation appropriate?
What is the key takeaway for emergency clinicians regarding prognostication?
What is the key takeaway for emergency clinicians regarding prognostication?
What are the first steps in the abbreviated protocol for induced hypothermia after cardiac arrest?
What are the first steps in the abbreviated protocol for induced hypothermia after cardiac arrest?
How should cooling be prioritized in post-arrest patients requiring coronary intervention?
How should cooling be prioritized in post-arrest patients requiring coronary intervention?
What monitoring is required during therapeutic hypothermia?
What monitoring is required during therapeutic hypothermia?
How is shivering managed during cooling?
How is shivering managed during cooling?
When should rewarming begin, and how is it managed?
When should rewarming begin, and how is it managed?
What are key contraindications to therapeutic hypothermia?
What are key contraindications to therapeutic hypothermia?
According to Fig. 4.3, what actions are required on Day 1 post-ROSC?
According to Fig. 4.3, what actions are required on Day 1 post-ROSC?
When is brain death evaluation appropriate post-arrest?
When is brain death evaluation appropriate post-arrest?
What diagnostic tests are recommended by Day 3–5 for prognostication?
What diagnostic tests are recommended by Day 3–5 for prognostication?
What defines a "strong predictor" of poor outcome >72 hours post-arrest?
What defines a "strong predictor" of poor outcome >72 hours post-arrest?
How should families be counseled during early post-arrest care?
How should families be counseled during early post-arrest care?
What institutional framework is critical for successful hypothermia protocols?
What institutional framework is critical for successful hypothermia protocols?
Why is prehospital cooling not recommended?
Why is prehospital cooling not recommended?
What is the role of NSE in prognostication?
What is the role of NSE in prognostication?
How long should therapeutic hypothermia be maintained in adults?
How long should therapeutic hypothermia be maintained in adults?
What is critical for ICU management during cooling?
What is critical for ICU management during cooling?
What is the key takeaway from the TTM trials comparing 33°C vs. 36°C?
What is the key takeaway from the TTM trials comparing 33°C vs. 36°C?
How does status myoclonus impact prognosis?
How does status myoclonus impact prognosis?
What is the final step in the hypothermia protocol?
What is the final step in the hypothermia protocol?
Flashcards
Hyperthermia Harm in Brain Injury
Hyperthermia Harm in Brain Injury
Hyperthermia worsens brain injury by increasing metabolic demand, glutamate release, free radical production, and blood-brain barrier disruption.
Hyperthermia Treatment Threshold
Hyperthermia Treatment Threshold
Treat temperatures >38°C aggressively with acetaminophen and surface cooling in post-ischemic patients.
Neuroprotective Hypothermia
Neuroprotective Hypothermia
Therapeutic hypothermia reduces glutamate release, metabolic demand, free radicals, inflammatory cytokines, and cell death.
Target Temperature Post-Arrest
Target Temperature Post-Arrest
Signup and view all the flashcards
Initiating Cooling Protocol
Initiating Cooling Protocol
Signup and view all the flashcards
Preventing Shivering
Preventing Shivering
Signup and view all the flashcards
Rewarming Rate
Rewarming Rate
Signup and view all the flashcards
Day 0 Actions (Neuroprognosis)
Day 0 Actions (Neuroprognosis)
Signup and view all the flashcards
Poor Outcome Predictors
Poor Outcome Predictors
Signup and view all the flashcards
Delayed Prognostication
Delayed Prognostication
Signup and view all the flashcards
Initial Hypothermia Steps
Initial Hypothermia Steps
Signup and view all the flashcards
Cooling vs. Coronary Intervention
Cooling vs. Coronary Intervention
Signup and view all the flashcards
Hypothermia Monitoring
Hypothermia Monitoring
Signup and view all the flashcards
Shivering Management
Shivering Management
Signup and view all the flashcards
Rewarming Management
Rewarming Management
Signup and view all the flashcards
Hypothermia Contraindications
Hypothermia Contraindications
Signup and view all the flashcards
Day 1 Post-ROSC Actions
Day 1 Post-ROSC Actions
Signup and view all the flashcards
Brain Death Evaluation Timing
Brain Death Evaluation Timing
Signup and view all the flashcards
Prognostication Tests-Day 3-5
Prognostication Tests-Day 3-5
Signup and view all the flashcards
Strong Predictors of Poor Outcome
Strong Predictors of Poor Outcome
Signup and view all the flashcards
Counseling Families
Counseling Families
Signup and view all the flashcards
Institutional Framework Hypothermia
Institutional Framework Hypothermia
Signup and view all the flashcards
Prehospital Cooling
Prehospital Cooling
Signup and view all the flashcards
Role of NSE
Role of NSE
Signup and view all the flashcards
Hypothermia Duration
Hypothermia Duration
Signup and view all the flashcards
ICU Management
ICU Management
Signup and view all the flashcards
TTM 33 vs 36
TTM 33 vs 36
Signup and view all the flashcards
Status Myoclonus Impact Prognosis
Status Myoclonus Impact Prognosis
Signup and view all the flashcards
TTM Significance
TTM Significance
Signup and view all the flashcards
Considerations for BBT(Brain-death testing)
Considerations for BBT(Brain-death testing)
Signup and view all the flashcards
Study Notes
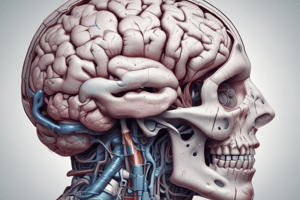
Hyperthermia in Brain Injury
- Hyperthermia increases cerebral metabolic demand by 8–13% per °C.
