Podcast
Questions and Answers
What condition is indicated by a decrease in everything?
What condition is indicated by a decrease in everything?
- Respiratory acidosis
- Metabolic alkalosis
- Respiratory alkalosis
- Metabolic acidosis (correct)
Which organ is primarily involved in the excretion of ammonia?
Which organ is primarily involved in the excretion of ammonia?
- Liver
- Lungs
- Kidneys (correct)
- Heart
Which condition could result in central respiratory failure?
Which condition could result in central respiratory failure?
- Hypoventilation
- Hyperventilation
- Metabolic alkalosis
- Respiratory acidosis (correct)
What is a common effect of ammonia in the body?
What is a common effect of ammonia in the body?
Which gas exchange structure is involved in the respiratory system?
Which gas exchange structure is involved in the respiratory system?
What is a primary condition associated with ammonia in the body?
What is a primary condition associated with ammonia in the body?
Which organ plays a crucial role in the handling of ammonia?
Which organ plays a crucial role in the handling of ammonia?
What effect does metabolic acidosis have on bodily functions?
What effect does metabolic acidosis have on bodily functions?
In which situation would respiratory failure likely occur?
In which situation would respiratory failure likely occur?
What is a likely consequence of an increase in ammonia levels in the body?
What is a likely consequence of an increase in ammonia levels in the body?
Flashcards
Acidosis
Acidosis
A type of acid-base imbalance where the body has too much acid.
Alveoli
Alveoli
The tiny air sacs in the lungs where gas exchange (oxygen and carbon dioxide) occurs.
Metabolic Acidosis
Metabolic Acidosis
A condition where the blood has a lower-than-normal pH due to a buildup of acid.
Renal Tubule
Renal Tubule
Signup and view all the flashcards
Respiratory System
Respiratory System
Signup and view all the flashcards
Study Notes
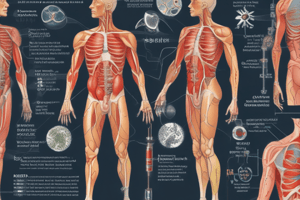
Human Urinary System - Acid-Base Regulation
- Learning Objectives: Students should be able to define pH, acidosis, alkalosis, volatile and fixed acids; discuss how the body defends against pH changes (blood buffers, respiratory system, kidneys); and provide examples of acid-base balance pathophysiology.
Definitions
- Hydrogen Ions (H+): Source of acidity in blood.
- pH: Potential of H+ ion concentration in body fluids. Arterial blood pH is 7.35-7.45.
- Buffer: Agent that prevents or minimizes pH change when acid or base is added. Buffers consist of a weak acid and its salt, or a weak base and its salt. They reversibly bind or release H+ ions.
Acid-Base Balance
- Normal Arterial Blood pH: 7.35-7.45
- Acidosis: pH below 7.35
- Alkalosis: pH above 7.45
- Incompatibility with Life: pH below 6.8 or above 7.8
- Fixed Acids: Sulphuric acid, phosphoric acid, and ammonia. Needing the kidneys for excretion.
- Volatile Acid: Carbon dioxide (CO2). Excreted by the lungs.
Urine pH
- Filtrate Acidification: Kidneys acidify glomerular filtrate from a pH of 7.4 to approximately 6.
- Urine pH Range: Depending on acid-base balance, urine pH can range from 4.5 to 8.0 (normal average is about 6.0).
CO2 (Respiratory Factor) and Bicarbonate (HCO3-) (Metabolic Factor)
- CO2 Importance: Important source of acid and bicarbonate (alkali).
- CO2 Tension (Partial Pressure): Normal arterial CO2 tension (PaCO2) is 38-42 mmHg.
- HCO3- Concentration: Normal arterial HCO3- concentration is 22-28 mEq/L(average 24 meq/L).
- CO2 as Acid & HCO3- as Alkali: Practical purposes, CO2 is considered acid because dissolved CO2 creates carbonic acid(H2CO3). HCO3- is an alkali.
- Respiratory Factor: CO2
- Metabolic Factor: HCO3-
Respiratory Regulation of Acid-Base Balance
- Mechanism: Control pH via CO2 removal or retention.
- Time Frame: Acts within seconds or fraction of a second; relatively short-term response.
