Podcast
Questions and Answers
Which primary function does the digestive system perform in the human body?
Which primary function does the digestive system perform in the human body?
- Pumping blood throughout the body to deliver oxygen.
- Filtering waste products from the blood to produce urine.
- Regulation of body temperature through sweat glands.
- Conversion of food into absorbable nutrients for energy and growth. (correct)
What is the primary process that occurs in the mouth during digestion?
What is the primary process that occurs in the mouth during digestion?
- Absorption of nutrients into the bloodstream.
- Storage of food for later digestion.
- Filtering of toxins from ingested substances.
- Mechanical and chemical breakdown of food. (correct)
How does the esophagus contribute to the process of digestion?
How does the esophagus contribute to the process of digestion?
- It absorbs the majority of nutrients from digested food.
- It neutralizes stomach acid before it reaches the small intestine.
- It propels food to the stomach through peristaltic movements. (correct)
- It filters digestive enzymes before they enter the stomach.
What is the main role of the stomach in the digestive system?
What is the main role of the stomach in the digestive system?
Which process primarily takes place in the small intestine?
Which process primarily takes place in the small intestine?
What function does the large intestine primarily perform?
What function does the large intestine primarily perform?
How do the liver and gallbladder assist the digestive system?
How do the liver and gallbladder assist the digestive system?
What role does the pancreas play in digestion?
What role does the pancreas play in digestion?
What is the role of saliva in the initial stages of digestion?
What is the role of saliva in the initial stages of digestion?
What is the role of peristalsis in the digestive process?
What is the role of peristalsis in the digestive process?
Which enzyme is secreted in the stomach to begin the digestion of proteins?
Which enzyme is secreted in the stomach to begin the digestion of proteins?
What is the function of bile salts in the digestive process?
What is the function of bile salts in the digestive process?
How does the villi structure in the small intestine contribute to nutrient absorption?
How does the villi structure in the small intestine contribute to nutrient absorption?
What is the primary role of gut microbiota in the large intestine?
What is the primary role of gut microbiota in the large intestine?
What happens to undigested materials as they reach the rectum?
What happens to undigested materials as they reach the rectum?
Which compound is essential for emulsifying fats, aiding in their digestion and absorption?
Which compound is essential for emulsifying fats, aiding in their digestion and absorption?
What role does hydrochloric acid (HCl) play in the stomach during digestion?
What role does hydrochloric acid (HCl) play in the stomach during digestion?
Which nutrient primarily begins its chemical digestion in the mouth?
Which nutrient primarily begins its chemical digestion in the mouth?
What is the purpose of the mucus layer in the stomach?
What is the purpose of the mucus layer in the stomach?
How do microvilli enhance nutrient absorption in the small intestine?
How do microvilli enhance nutrient absorption in the small intestine?
What is the role of pancreatic lipase in the small intestine?
What is the role of pancreatic lipase in the small intestine?
Which primary process is associated with the secretion of bicarbonate ions by the pancreas?
Which primary process is associated with the secretion of bicarbonate ions by the pancreas?
What effect does the hormone gastrin have on digestion?
What effect does the hormone gastrin have on digestion?
Which motility pattern is primarily responsible for mixing chyme with digestive juices in the small intestine?
Which motility pattern is primarily responsible for mixing chyme with digestive juices in the small intestine?
In the small intestine, what is the role of the enzyme lactase?
In the small intestine, what is the role of the enzyme lactase?
What is the significance of the ileocecal valve in the digestive system?
What is the significance of the ileocecal valve in the digestive system?
How does the liver metabolize carbohydrates during digestion?
How does the liver metabolize carbohydrates during digestion?
What function do goblet cells perform in the digestive tract?
What function do goblet cells perform in the digestive tract?
How does the myenteric plexus contribute to digestive processes?
How does the myenteric plexus contribute to digestive processes?
What is the primary function of the brush border enzymes in the small intestine?
What is the primary function of the brush border enzymes in the small intestine?
