Podcast
Questions and Answers
What characteristic distinguishes cartilage from other connective tissues?
What characteristic distinguishes cartilage from other connective tissues?
- High concentration of mineral salts.
- Lack of blood vessels and lymphatics. (correct)
- Presence of abundant blood vessels.
- Presence of nerves.
Which component of the cartilage extracellular matrix (ECM) is primarily responsible for binding large amounts of water, providing resilience and cushioning?
Which component of the cartilage extracellular matrix (ECM) is primarily responsible for binding large amounts of water, providing resilience and cushioning?
- Proteoglycans (notably aggrecan) (correct)
- Chondroblasts
- Chondrocytes
- Collagen fibers
Which type of cartilage is characterized by its homogeneous and semitransparent fresh state, commonly found in articular surfaces of movable joints?
Which type of cartilage is characterized by its homogeneous and semitransparent fresh state, commonly found in articular surfaces of movable joints?
- Elastic cartilage
- Fibrocartilage
- Hyaline cartilage (correct)
- Reticular cartilage
Isogenous groups are a characteristic feature of which cartilage type?
Isogenous groups are a characteristic feature of which cartilage type?
Which type of collagen is predominantly found in hyaline cartilage providing tensile strength to the matrix?
Which type of collagen is predominantly found in hyaline cartilage providing tensile strength to the matrix?
What is the primary function of chondronectin in the hyaline cartilage matrix?
What is the primary function of chondronectin in the hyaline cartilage matrix?
Which characteristic primarily distinguishes elastic cartilage from hyaline cartilage?
Which characteristic primarily distinguishes elastic cartilage from hyaline cartilage?
Elastic cartilage is found in which of the following locations?
Elastic cartilage is found in which of the following locations?
What is a defining characteristic of fibrocartilage matrix, compared to hyaline and elastic cartilage?
What is a defining characteristic of fibrocartilage matrix, compared to hyaline and elastic cartilage?
In which locations is fibrocartilage typically found, reflecting its role in providing support and resistance to tensile forces?
In which locations is fibrocartilage typically found, reflecting its role in providing support and resistance to tensile forces?
How does interstitial growth contribute to the development of cartilaginous structures?
How does interstitial growth contribute to the development of cartilaginous structures?
What type of growth involves the formation of new chondroblasts from progenitor cells in the perichondrium?
What type of growth involves the formation of new chondroblasts from progenitor cells in the perichondrium?
Which factor significantly contributes to the slow and ineffective repair of cartilage?
Which factor significantly contributes to the slow and ineffective repair of cartilage?
What is the function of 'perforating (Sharpey) fibers' relating to bone?
What is the function of 'perforating (Sharpey) fibers' relating to bone?
During bone remodeling, which cells are primarily responsible for removing or resorbing existing bone tissue?
During bone remodeling, which cells are primarily responsible for removing or resorbing existing bone tissue?
What is the organic component of Bone Matrix mainly composed of?
What is the organic component of Bone Matrix mainly composed of?
What allows communication between osteocytes?
What allows communication between osteocytes?
What is the role of osteocalcin on bone matrix?
What is the role of osteocalcin on bone matrix?
What is the initial bone matrix secreted by osteoblasts called?
What is the initial bone matrix secreted by osteoblasts called?
What is released by osteoblasts to remove $PO4^-$ ions from matrix creating a high concentration of ions locally?
What is released by osteoblasts to remove $PO4^-$ ions from matrix creating a high concentration of ions locally?
What is the name of the structure that contains blood vessels and nerves?
What is the name of the structure that contains blood vessels and nerves?
What is the name of channels that allows osteons to communicate with each other?
What is the name of channels that allows osteons to communicate with each other?
What precent of of total bone mass is compact bone?
What precent of of total bone mass is compact bone?
Select the bones that are not formed by intramembranous ossification.
Select the bones that are not formed by intramembranous ossification.
What occurs during intramembranous ossification?
What occurs during intramembranous ossification?
What is the first step of endochondral ossification?
What is the first step of endochondral ossification?
What occurs at zone of proliferation of epiphyseal growth plate?
What occurs at zone of proliferation of epiphyseal growth plate?
What cell type deposits more bone at the periosteum, increasing bone diameter?