- It escalates glutamate release, oxygen free radical production, cytoskeletal breakdown, blood-brain barrier disruption, and vasogenic edema.
- Mnemonic: "HOT BRAIN" (BBB breakdown, Release of glutamate, Antioxidant depletion, Temperature-driven metabolic demand, Brain injury exacerbation).
Treatment of Post-Ischemic Patients
- Initiate aggressive treatment for temperatures >38°C.
- Interventions include acetaminophen and surface cooling.
Neuroprotective Mechanisms of Therapeutic Hypothermia
- Reduces glutamate release, metabolic demand, free radicals, inflammatory cytokines, and programmed cell death.
Target Temperature and Duration for Comatose Adults After Cardiac Arrest
- Target 33°C for 24 hours.
- Recent trials suggest 33°C provides better neuroprotection than 36°C, though safety outcomes are similar.
- Mnemonic: "COOL 33" (Cooling to 33°C, Optimal outcomes, Length 24h).
Initiating Cooling
- Rapid infusion of 2 L cold (4°C) IV saline immediately after ROSC.
- Follow with surface/endovascular cooling devices.
- Avoid blankets or heated ventilator circuits.
Preventing Shivering During Therapeutic Hypothermia
- Use sedation and nondepolarizing paralytics (e.g., bolus in ED, drip in ICU).
Rewarming
- Begin at 24 hours post-cooling.
- Rewarm to 36.5°C at 0.15°C/hour.
- Avoid rebound hyperthermia.
Actions on Day 0 (ROSC) for Neuroprognostication
- Initiate TTM.
- Perform CT brain.
- Start long-term EEG.
- Document status myoclonus.
- Assess motor response (flexion/better = indeterminate prognosis).
Strong Predictors of Poor Outcome >72 Hours Post-Normothermia
- Bilateral absent pupillary reflexes OR absent pupillary + corneal reflexes, OR bilateral absence of N20 waves on SSEP.
- False-positive rate <5%.
"Moderate predictors" of poor outcome
- Requires ≥2 findings
Status Myoclonus
- Status myoclonus <48h, unreactive/burst-suppression EEG, diffuse anoxic injury on CT/MRI.
Prognostication
- Prognostication is unreliable before 72 hours post-cardiac arrest due to sedatives/paralytics from TTM confounding exams.
- Early withdrawal of care creates a self-fulfilling prophecy.
- Mnemonic: "72 HRS" (Hours for Reliable Signs).
DNR Orders
- Avoid assigning new DNR status within the first 24 hours to prevent self-fulfilling prophecies.
SSEP Timing
- Perform SSEP after rewarming or 24–72h post-arrest in TTM patients.
- Obtain earlier (Day 2) in non-TTM patients.
Neuron-Specific Enolase (NSE)
- Higher NSE correlates with worse outcomes, but thresholds lack standardization.
- Do not rely on NSE alone.
Cooling Methods
- Use intranasal, intravascular, or surface temperature-modulating devices, or cold saline infusions instead of ice packs or fans
When to Avoid Therapeutic Hypothermia
- After ischemic stroke (no proven benefit).
During Rewarming
- Avoid rebound hyperthermia (common with passive rewarming).
Brain Death Evaluation
- If brainstem reflexes are absent >24h post-ROSC and temperature >36°C.