What is the role of the hormone cholecystokinin (CCK) in digestion?
What is the role of the hormone cholecystokinin (CCK) in digestion?
Which process is primarily responsible for moving food through the pharynx?
Which process is primarily responsible for moving food through the pharynx?
How does the enteric nervous system influence the digestive system?
How does the enteric nervous system influence the digestive system?
Which metabolic process is facilitated by bacteria in the colon?
Which metabolic process is facilitated by bacteria in the colon?
What primarily triggers the release of secretin into the bloodstream?
What primarily triggers the release of secretin into the bloodstream?
What is the role of haustral contractions in the colon?
What is the role of haustral contractions in the colon?
How does the digestion of lipids differ from the digestion of carbohydrates and proteins?
How does the digestion of lipids differ from the digestion of carbohydrates and proteins?
How does the enteric nervous system coordinate digestive activities across different organs?
How does the enteric nervous system coordinate digestive activities across different organs?
Which physiological response is directly stimulated by the presence of chyme in the duodenum?
Which physiological response is directly stimulated by the presence of chyme in the duodenum?
What is the most likely outcome if the ileocecal valve fails to function properly?
What is the most likely outcome if the ileocecal valve fails to function properly?
How does increased parasympathetic activity influence the digestive system?
How does increased parasympathetic activity influence the digestive system?
Which of the following best describes the impact of severe liver damage on lipid digestion?
Which of the following best describes the impact of severe liver damage on lipid digestion?
How does the regulation of gastric emptying optimize digestive processes?
How does the regulation of gastric emptying optimize digestive processes?
What mechanism prevents the gastric juices in the stomach from digesting the stomach itself?
What mechanism prevents the gastric juices in the stomach from digesting the stomach itself?
What is the physiological result of the migrating motor complex (MMC) during fasting?
What is the physiological result of the migrating motor complex (MMC) during fasting?
How does the composition of gut microbiota influence overall health?
How does the composition of gut microbiota influence overall health?
If someone's large intestine is removed, what is the most significant nutritional consequence?
If someone's large intestine is removed, what is the most significant nutritional consequence?
What effect would a drug that inhibits the production of gastrin have on digestion?
What effect would a drug that inhibits the production of gastrin have on digestion?
How do changes in blood flow to the digestive organs support digestion?
How do changes in blood flow to the digestive organs support digestion?
If a patient has a genetic defect that prevents the production of intrinsic factor, what specific physiological problem would they likely develop?
If a patient has a genetic defect that prevents the production of intrinsic factor, what specific physiological problem would they likely develop?
What adaptive mechanism in the small intestine increases the efficiency of nutrient absorption?
What adaptive mechanism in the small intestine increases the efficiency of nutrient absorption?
How would the surgical removal of the gallbladder affect a person's digestive capabilities?
How would the surgical removal of the gallbladder affect a person's digestive capabilities?
What is the primary role of the myenteric plexus in the digestive system?
What is the primary role of the myenteric plexus in the digestive system?
Which outcome would you expect from a drug that selectively stimulates parietal cells in the stomach?
Which outcome would you expect from a drug that selectively stimulates parietal cells in the stomach?
In the context of digestion, what is the migrating motor complex (MMC)?
In the context of digestion, what is the migrating motor complex (MMC)?
What is the physiological significance of segmentation contractions in the small intestine?
What is the physiological significance of segmentation contractions in the small intestine?
How does damage to the exocrine pancreas specifically affect digestion?
How does damage to the exocrine pancreas specifically affect digestion?
If a person chronically consumes antacids, what effect might this have on protein digestion?
If a person chronically consumes antacids, what effect might this have on protein digestion?
How does the presence of dietary fat in the duodenum affect gastric emptying?
How does the presence of dietary fat in the duodenum affect gastric emptying?
What role do the brush border enzymes play in nutrient absorption?
What role do the brush border enzymes play in nutrient absorption?
Which of the following best explains the importance of bile salts in the small intestine?