What cell type deposits more bone at the periosteum, increasing bone diameter?
What type of callus will form immediately after bone breakage?
What type of callus will form immediately after bone breakage?
What hormone inhibits osteoclast activity?
What hormone inhibits osteoclast activity?
A tissue sample shows chondrocytes within lacunae, surrounded by a clear, glassy matrix and without a perichondrium in the articular region. Which type of cartilage is this?
A tissue sample shows chondrocytes within lacunae, surrounded by a clear, glassy matrix and without a perichondrium in the articular region. Which type of cartilage is this?
A connective tissue is described as having high tensile strength, consisting of chondrocytes and thick bundles of collagen fibers, and located in the intervertebral discs. What type of cartilage matches this description?
A connective tissue is described as having high tensile strength, consisting of chondrocytes and thick bundles of collagen fibers, and located in the intervertebral discs. What type of cartilage matches this description?
Which of the following best describes the location and function of elastic cartilage?
Which of the following best describes the location and function of elastic cartilage?
During endochondral ossification, which event directly precedes the formation of the bony trabeculae?
During endochondral ossification, which event directly precedes the formation of the bony trabeculae?
Which description characterizes the main function of osteocytes?
Which description characterizes the main function of osteocytes?
What is the primary effect of parathyroid hormone (PTH) on bone tissue?
What is the primary effect of parathyroid hormone (PTH) on bone tissue?
Which type of bone is characterized by a random arrangement of collagen fibers and is typically found during fracture repair or in developing bone?
Which type of bone is characterized by a random arrangement of collagen fibers and is typically found during fracture repair or in developing bone?
In the context of bone remodeling, how do osteoblasts contribute to the process?
In the context of bone remodeling, how do osteoblasts contribute to the process?
How does appositional growth contribute to bone development?
How does appositional growth contribute to bone development?
Which zone of the epiphyseal plate is characterized by chondrocytes that are actively dividing and organized into distinct columns or stacks?
Which zone of the epiphyseal plate is characterized by chondrocytes that are actively dividing and organized into distinct columns or stacks?
In the epiphyseal growth plate, what key event takes place in the zone of calcified cartilage?
In the epiphyseal growth plate, what key event takes place in the zone of calcified cartilage?
Flashcards
Cartilage Function
Cartilage Function
A tough and resilient tissue that supports soft tissues, provides cushioned, low-friction surfaces in joints.
Chondroblasts
Chondroblasts
Cells that produce the extracellular matrix in cartilage.
Chondrocytes
Chondrocytes
Cartilage cells that maintain the matrix.
Cartilage ECM
Cartilage ECM
Signup and view all the flashcards
Perichondrium
Perichondrium
Signup and view all the flashcards
Hyaline Cartilage
Hyaline Cartilage
Signup and view all the flashcards
Isogenous Groups
Isogenous Groups
Signup and view all the flashcards
Chondronectin
Chondronectin
Signup and view all the flashcards
Elastic Cartilage
Elastic Cartilage
Signup and view all the flashcards
Fibrocartilage
Fibrocartilage
Signup and view all the flashcards
Interstitial Growth
Interstitial Growth
Signup and view all the flashcards
Appositional Growth
Appositional Growth
Signup and view all the flashcards
Bone / Osseous Tissue
Bone / Osseous Tissue
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Osteoid
Osteoid
Signup and view all the flashcards
Osteocalcin
Osteocalcin
Signup and view all the flashcards
Hydroxyapatite
Hydroxyapatite
Signup and view all the flashcards
Osteocytes
Osteocytes
Signup and view all the flashcards
