Podcast
Questions and Answers
What is a primary consequence of increased sodium delivery to the collecting duct when loop diuretics inhibit salt reabsorption?
What is a primary consequence of increased sodium delivery to the collecting duct when loop diuretics inhibit salt reabsorption?
- Decreased sodium excretion
- Increased potassium reabsorption
- Decreased bicarbonate reabsorption
- Increased excretion of protons (H+) (correct)
Which of the following is NOT an adverse effect commonly associated with loop diuretics?
Which of the following is NOT an adverse effect commonly associated with loop diuretics?
- Hypoglycemia (correct)
- Hyperuricemia
- Hearing loss
- Hypokalemia
Which condition can potentially be reversed by potassium replacement and correction of hypovolemia?
Which condition can potentially be reversed by potassium replacement and correction of hypovolemia?
- Hypokalemic alkalosis (correct)
- Ototoxicity
- Hyperuricemia
- Hypomagnesemia
What causes the hypomagnesemia seen in patients using loop diuretics long-term?
What causes the hypomagnesemia seen in patients using loop diuretics long-term?
What potential cardiovascular risk is associated with acute hypovolemia caused by loop diuretics?
What potential cardiovascular risk is associated with acute hypovolemia caused by loop diuretics?
What mechanism accounts for the development of hyperuricemia due to loop diuretics?
What mechanism accounts for the development of hyperuricemia due to loop diuretics?
What is the primary mechanism by which loop diuretics increase urinary excretion of sodium and chloride?
What is the primary mechanism by which loop diuretics increase urinary excretion of sodium and chloride?
Which of the following is a consequence of loop diuretics affecting divalent cation reabsorption?
Which of the following is a consequence of loop diuretics affecting divalent cation reabsorption?
What impact do loop diuretics have on renal blood flow?
What impact do loop diuretics have on renal blood flow?
What is the duration of action of furosemide, a commonly used loop diuretic?
What is the duration of action of furosemide, a commonly used loop diuretic?
Which condition is NOT generally treated with loop diuretics?
Which condition is NOT generally treated with loop diuretics?
What is one of the adverse effects associated with the increased excretion of potassium due to loop diuretics?
What is one of the adverse effects associated with the increased excretion of potassium due to loop diuretics?
Which of the following statements about the pharmacokinetics of loop diuretics is TRUE?
Which of the following statements about the pharmacokinetics of loop diuretics is TRUE?
How do loop diuretics affect the transport of water in the collecting tubules?
How do loop diuretics affect the transport of water in the collecting tubules?
Which organ system predominantly mediates baroreflexes in the regulation of blood pressure?
Which organ system predominantly mediates baroreflexes in the regulation of blood pressure?
What percentage of hypertension cases are secondary to known organic diseases?
What percentage of hypertension cases are secondary to known organic diseases?
Which of the following treatment strategies for hypertension is often less effective in black patients?
Which of the following treatment strategies for hypertension is often less effective in black patients?
Mean arterial pressure is determined by which two factors?
Mean arterial pressure is determined by which two factors?
Which antihypertensive agents are typically favored for elderly patients?
Which antihypertensive agents are typically favored for elderly patients?
What are the two main control mechanisms involved in the regulation of blood pressure?
What are the two main control mechanisms involved in the regulation of blood pressure?
What is the primary aim of antihypertensive therapy?
What is the primary aim of antihypertensive therapy?
Secondary hypertension can be caused by which of the following conditions?
Secondary hypertension can be caused by which of the following conditions?
What is the primary mechanism through which diuretics increase urine output?
What is the primary mechanism through which diuretics increase urine output?
How do diuretics typically affect blood pressure in patients with hypertension?
How do diuretics typically affect blood pressure in patients with hypertension?
What class of diuretics is considered the most potent in terms of Na+ excretion?
What class of diuretics is considered the most potent in terms of Na+ excretion?
What effect does increased Na+ delivery to the distal nephron have on potassium and hydrogen secretion?
What effect does increased Na+ delivery to the distal nephron have on potassium and hydrogen secretion?
Which of the following describes a common clinical use of diuretics?
Which of the following describes a common clinical use of diuretics?
What is the mechanism of action of loop diuretics in the nephron?
What is the mechanism of action of loop diuretics in the nephron?
How does the efficacy of different classes of diuretics vary?
How does the efficacy of different classes of diuretics vary?
Which statement accurately reflects the interactions between diuretics and other antihypertensive agents?
Which statement accurately reflects the interactions between diuretics and other antihypertensive agents?
Which of the following statements about loop diuretics is true?
Which of the following statements about loop diuretics is true?
What is the primary mechanism by which thiazide diuretics achieve their effect?
What is the primary mechanism by which thiazide diuretics achieve their effect?
Which of the following statements is accurate regarding the diuretic effect of thiazides?
Which of the following statements is accurate regarding the diuretic effect of thiazides?