Prognostication Takeaway
- Avoid nihilism.
- Delay prognostication until ≥72h post-arrest using a multimodal approach (exam, EEG, SSEP, imaging).
First Steps in Induced Hypothermia After Cardiac Arrest
- Rapidly infuse 2 L of cold (4°C) IV saline.
- Expose the patient (no blankets/heated ventilator).
- Place temperature probes (urinary catheter + esophageal).
- Initiate cooling via surface/endovascular devices.
Cooling in Post-Arrest Patients Requiring Coronary Intervention
- Cooling should not delay door-to-balloon time for acute MI.
- Initiate cooling in the ED if time permits; otherwise, start in the catheterization lab.
Monitoring During Therapeutic Hypothermia
- Temperature: Esophageal + bladder probes.
- Continuous EEG for seizures.
- SSEPs after rewarming (TTM patients) or by Day 2 (non-TTM patients).
- Arterial blood gases (pH stat or alpha stat).
Managing Shivering During Cooling
- Use sedation (e.g., midazolam/propofol) and nondepolarizing paralytics (e.g., rocuronium).
- Bolus paralytics in the ED; transition to drips in the ICU.
Managing Rewarming
- Start at 24 hours post-cooling.
- Rate: 0.15°C/hour to a target of 36.5°C.
- Avoid rebound hyperthermia (use active rewarming if needed).
- Discontinue paralytics at rewarming onset; use sedation/narcotics for shivering.
Key Contraindications to Therapeutic Hypothermia
- Ischemic stroke (no proven benefit) and unstable hemodynamics (avoid hypotension/hypoxia during cooling).
Actions Required on Day 1 Post-ROSC
- Begin rewarming.
- Document status myoclonus.
- Continue EEG monitoring.
- Evaluate for absent brainstem reflexes (if present, perform brain death assessment once temperature >36°C).
Brain Death Evaluation
- If brainstem reflexes (e.g., pupillary, corneal) are absent >24 hours post-ROSC AND temperature is >36°C.
Diagnostic Tests Recommended by Day 3–5 for Prognostication
- SSEPs (if TTM-treated).
- Noncontrast CT/MRI for anoxic injury. EEG reactivity testing.
Strong Predictors of Poor Outcome
- Bilateral absent pupillary reflexes OR absent pupillary + corneal reflexes OR absent N20 waves on SSEP.
- Mnemonic: "3 Absents" (Pupils, Corneas, N20).
Counseling Families During Early Post-Arrest Care
- Avoid discussing prognosis before 72 hours due to sedation/TTM confounders.
- Emphasize multimodal testing (exam, EEG, SSEP, imaging) and avoid early DNR orders.
Institutional Framework for Successful Hypothermia Protocols
- A comprehensive post-arrest program spanning the ED, ICU, and rehab, with protocols for cooling, hemodynamic stability, and neuroprognostication.
Prehospital Cooling
- Trials show no benefit, and transport must prioritize avoiding rewarming en route.
- Cooling should only begin at facilities equipped to maintain TTM.
Role of NSE in Prognostication
- Higher levels correlate with poor outcomes, but thresholds vary.
- Use only in combination with clinical/EEG/imaging data.
Duration of Therapeutic Hypothermia
- Maintain for 24 hours at 33°C.
- A 48-hour duration showed no added benefit.
Critical Factors for ICU Management During Cooling
- Avoid hypotension/hypoxia.
- Lighten sedation gradually during rewarming.
- Minimize sedation by 72 hours for neurologic evaluation.
TTM Trials
- Both 33°C vs. 36°C are equally safe, but 33°C has stronger biologic evidence for neuroprotection
Impact of Status Myoclonus on Prognosis
- Status myoclonus <48 hours post-ROSC is a moderate predictor of poor outcome when combined with EEG/imaging abnormalities.
Final Step in the Hypothermia Protocol
- Remove sedation by 72 hours for neurologic evaluation and involve neurology for prognostication.
Mnemonics
- COLD SALINE: Cooling Initiated, Oxygenation maintained, Labs monitored, Devices (temperature probes), Sedation/Paralytics, Avoid blankets, Line (IV access), Infuse 2L cold saline, Neurologic monitoring, EEG/SSEP.
- 72-HOUR RULE: Prognostication requires 72 hours post-rewarming for reliable signs.
- SSEP Timing: "TTM patients: Post-rewarm or Day 3; Others: Day 2."
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.