Podcast
Questions and Answers
What is the primary role of Pinopodes during implantation?
What is the primary role of Pinopodes during implantation?
- They initiate the process of decidualization.
- They promote the differentiation of trophoblasts.
- They release hormones to support the embryo.
- They facilitate contact and adherence between the blastocyst and uterine cells. (correct)
What factors trigger the formation of decidual cells in the endometrium?
What factors trigger the formation of decidual cells in the endometrium?
- Age of the mother.
- Signals from the developing embryo. (correct)
- Environmental factors.
- Maternal hormones only.
Which of the following is NOT considered a symptom of implantation?
Which of the following is NOT considered a symptom of implantation?
- Abdominal pain.
- Severe headaches. (correct)
- Increased urge to urinate.
- Implantation bleeding.
What is the first step in placenta development after the embryo enters the uterus?
What is the first step in placenta development after the embryo enters the uterus?
What is a characteristic of the cleavage stage in cell division?
What is a characteristic of the cleavage stage in cell division?
What is the purpose of cleavage in embryonic development?
What is the purpose of cleavage in embryonic development?
What type of implantation involves the blastocyst invading the uterine lining?
What type of implantation involves the blastocyst invading the uterine lining?
How many cells does the embryo consist of after the 3rd cleavage stage?
How many cells does the embryo consist of after the 3rd cleavage stage?
Which component of the placenta faces the fetus?
Which component of the placenta faces the fetus?
What characteristic distinguishes the Syncitiotrophoblast from the Cytotrophoblast?
What characteristic distinguishes the Syncitiotrophoblast from the Cytotrophoblast?
What is the size of the embryo throughout the early cleavage stages?
What is the size of the embryo throughout the early cleavage stages?
What is the primary function of the placenta during pregnancy?
What is the primary function of the placenta during pregnancy?
How long does it typically take for one cleavage cycle to occur in humans?
How long does it typically take for one cleavage cycle to occur in humans?
What happens to the DNA content during the cleavage stages?
What happens to the DNA content during the cleavage stages?
What is observed regarding the synchronization of cleavage in human embryos?
What is observed regarding the synchronization of cleavage in human embryos?
What significant structural change occurs after the morula stage during cleavage?
What significant structural change occurs after the morula stage during cleavage?
What is the role of E-cadherin during the compaction process of the human embryo?
What is the role of E-cadherin during the compaction process of the human embryo?
What happens if cells are treated with anti-cadherin before compaction?
What happens if cells are treated with anti-cadherin before compaction?
What is cavitation in relation to embryo development?
What is cavitation in relation to embryo development?
What is the significance of the hatching of the blastocyst?
What is the significance of the hatching of the blastocyst?
What is a potential consequence of impaired hatching of the blastocyst?
What is a potential consequence of impaired hatching of the blastocyst?
What is meant by nidation in the context of embryo development?
What is meant by nidation in the context of embryo development?
Which of the following processes occurs to enable the blastocyst to hatch?
Which of the following processes occurs to enable the blastocyst to hatch?
What fluid-filled structure is produced during the process of cavitation?
What fluid-filled structure is produced during the process of cavitation?
What is the initial phase of cell division after fertilization called?
What is the initial phase of cell division after fertilization called?
During cleavage, what term is used to refer to the newly formed cells?
During cleavage, what term is used to refer to the newly formed cells?
What characterizes the cell divisions during cleavage?
What characterizes the cell divisions during cleavage?
Which of the following developmental processes results in the organization of cells, tissues, and organs?
Which of the following developmental processes results in the organization of cells, tissues, and organs?
What happens to the size of cells during the cleavage stage?
What happens to the size of cells during the cleavage stage?
Which type of cleavage involves completely separate cells?
Which type of cleavage involves completely separate cells?
What is a key event that continues until the blastocyst is hatched?
What is a key event that continues until the blastocyst is hatched?
During the first 7 days after fertilization, what structure is formed that is ready for implantation?
During the first 7 days after fertilization, what structure is formed that is ready for implantation?
What is the main role of pinopodes during the window of implantation?
What is the main role of pinopodes during the window of implantation?
What process refers to the transformation of the endometrium to prepare for implantation?
What process refers to the transformation of the endometrium to prepare for implantation?
During which days does the window of implantation occur in humans?