Osteoclasts
Osteoclasts
Signup and view all the flashcards
Periosteum
Periosteum
Signup and view all the flashcards
Perforating Fibers
Perforating Fibers
Signup and view all the flashcards
Endosteum
Endosteum
Signup and view all the flashcards
Osteon / Haversian System
Osteon / Haversian System
Signup and view all the flashcards
Lacunae
Lacunae
Signup and view all the flashcards
Canaliculi
Canaliculi
Signup and view all the flashcards
Perforating Canals / Volkmann Canals
Perforating Canals / Volkmann Canals
Signup and view all the flashcards
Interstitial Lamellae
Interstitial Lamellae
Signup and view all the flashcards
Woven Bone
Woven Bone
Signup and view all the flashcards
Lamellar Bone
Lamellar Bone
Signup and view all the flashcards
Compact (Cortical) Bone
Compact (Cortical) Bone
Signup and view all the flashcards
Cancellous (Trabecular) Bone
Cancellous (Trabecular) Bone
Signup and view all the flashcards
Osteogenesis
Osteogenesis
Signup and view all the flashcards
Intramembranous Ossification
Intramembranous Ossification
Signup and view all the flashcards
Endochondral Ossification
Endochondral Ossification
Signup and view all the flashcards
Bone Collar Formation
Bone Collar Formation
Signup and view all the flashcards
Primary Ossification Center
Primary Ossification Center
Signup and view all the flashcards
Secondary Ossification Center
Secondary Ossification Center
Signup and view all the flashcards
Appositional Bone Growth
Appositional Bone Growth
Signup and view all the flashcards
Calcium
Calcium
Signup and view all the flashcards
Parathyroid hormone (PTH)
Parathyroid hormone (PTH)
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
Study Notes
Cartilage
- Tough and resilient, cartilage supports soft tissues
- Cushioned, low-friction surfaces in joints provided by cartilage
- Cartilage cells comprised of chondroblasts and chondrocytes
- The cartilage extracellular matrix (ECM) includes collagen and proteoglycans
- Aggrecan binds large amounts of water
Cartilage Characteristics
- Cartilage lacks blood vessels, lymphatics, and nerves
- Perichondrium, a dense connective tissue, usually surrounds cartilage and is vascularized
Forms of Cartilage
- There are 3 forms of cartilage: hyaline, elastic, and fibrocartilage
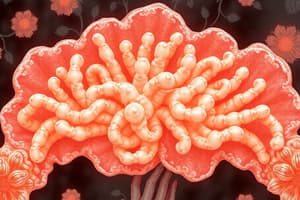
Hyaline Cartilage
- The most common type of cartilage, it is homogeneous and semitransparent in the fresh state
- In adults, it's located in articular surfaces of movable joints
- Hyaline cartilage is also located in the walls of larger respiratory passages (nose, larynx, trachea, bronchi)
- Hyaline cartilage is located in the ventral ends of the ribs, epiphyseal plates of long bones, and as a temporary skeleton in the embryo
- The ECM has less collagen and more proteoglycan immediately around the lacunae -This produces slight staining differences in this territorial matrix.
- Chondrocytes occur singly or in small, mitotically derived isogenous groups
- Perichondrium is usually present, except at the hyaline cartilage of articular surfaces or the epiphyses of growing long bones.
Hyaline Cartilage Matrix
- The matrix is 40% collagen embedded in a firm, hydrated gel of proteoglycans and glycoproteins
- Type II collagen is present
- Aggrecan, the most abundant proteoglycan in HC, is present
- Chondronectin, a multiadhesive glycoprotein, is present
- Chondronectin binds specifically to GAGs, collagen, integrins to mediate chondrocyte adherence to the ECM
Perichondrium
- Essential for growth and maintenance of cartilage
- Outer region consists largely of collagen
- Type I fibers and fibroblasts
- The inner layer adjoining the cartilage matrix contains mesenchymal stem cells
- Mesenchymal stem cells provide a source for new chondroblasts that divide and differentiate into chondrocytes.
Elastic Cartilage
- Resembles hyaline cartilage in chondrocytes and major ECM components
- Matrix includes abundant fibers, visible with special stains, which increase flexibility
- Possesses a perichondrium.