Which of the following best explains the importance of bile salts in the small intestine?
How would significantly reducing dietary fiber impact digestion in the large intestine?
How would significantly reducing dietary fiber impact digestion in the large intestine?
Flashcards
Digestive System
Digestive System
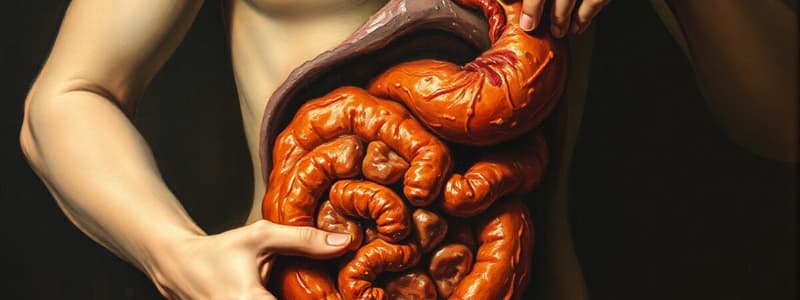
The digestive system is a system of organs responsible for getting food into and out of the body and for making use of food to keep the body healthy.
Study Notes
- Digestive System
Digestive System Anatomy
- Consists of the gastrointestinal (GI) tract
- The GI tract is a muscular tube, also called the digestive tract or alimentary canal
- Food passes along the GI tract from mouth to anus
- Consists of accessory organs
- Accessory organs produce or store secretions that flow into GI tract through ducts
Functions of the Digestive System
- Ingestion occurs when solid food and liquid enter the oral cavity
- Mechanical digestion and propulsion involves crushing and shredding food in the oral cavity, and mixing and churning in the stomach
- Chemical digestion consists of chemical and enzymatic breakdown of food into small organic molecules that can be absorbed by the digestive organs
- Secretion is the release of water, acids, enzymes, buffers, and salts by the digestive tract epithelium and by accessory digestive organs
- Absorption is the movement of nutrients across the digestive epithelium and into the bloodstream
- Defecation occurs when indigestible food is compacted into material waste called feces, which are eliminated by defecation
Mechanical Digestion
- Includes all movements that help digestion
- Mastication (chewing) is a form of mechanical digestion
- Swallowing is a form of mechanical digestion
- Mixing is a form of mechanical digestion
- Peristalsis is a form of mechanical digestion
- Muscular contractions in the wall of the GI tract physically break down food by churning it and propelling it along the tract, and also help dissolve foods by mixing them with fluids into the GI tract
Chemical Digestion
- Enzymes secreted by accessory organs and cells that line the tract break down the food chemically
- Main digestion is accomplished by using water to break down chemical bonds (hydrolysis)
- Fats are broken down into fatty acids and glycerol
- Carbohydrates are broken down into monosaccharides
- Proteins are broken down into amino acids
Major Organs & Functions
- The oral cavity (mouth) is used for mechanical processing (with the teeth and tongue), moistening, and mixing with salivary secretions
- The pharynx plays a role in muscular propulsion of food into the esophagus
- The esophagus transports materials to the stomach
- The stomach is used for chemical breakdown and mechanical processing
- The small intestine is used for enzymatic digestion and absorption
- The large intestine is used for dehydration and compaction of indigestible materials
Accessory Digestive Organs
- Salivary glands produce saliva containing mucins and enzymes
- The gallbladder stores and concentrates bile secreted by the liver
- The pancreas features exocrine cells, which secrete buffers and digestive enzymes
- Endocrine cells secrete several hormones as part of the pancreas function
- The liver has almost 200 known functions
Layers of the GI Tract
- Four major layers make up the digestive tract
- The same basic layers are in the digestive tract from esophagus to anal canal
The Layers of the GI Tract
- Mucosa (epithelium, lamina propria, muscularis mucosae) is a layer of the GI Tract
- The submucosa is a layer of the GI Tract
- The muscular layer is a layer of the GI Tract
- The serosa or adventitia is a layer of the GI Tract
Mucosa
- Inner lining/Superficial - 3 components
- Epithelium in the mouth, pharynx, esophagus, and anal canal is nonkeratinized, stratified squamous epithelium
- Epithelium in the mouth, pharynx, esophagus, and anal canal is present for protection
- Epithelium in the stomach and intestines is simple columnar epithelium