- Increase in PaCO2: Respiratory acidosis (e.g., hypoventilation).
- Decrease in PaCO2: Respiratory alkalosis (e.g., hyperventilation).
- [H+] affects Alveolar Ventilation: Lower pH increases ventilation rate 4-5 times, while higher pH decreases it.
- Negative Feedback: Respiratory system acts as a negative feedback to control [H+].
Renal Regulation of Acid-Base Balance
- Mechanism: Slow, but powerful (days or more) buffering mechanism. Kidneys can secrete acidic or alkaline urine to regulate blood pH.
- HCO3- Filtration: Continuously filtering HCO3- into tubules.
- Buffering Systems: Employing bicarbonate, phosphate, and ammonia buffering mechanisms.
- Renal Bicarbonate Buffering: Three mechanisms include H+ secretion, HCO3- reabsorption, and new bicarbonate ion production, all situated in distal tubules and collecting ducts.
- Renal Phosphate Buffering: Intracellular and renal tubular fluid buffer. Components are H2PO4- and HPO42-.HCI (strong acid) is replaced by the weaker NaH2PO4, minimizing pH decrease.
- Ammonia (NH3) Buffering: Ammonia ionizes, forming ammonium ion (NH4+), which is a useful buffer. Decreased ECF pH stimulates glutamine metabolism, leading to more NH4+ and HCO3- production. For every glutamine molecule that's metabolized, 2 new HCO3- ions are created.
Compensatory Mechanisms
- Respiratory Acidosis: Kidneys increase plasma HCO3- levels (compensatory mechanism).
- Metabolic Acidosis: Increase in ventilation and kidneys make new HCO3- (compensatory mechanism).
- Respiratory Alkalosis: Increased renal excretion of HCO3- (compensatory mechanism).
- Metabolic Alkalosis: Decreased Ventilation, increased CO2, and increased renal excretion of HCO3− (compensatory mechanism).
Pathophysiology - Example (Respiratory Acidosis)
- Condition: Decreased ventilation (hypoventilation) increases CO2 and causes acidosis (PaCO2 over 45mmHg, pH under 7.35).
- Common Causes: Acute pulmonary edema (excess fluid in lungs), other conditions like pneumonia
- Symptoms: Dyspnea ("shortness of breath"), suffocating or drowning feelings, wheezing, gasping, cyanosis ("bluish skin"), cough with frothy sputum, and possibly blood tinged. Central bat-wing pattern observed on chest X-rays can be a sign of respiratory acidosis.
- Significance: Medical emergency, requiring prompt attention to restore proper ventilation and respiratory function.
Pathophysiology - Example (Respiratory Alkalosis)
- Condition: Excessive anxiety or hyperventilation reduces CO2, causing alkalosis (PaCO2 under 35 mmHg, pH over 7.45).
- Symptoms: Extreme worry, anxiety, agitation, panic, confusion, weakness, or dizziness.
- Physiology: Reduced CO2 in blood reduced blood flow to the brain, resulting in nervous system/emotional symptoms.
Pathophysiology - Example (Metabolic Acidosis)
- Condition: Often caused by renal failure or other metabolic disturbances; imbalance in acid-base homeostasis leads to a decrease in blood pH (below 7.35).
- Symptoms: Increased heart rate, rapid breathing, fatigue, muscle pain, mental confusion, edema (e.g. facial puffiness or swelling in lower limbs), headache, sleepiness, loss of appetite, further complications
- Physiology: Respiratory compensation leads to a decrease in PaCO2 (below 35 mmHg) to counteract the metabolic acidosis. HCO3- levels in the blood are also decreased.
Pathophysiology - Example (Metabolic Alkalosis)
- Condition: Increases in blood bicarbonate (HCO3−) often occur with prolonged vomiting, excessive ingestion of antacids, or other conditions. Blood pH becomes elevated.
- Symptoms: Hand tremors, nausea, vomiting, and numbness or tingling in face, hands, and/or feet, further complications
- Physiology: The cause is an increase in blood HCO3− concentration (typically above 28mEq/L), often coupled with a lower than normal level of blood CO2 as the body tries to compensate resulting changes toward metabolic alkalosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.