- Elastic cartilage provides flexible support for the external ear
- It also supports structures of the middle ear, the epiglottis and the larynx
Fibrocartilage
- Contains combinations of hyaline cartilage in small amounts of dense connective tissue
- Provides strong support at tendon insertions, in intervertebral discs and certain joints
- Consists of small chondrocytes in a scant matrix with thick, parallel bundles of type I collagen fibers
- Found in areas requiring support and tensile strength
- Lacks a perichondrium
Cartilage Formation
- All forms of cartilage form from embryonic mesenchyme
- Cartilaginous structures grow by mitosis of existing chondroblasts in lacunae
- This is known as "interstitial growth" and is important in increasing length of long bones
- New chondroblasts form peripherally from progenitor cells in the perichondrium
- This is "appositional growth" and is important in postnatal development
- Repair or replacement of injured cartilage is very slow and ineffective
- This is due in part to the tissue's avascularity and low metabolic rate
Bone
- Bone/Osseous tissue, a specialized type of connective tissue
- Characterized by a calcified extracellular matrix
- Bone supports the body and protects many internal organs
- It acts as a reservoir of calcium and phosphate
Bone Cells: Osteoblasts
- They originate from mesenchymal stem cells
- Growing cells which synthesize and secrete the organic components of the matrix
- These components are collagen, proteoglycans, glycoproteins (osteonectin)
- Osteoblasts secrete components of the initial matrix called osteoid, which allow matrix mineralization to occur
Osteoid
- A layer of unique collagen material is between the osteoblast layer and preexisting bone surface
- Key components include type I collagen and osteocalcin, the protein, which binds Ca2+
- Matrix vesicles that contain enzymes generating PO4- are also present in osteoid
- High concentrations of Ca2+ and PO4− ions cause formation of hydroxyapatite crystals, -Their growth gradually calcifies the matrix
Osteoblast Activity
- Secrete type I collagen, several glycoproteins, and proteoglycans
- Secrete osteocalcin and certain glycoproteins
- These glycoproteins bind Ca2+ with high affinity and raising local concentration
- Release very small membrane-enclosed matrix vesicles which contain alkaline phosphatase and other enzymes
- The included enzymes remove PO4− ions from various matrix macromolecules
- This process creates a high concentration of these ions locally
Bone Matrix Mineralization
- High Ca2+ and PO4− ion concentrations will cause calcified nanocrystals to form in and around the matrix vesicles
- The crystals grow and mineralize further; Forming small growing masses of calcium hydroxyapatite
- These masses surround the collagen fibers and all other macromolecules
- Masses of hydroxyapatite merge as a confluent solid bony matrix as calcification of the matrix is completed
Bone Cells: Osteocytes
- Osteoblasts gradually surround themselves, and their own secretion differentiates into osteocytes
- Enclosed singly within spaces (lacunae)
- Occurs throughout the mineralized matrix
- Osteocytes maintain the calcified matrix and detect mechanical stresses on bone
- Osteocytes maintain communication with adjacent cells via gap junctions at the ends of their processes
Bone Cells: Osteoclasts
- Giant, multinucleated cells
- Involved in removing calcified bone matrix and remodeling bone tissue
- Formed by fusion of several blood monocytes
- Activity controlled by hormones and local factors
Bone Matrix Composition
- Inorganic materials consist of:
- Hydroxyapatite, bicarbonate, citrate, magnesium, potassium and sodium ions
- Organic materials consist of:
- Type I Collagen
- Ground Substance
- Proteoglycans
- Glycoproteins (osteonectin, osteocalcin)
Periosteum
- A dense connective tissue layer on the outer surface of bone
- Bound to bone matrix by bundles of type I collagen
- These bundles are called perforating (or Sharpey) fibers
- Regions of periosteum adjacent to bone are rich in osteoprogenitor cells and osteoblasts
- These cells mediate increases in bone thickness by appositional growth
Endosteum
- A thin layer of active and inactive osteoblasts lining all the internal surfaces within bone
- Osteoblasts are required for bone growth
Woven Bone
- Exhibits random distribution of type I collagen fibers
- Woven Bone features a lower mineral content
- First bone tissue to appear in embryonic development and fracture repair.