- Epithelium in the stomach and intestines is present for secretion and absorption
- Lamina propria is areolar connective tissue with blood and lymphatic vessels and mucosa - associated lymphatic tissue (MALT)
- MALT contains immune cells that protect against disease
- The muscularis mucosae is a thin layer of smooth muscles
- Muscularis mucosae making folds increase surface area specifically in the stomach and the small intestine
Submucosa
- Layer of dense irregular connective tissue
- Contains blood vessels and lymphatic vessels
- Also contains exocrine glands in some regions
- Exocrine glands secrete buffers and enzymes into the digestive tract
- Submucosa has a network of neurons called submucosal (Meissner's) plexus
Muscular Layer
- Smooth muscle in two layers
- Inner circular layer
- Outer longitudinal layer
- Muscular layer is involved in mechanical processing and movement along tract - Peristalsis
- Another network of neurons exists here called the myenteric (Auerbach's) plexus; between muscle layers
Serosa
- Outermost covering of organs along the digestive tract in the abdominal cavity
- Also called the visceral peritoneum along the digestive tract in the abdominal cavity
- No serosa in oral cavity, pharynx, esophagus and rectum
- Oral cavity, pharynx, esophagus and rectum are covered instead by adventitia (sheath formed from a dense network of collagen fibers)
- Adventitia firmly attaches tract to adjacent structures
Peritoneum
- Largest serous membrane of the body
- Divided into: Parietal Peritoneum and Visceral Peritoneum
- Parietal Peritoneum lines the inner surface of the peritoneal cavity
- Visceral peritoneum (aka. Serosa) covers organs enclosed by the peritoneal cavity
- Space between the Parietal Peritoneum and Visceral Peritoneum is peritoneal cavity that contains lubricating serous fluid
Serous Membrane
- Continuously secretes peritoneal fluid into peritoneal cavity
- Secretes and reabsorbs ~7 liters/day total
- Volume at any one time is about 50 mL
- Thin layer separates parietal and visceral surfaces
- Allows sliding movements without friction or irritation
- Rate of fluid moving into the cavity is accelerated by liver disease, kidney disease, and heart failure
- Accumulation of peritoneal fluid can create abdominal swelling (ascites)
Retroperitoneal Organs
- Some organs are considered retroperitoneal which means the peritoneum only covers their anterior surface
- Kidneys are retroperitoneal Organs
- Ascending and descending colon are retroperitoneal Organs
- Duodenum is a retroperitoneal Organ
- Pancreas is a retroperitoneal Organ
- Ureters are retroperitoneal Organs
- 3 major Peritoneal folds in the peritoneum: Mesentery, Omenta, Falciform ligaments
Peritoneal Folds
- Mesentery is a double sheets of peritoneal membrane
- Areolar tissue lies between mesothelial layers and provides access route for blood vessels, nerves, and lymphatics
- Stabilizes attached organs and attaches to the posterior abdominal wall
- Prevents entanglement of intestines
- Includes the Mesocolon - Mesentery of the colon
- There are two omenta in the body, they are continuations of the mesentery: Greater omentum and Lesser omentum
Greater Omentum
- Attach to stomach and transverse colon
- Forms a large pouch extending inferiorly b/w anterior body wall and anterior surface of the small intestine
- Contains adipose tissue that provides padding and protection
- Also contains blood vessels and lymphatic tissue
Lesser Omentum
- Suspends the stomach and duodenum from the liver
- Provides an access route for blood vessels and other structures entering/leaving the liver
- The hepatic portal vein is part of the other structures involved
- The hepatic artery is part of the other structures involved
- The common bile duct is part of the other structures involved
Falciform Ligament
- Connects the liver to the anterior body wall
- The liver is the only digestive organ that is attached to the ANTERIOR abdominal wall
- Remnant part of the umbilical vein