During which days does the window of implantation occur in humans?
What is the significance of receptor-ligand interactions during implantation?
What is the significance of receptor-ligand interactions during implantation?
What characterizes the process of decidualization in the endometrium?
What characterizes the process of decidualization in the endometrium?
What is the main function of the decidua during implantation?
What is the main function of the decidua during implantation?
What cellular feature marks the receptivity of the endometrium?
What cellular feature marks the receptivity of the endometrium?
What does the presence of increased levels of human chorionic gonadotropin (hCG) indicate?
What does the presence of increased levels of human chorionic gonadotropin (hCG) indicate?
The window of implantation corresponds with which phase of the menstrual cycle?
The window of implantation corresponds with which phase of the menstrual cycle?
Which stage of development must the embryo reach before successful implantation?
Which stage of development must the embryo reach before successful implantation?
What condition must the endometrium meet for successful embryo implantation?
What condition must the endometrium meet for successful embryo implantation?
What happens to the endometrium if implantation does not occur?
What happens to the endometrium if implantation does not occur?
Where is the most common site for implantation within the uterus?
Where is the most common site for implantation within the uterus?
What role do estrogens and progesterone play in relation to the endometrium?
What role do estrogens and progesterone play in relation to the endometrium?
What is the role of the trophoectoderm in a developing embryo?
What is the role of the trophoectoderm in a developing embryo?
What must occur before the blastocyst can implant successfully?
What must occur before the blastocyst can implant successfully?
Flashcards
Cleavage
Cleavage
The initial divisions of a zygote resulting in a multicellular embryo.
Blastomeres
Blastomeres
The cells created during cleavage are called blastomeres.
Mitotic Divisions in Cleavage
Mitotic Divisions in Cleavage
Cleavage is a special type of cell division that maintains the original chromosome number.
Rapid Cell Divisions with No Growth
Rapid Cell Divisions with No Growth
Signup and view all the flashcards
Cell Size Reduction
Cell Size Reduction
Signup and view all the flashcards
Holoblastic Cleavage
Holoblastic Cleavage
Signup and view all the flashcards
First Seven Days of Development
First Seven Days of Development
Signup and view all the flashcards
Four Major Developmental Events
Four Major Developmental Events
Signup and view all the flashcards
Decidualization
Decidualization
Signup and view all the flashcards
Pinopodes
Pinopodes
Signup and view all the flashcards
Window of Implantation
Window of Implantation
Signup and view all the flashcards
Plasma Membrane Transformation
Plasma Membrane Transformation
Signup and view all the flashcards
Implantation
Implantation
Signup and view all the flashcards
Decidual Cells
Decidual Cells
Signup and view all the flashcards
Receptor-Ligand Interactions
Receptor-Ligand Interactions
Signup and view all the flashcards
Decidua
Decidua
Signup and view all the flashcards
Compaction
Compaction
Signup and view all the flashcards
Blastocoel
Blastocoel
Signup and view all the flashcards
Hatching
Hatching
Signup and view all the flashcards
E-cadherin
E-cadherin
Signup and view all the flashcards
Embryoblast
Embryoblast
Signup and view all the flashcards
Trophoblast
Trophoblast
Signup and view all the flashcards
Cavitation
Cavitation
Signup and view all the flashcards
hCG (Human Chorionic Gonadotropin)
hCG (Human Chorionic Gonadotropin)
Signup and view all the flashcards
Endometrium
Endometrium
Signup and view all the flashcards
Blastocyst stage
Blastocyst stage
Signup and view all the flashcards
Zona pellucida
Zona pellucida
Signup and view all the flashcards
Site of implantation
Site of implantation
Signup and view all the flashcards
Receptive endometrium
Receptive endometrium
Signup and view all the flashcards
Menstruation
Menstruation
Signup and view all the flashcards
Purpose of Cleavage: Multicellularity
Purpose of Cleavage: Multicellularity
Signup and view all the flashcards
Purpose of Cleavage: Identical Cells
Purpose of Cleavage: Identical Cells
Signup and view all the flashcards
Stages of Early Cleavage
Stages of Early Cleavage
Signup and view all the flashcards
1st Cleavage
1st Cleavage
Signup and view all the flashcards
2nd Cleavage
2nd Cleavage
Signup and view all the flashcards
3rd Cleavage
3rd Cleavage
Signup and view all the flashcards
What are Pinopodes?