- Temporary and replaced by lamellar bone in adults
- Except in very few places in the body
Lamellar Bone
- Both compact and cancellous bone are lamellar bone
- Lamellae are organized concentrically around small central canals
- Canals containing blood vessels and nerves (osteon or haversian system)
Osteon/Haversian System
- Refers to the complex of concentric lamellae surrounding a central canal
- Includes small blood vessels, nerves, and endosteum
- Between each lamellae are lacunae with osteocyte, all interconnected by the canaliculi
Perforating Canals/Volkmann Canals
- Allow canals to communicate with one another
- Features only a few concentric lamellae
Interstitial Lamellae
- Numerous irregularly shaped groups of parallel lamellae
- Can arise from remaining osteons
- Partially destroyed by osteoclasts during growth and remodeling of bone
Compact bone
- Dense area near the surface
- Accounts for 80% of the total bone mass
Cancellous Bone
- Deeper areas with numerous interconnecting cavities
- Accounts for 20% of total bone mass
Osteogenesis
- Bone formation occurs via intramembranous and endochondral ossification
Intramembranous Ossification
- Osteoblasts differentiate directly from progenitor cells in condensed "membranes” of mesenchyme
- Key examples of Intramembranous Ossification include the bones of the skull and jaw
Endochondral Ossification
- A preexisting matrix of hyaline cartilage is eroded and invaded by osteoblasts
- The osteoblasts then begin osteoid production
- Most bones are formed this way
Intramembranous Ossification Characteristics
- Takes place within condensed sheets (“membranes”) of embryonic mesenchymal tissue
- Examples: bones of the skull and jaw, scapula, clavicle
Endochondral Ossification Characteristics
- Occurs within hyaline cartilage and forms most bones of the body
Endochondral Ossification Phases
- Cartilage Model Formation
- Bone Collar Formation
- Primary Ossification Center
- Secondary Ossification Center
- Bone replace cartilage except the articular cartilage and epiphyseal plates.
- Epiphyseal plates ossify and form epiphyseal lines
Processes During Bone Collar Formation
- Perichondrium becomes periosteum
- Osteoblasts produce compact bone on the surface
- There is an increased size of cartilage through Interstitial growth and appositional growth
- Further increased size from Hypertrophy of chondrocytes
- Chondrocytes initiate formation of hydroxyapatite crystals, also known as calcified matrix
Further Clarification on Endochondral Ossification
- Blood vessels grow into the enlarged lacunae of the calcified cartilage
- The osteoclasts remove any remaining cartilage matrix
- Osteoblasts replace the dying chondrocytes and secrete its component in the calcified matrix to form the trabeculae
Cartilage Remaining
- Articular cartilage remains within the joints between long bones; Normally persists through adult life
- Epiphyseal cartilage (epiphyseal plate or growth plate) is specially organized
- It connects each epiphysis to the diaphysis and allows longitudinal bone growth
Epiphyseal Plate
- Contains a zone of reserve cartilage composed of typical hyaline cartilage
- The zone of proliferation is where chondrocytes undergo mitosis and appear stacked within elongated lacunae
- In the Zone of Hypertrophy mature chondrocytes in these lacunae swell up
- They compress the matrix, and undergo apoptosis
- In the Zone of Calcified Cartilage chondrocytes about to undergo apoptosis release matrix vesicles and osteocalcin to begin matrix calcification by the formation of hydroxyapatite crystals
- The Zone of Ossification is where bone tissue first appears
- Further, woven bone is laid down initially by osteoblasts and remodeled into lamellae bone
Appositional Bone Growth
- Increases the circumference of a bone by osteoblast activity at the periosteum
- The process is accompanied by enlargement of the medullary marrow cavity
Bone Growth
- Occurs throughout life
- Cells & matrix turn over continuously
- Accomplished through activities of osteoblasts and osteoclasts
- Lamellae and osteons are temporary structures replaced and rebuilt continuously
- This is bone remodeling, in which bones can change size and shape according to mechanical stress
Bone Repair
- Soft, fibrocartilage-like callus – initial bone formation which involves the activation of periosteal fibroblasts after fracture or other injury
- Hard callus of woven bone – replaces the soft callus and this is soon remodeled to produce stronger lamellar bone
Calcium
- A key ion for all cells
- Stored in bone when dietary calcium is adequate
- Mobilized from bone when dietary calcium is deficient
Calcium Importance
- Maintenance of proper blood calcium levels involves the activity of all three major bone cells
- Regulated by subtle paracrine interaction among these and other cells
- Hormones affecting calcium deposition and removal from bone include:
- Parathyroid hormone (PTH)
- Indirectly stimulates osteoclasts to elevate levels of calcium in blood
- Calcitonin
- Serves to inhibit osteoclast activity, lowering blood calcium levels
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.