Nerve Plexuses
- The nerve plexuses are involved in local control of digestive activities
- Parasympathetic stimulation increases digestive muscle tone and activity
- Sympathetic stimulation decreases muscle tone and activity
- Two major nerve plexuses: Submucosal neural plexus (Meissner's) and Myenteric plexus (Auerbach's)
Submucosal Neural Plexus (Meissner's)
- Located in the submucosal layer
- Innervates the mucosa and submucosa
- Contains sensory neurons and autonomic nerve fibers
Myenteric Plexus (Auerbach's)
- Network of sensory neurons and autonomic nerve fibers
- Located in the muscularis externa b/w the circular and longitudinal layer
- Works with the submucosal plexus to coordinate local control of digestive activity
Enteric Nervous System (ENS)
- The submucosal and myenteric plexuses make up the ENS
- It is an intrinsic set of nerves, otherwise known as the "brain of the gut"
- Neurons extend from the esophagus to the anus
- Quasi autonomous – meaning it can act on its own with some input from the autonomic nervous system
Autonomic Nervous System
- Extrinsic set of nerves
- The vagus nerve (CN X) supplies parasympathetic fibers to most of the GI tract
- Except the last ½ of the large intestine which is supplied from the sacral spinal cord
- Parasympathetic stimulation will increase secretion and motility by increasing activity of ENS neurons
- Sympathetic nerve supply arises from thoracic and lumbar region of the spinal cord
- Stimulation decreases secretions and activity by inhibiting ENS
The Oral Cavity
- Space that contains the tongue, teeth, and gums
- Lined by oral mucosa (stratified squamous epithelium)
- Thin mucosa inferior to the tongue allows for rapid absorption of lipid-soluble drugs (nitroglycerin)
- Little to no nutrients are absorbed here
- Digestion of carbohydrates and lipids begins here
Oral Cavity Boundaries
- Superior Boundary is the hard palate and the soft palate
- The hard palate is formed by the palatine processes of the maxillary bones and horizontal plates of the palatine bones
- Thick mucosa w/ ridges covering the hard palate provides traction for compression of food by the tongue
- The soft palate is a muscular region posterior to the hard palate
- The Anterior/Lateral Boundary is the cheeks and the labia
- Cheeks form the lateral walls of the oral cavity
- Cheeks are supported by pads of fat and the buccinator muscles
- Anteriorly, cheek mucosa is continuous with the labia
- Labia are aka lips
- Labia form the anterior boundary
- The inferior boundary is the tongue
- The body of the tongue is the anterior, mobile portion
- The posterior boundary is the uvula
- The uvula is a dangling process extending from the soft palate
- The uvula helps prevent food from entering pharynx prematurely
- During swallowing, the Uvula swings upward to prevent food from entering the nasopharynx
- Palatine tonsils are located on either side of the oropharynx
- The root of the tongue is the fixed portion projecting into the oropharynx and is marked by a V-shaped line of vallate papillae
- Lingual tonsils are located in the root of the tongue
Other Features of the Oral Cavity
- The oral vestibule is the space b/w the cheeks (or lips) and teeth
- The frenulum of the upper lip attaches gums to the upper lip
- The frenulum of the lower lip attaches gums to lower lip
- Gingivae (gums) are ridges or oral mucosa surround the base of each tooth
- Gingivae (gums) are firmly attached to the periostea of the underlying bone
Tongue
- Accessory digestive organ
- Skeletal muscle covered by mucous membrane
- Extrinsic muscles move the tongue side to side and in and out to maneuver food for chewing and forcing food to the back of the mouth for swallowing
- Intrinsic muscles originate in and insert into connective tissue within the tongue
- Dorsum and lateral surfaces are covered w/ papillae which contain taste buds and some receptors for touch
- Tongue surface is flushed by secretions of small glands