How do thiazide diuretics influence calcium reabsorption?
How do thiazide diuretics influence calcium reabsorption?
Which of the following thiazide diuretics can be administered parenterally?
Which of the following thiazide diuretics can be administered parenterally?
Which of the following is a shared characteristic of all thiazide diuretics?
Which of the following is a shared characteristic of all thiazide diuretics?
What factor significantly influences the secretion competition in thiazide diuretics?
What factor significantly influences the secretion competition in thiazide diuretics?
Which adverse effects are associated with loop diuretics?
Which adverse effects are associated with loop diuretics?
Study Notes
Secondary Hypertension
- Accounts for 10-15% of hypertension cases, linked to identifiable organic diseases like renovascular disease or pheochromocytoma.
- Treating the underlying condition often leads to a decrease in blood pressure.
Determinants of Arterial Pressure
- Mean Arterial Pressure = Cardiac Output x Peripheral Resistance.
- Influenced by heart rate, contractility, filling pressure, blood volume, venous tone, and arteriolar diameter.
Normal Regulation of Blood Pressure
- Blood pressure is regulated at four key sites: arterioles, postcapillary venules, heart, and kidneys.
- Regulation is managed primarily through baroreflexes (sympathetic nervous system) and the renin-angiotensin-aldosterone system.
Treatment Aims for Hypertension
- Goal is to reduce blood pressure to normal levels.
- Aim to decrease cardiovascular and renal morbidity and mortality.
Antihypertensive Agents
- Lower blood pressure via effects on peripheral resistance, cardiac output, or both.
- Act at arterioles, postcapillary venules, heart, and kidneys, disrupting normal blood pressure regulation mechanisms.
Treatment Strategies
- Match antihypertensive drugs to individual patient needs.
- Response varies by demographic: Black patients may benefit more from diuretics and calcium-channel blockers, whereas elderly patients may respond better to certain classes like ACE inhibitors and diuretics.
Diuretics
- Diuretics interfere with renal Na+ reabsorption across nephron sites, increasing sodium and water excretion, leading to reduced blood volume and lower blood pressure.
- Commonly used to manage fluid retention and hypertension, with effects varying by nephron segment.
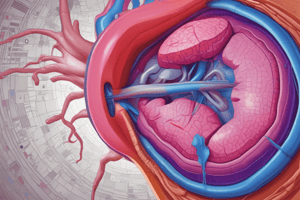
Loop Diuretics
- Agents include Bumetanide, Furosemide (prototype), Torsemide, and Ethacrynic acid.
- Most potent diuretics, targeting the thick ascending limb of the loop of Henle, can excrete 15-25% of filtered Na+.
- Mechanism involves inhibition of the Na+/K+/2Cl– transporter, leading to increased renal blood flow and reduced cardiac filling pressures.
Pharmacokinetics of Loop Diuretics
- Administered orally or parenterally, rapidly absorbed and eliminated by renal function.
- Duration of action: Furosemide (2-3 hours), Torsemide (4-6 hours).
Clinical Uses of Loop Diuretics
- Treatment for acute pulmonary edema, hypertension, severe hypercalcemia, hyperkalemia, acute renal failure, and anion overdoses.
Adverse Effects of Loop Diuretics
- Hypokalemic Metabolic Alkalosis: Caused by significant K+ wasting due to increased Na+ delivery to collecting ducts.
- Ototoxicity: Potential hearing loss, more prominent in patients with renal impairment or on ototoxic medications.
- Hypovolemia: Rapid volume reduction may lead to hypotension, shock, and arrhythmias.
- Hyperuricemia: Enhanced uric acid reabsorption due to hypovolemia.
- Hypomagnesemia: Magnesium depletion can result from chronic use, reversible with supplementation.
- Allergic Reactions: Possible cross-reactivity in sulfonamide-sensitive individuals, with skin rash or interstitial nephritis.
Thiazide Diuretics
- Key agents include Hydrochlorothiazide, Chlorothiazide, Metolazone, Chlorthalidone, and Indapamide.
- Function by blocking Na+/Cl– cotransporter in distal convoluted tubules, moderately effective (5-10% Na+ excretion).
Pharmacokinetics of Thiazide Diuretics
- Primarily administered orally; Chlorothiazide is also available parenterally.
- Compete with uric acid for excretion in proximal tubules.
Key Points on Thiazide Effects
- Enhance Ca2+ reabsorption by reducing intracellular Na+, leading to greater Na+/Ca2+ exchange and passive reabsorption.
- Moderate efficacy requiring careful monitoring for electrolyte balance.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the essentials of hypertension, including its secondary forms linked to identifiable diseases and key determinants of arterial pressure. Additionally, it explores the regulation of blood pressure and treatment aims, detailing various antihypertensive agents. Test your understanding of these critical concepts in cardiovascular health.