What are Pinopodes?
Signup and view all the flashcards
What is Decidualization?
What is Decidualization?
Signup and view all the flashcards
How does the embryo impact Decidualization?
How does the embryo impact Decidualization?
Signup and view all the flashcards
What is the Trophoblast?
What is the Trophoblast?
Signup and view all the flashcards
What is the Syncitiotrophoblast?
What is the Syncitiotrophoblast?
Signup and view all the flashcards
What is the Cytotrophoblast?
What is the Cytotrophoblast?
Signup and view all the flashcards
What is the Placenta?
What is the Placenta?
Signup and view all the flashcards
How is the Placenta formed?
How is the Placenta formed?
Signup and view all the flashcards
Study Notes
Human Embryonic and Fetal Development
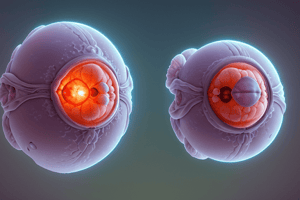
- The image displays various stages of human embryonic and fetal development.
- The stages show the fertilized egg, 2-cell stage, 4-cell stage, 8-cell stage, 16-cell stage, blastocyst and subsequent fetal development stages at 4 weeks, 10 weeks, 16 weeks, and 20 weeks.
- The images show the progression in size and development during the early stages.
Early Development: Cleavage Lecture
- Four major developmental events occur in human embryogenesis:
- Cell division (cleavage)
- Cell differentiation
- Morphogenetic events
- Growth
- Cleavage is the initial mitotic divisions converting the single-celled zygote to a multicellular embryo.
- Blastomeres are the cells produced during cleavage.
- Mitotic divisions during cleavage maintain the 2N complement (number of chromosomes) without growth phases, leading to smaller cells over time.
The Timing of Early Development
- Development from Day 0-35 after fertilization
- Days 0-7: fertilization, cleavage, and blastocyst formation
- Days 8-14: implantation
- Days 15-21: gastrulation, formation of somites, and vascular systems
- Days 22-28: neurulation, neural crest migration, and development of various organ systems
- Days 28-35: further development of systems including nervous system, limbs, and genitalia
Cleavage: Functions & Events
- Cleavage involves initial divisions transforming the zygote into a multicellular embryo.
- During cleavage the cells are called "Blastomeres"
- These divisions, mitotic divisions, maintain the chromosome number (2N) without intervening growth phases.
- The result is smaller cells over time.
- Complete separation of cells in holoblastic cleavage.
Mitotic vs. Normal Cell Cycle
- During cleavage, the cells progress directly from S stage (DNA synthesis) to M stage (mitosis) without the interphase growth phases (G1 and G2).
- This results in cleavages continuing to decrease in size approximating the size of somatic cells.
The Purposes of Cleavage
- Cleavage converts the zygote from a single cell to many cells.
- It generates many cells that interact and can be moved around the embryo.
- It maintains the diploid chromosome complement across all the cells, ensuring genetic fidelity via synchronous divisions that are not identical in timing.
- Embryos with differing numbers of cells at various points in time are a result.
- No growth during cleavage; the total embryo will remain about 100 microns in diameter.
The Stages of Early Cleavage
- Cleavage begins approximately 24 hours after fertilization.
- The images show the 2-cell stage, 4-cell stage, and 8-cell stage, etc.
- The process is not synchronous (all cells do not divide exactly at the same time).
Mammalian Compaction
- Compaction is a process occurring at the 8-cell stage.
- Cells adhere more tightly together, becoming more compact.
- E-cadherin, an adhesion protein, appears at the time of compaction, causing tighter cell adhesion.
Formation of the Blastocyst
- The formation of the blastocyst from the morula involves accumulation of fluid forming the blastocoele.
- The fluid-filled cavity within the blastocyst is called the blastocoel.
- The blastocyst consists of an outer layer of cells called the trophoblast and an inner cell mass.
Hatching of the Blastocyst
- Hatching takes place just prior to implantation.
- The blastocyst secretes proteases, which digest components (e.g., zona pellucida), allowing the blastocyst to free itself.
- Hatching is crucial for the blastocyst to implant in the uterine wall.
Embryo Implantation, Process & Their Stages
- The process of implantation involves several stages, from initial hatching through apposition, adhesion, and invasion.
- Specific time frames within the implantation window are critical for successful implantation, with a limited window of receptivity.
Implantation (Process)
- Implantation is a crucial stage converting a blastocyst into a functional embryo.
- It involves multiple phases: hatching, pre-contact, apposition, adhesion, and invasion. This allows the embryo to attach and invade the uterine wall (endometrium).
Factors Related to the Embryo
- The embryo must reach the blastocyst stage to implant.
- The embryo consists of an internal cell mass and a trophoectoderm.
- The trophoectoderm forms the placenta and other attachments.
- Implantation requires the blastocyst to detach from the zona pellucida, grow to full size and achieve maximum expansion before implantating.
Factors Related to the Endometrium
- The endometrium, the innermost lining of the uterus, must be receptive to allow for successful implantation.
- Its thickness (between 7-10 mm) and specific trilaminar aspect indicate receptivity.
- The endometrium's receptivity is influenced by hormonal changes during the menstrual cycle.
When Does Implantation Occur?
- Implantation will only occur when the endometrium has become receptive.
- This receptive period, the window of implantation, lasts for about 4 days in most women, typically between days 19-21 of the menstrual cycle.
Phases of Implantation
- Implantation is a process that consists of specific steps. These are adhesion, apposition, and invasion. The diagram details the stages beginning with the hatching blastocyst.
- Adhesion molecules bind the blastocyst to the endometrial lining.
- During apposition, a close relationship between the embryo and the uterine lining is established.
- Invasion occurs when the trophoblast cells of the embryo penetrate into the uterine lining.
Symptoms of Implantation
- Implantation-related symptoms are not always observable, although certain signs including light bleeding, breast swelling, abdominal pain, or a heightened urge to urinate may occur.
Placenta Development
- The placenta forms from the invasion and merging of the syncitiotrophoblast and endometrial cells.
- It's a disc-shaped organ consisting of two plates (chorionic plate and basal plate) to facilitate the exchange of nutrients and waste products.
- The placenta goes through stages from initial formation to maturation.
Trophoblast Action
- The trophoblast cells secrete proteolytic enzymes to digest the uterine lining and allows the blastocyst to penetrate and attach to the uterine wall.
- The secreted enzymes help the embryo penetrate and adhere to the uterine lining, providing nutrients.
Receptivity of Uterus
- Receptivity involves several crucial changes: -Plasma membrane transformation (pinopodes) -Decidualization (change in endometrial thickness) and production of decidual cells.
Process of Implantation of the Blastocyst in the Uterus
- The blastocyst is transported toward the uterus from the fallopian tube and will implant in the uterine wall after approximately 3-6 days.
- It relies on the nutritive secretions of the uterine endometrium for support during this time.
- The trophoblast cells are crucial to implantation, enabling the blastocyst to penetrate and attach to the uterine lining.
Remodelling of Circulation
- The placenta's functionality depends on remodelling maternal blood vessels that allows low pressure and low velocity flow, which occurs by roughly 10-12 weeks.
- Extravillous trophoblasts (EVTs) remodel maternal spiral arteries.
Placental Maturation
- The placenta matures through the development of septa dividing into cotyledons.
- Receiving blood from approximately 80-100 spiral arteries in these structures.
Full-Term Placenta
- By the end of pregnancy, the placenta reaches a size and thickness, and a certain weight.
- The maternal side is covered by a layer of decidua basalis.
- The fetal side is covered by chorionic plate.
Umbilical Cord
- The umbilical cord connects the fetus to the placenta and consists of 3 blood vessels carrying fetal blood.
- Two arteries carry deoxygenated blood from the fetus to the placenta; a vein carries oxygenated blood from the placenta to the fetus.
Amniotic Fluid
- Amniotic fluid cushions and protects the fetus, and acts as a transport medium for fetal urine and other substances/metabolites.
- It's formed from maternal plasma diffusing through the placenta and fetal urine production.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the stages of human embryonic and fetal development, from the fertilized egg to later stages at 4, 10, 16, and 20 weeks. Key concepts include cleavage, cell differentiation, and morphogenetic events that shape the early embryo. Test your understanding of these crucial developmental milestones.