- Secretions contain water, mucins, and lingual lipase (an enzyme that starts the digestion of lipids)
- The tongue is attached to the floor of the mouth by the frenulum of the tongue (lingual frenulum)
Salivary Glands
- Salivary glands release saliva into the oral cavity
- Just enough saliva is secreted to keep mouth and pharynx moist and clean
- When food enters mouth, secretion increases to lubricate, dissolve and begins the chemical digestion of food
- Three pairs of major salivary glands secrete most of the saliva: Parotid glands, Submandibular glands, and Sublingual glands
Parotid Glands
- Lie inferior to the zygomatic arch, deep to the skin, covering the mandible
- Secretes saliva via parotid duct
- Produce serous secretion containing large amounts of salivary amylase
- Parotid Glands produce ~25% of total saliva
Sublingual Glands
- Located beneath the tongue
- Sublingual ducts open into the floor of the mouth
- Produce a mucous secretion that acts as a buffer and lubricant
- Sublingual Glands produce ~5% of total saliva
Submandibular Glands
- Located medial and inferior to the body of the mandible and the submandibular ducts enter the oral cavity lateral to the lingual frenulum
- Secrete a mixture of buffers, mucins, and salivary amylase
- Amylase is an enzyme that breaks down starches
- Cells transport IgA antibodies into the saliva, providing protection against pathogens
- Submandibular glands produce ~70% of total saliva
Saliva
- Mostly water – 99.5%
- 0.5% solutes make up saliva
- Ions (sodium, potassium, chloride, bicarbonate and phosphate), dissolved gases, urea, uric acid, mucous, immunoglobulin A, lysozyme, and salivary amylase are key materials in saliva
- Saliva constantly flushes oral surfaces
- Saliva buffers keep pH of mouth near 7.0 and prevent buildup of acids produced by bacteria
- Saliva contains antibodies (IgA) and lysozyme to help control oral bacteria populations
- Saliva mixes with food to form a bolus to be easily swallowed
- Lingual glands are small glands called Ebner's glands secrete lingual lipase
Salivation
- Controlled by autonomic nervous system
- Parasympathetic stimulation promotes secretion of moderate amount of saliva
- Sympathetic stimulation decreases salivation
- The taste and smell of food are potent stimulators of salivary gland secretions ( "cephalic phase" of digestion)
Teeth
- Accessory digestive organ
- Dentin forms the majority of the tooth and is harder than bone
- Teeth are covered by enamel, which is even harder
- There are 2 dentitions: Deciduous or primary teeth and Permanent or secondary teeth
Components of a Tooth
- The bulk to each tooth is composed of dentin
- The mineralized matrix is similar to bone but contains no cells
- The pulp cavity is the interior chamber of the tooth
- Enamel covers the dentin of the crown
- Enamel is the hardest biologically manufactured substance
- Enamel is composed of calcium phosphate
- Enamel requires calcium, phosphate, and vit D for formation and resistance to decay
- The root canal is the narrow tunnel within the root of the tooth
- Root canal is a passageway for blood vessels and nerves to the pulp cavity
- The opening into the root canal is the apical foramen
Regions of a Tooth
- The crown is the portion projecting into the oral cavity from the surface of the gums
- The neck is the boundary between the crown and root
- The root is the portion below the gum line
- The root sits in a bony tooth socket called an alveolus
Digestion in the Mouth
- The mouth is the 1st place where digestion begins, both mechanical and chemical
- Mechanical Digestion involves chewing or mastication
- Food is manipulated by tongue, ground by teeth, and mixed w/ saliva
- Forms a soft, flexible mass called a bolus
- Chemical Digestion involves Salivary Amylase and Lingual Lipase
- Salivary Amylase is secreted by salivary glands and acts on starches
- Only monosaccharides can be absorbed into the bloodstream
- Salivary Amylase continues to act until inactivated by stomach acid, works well in the mouth but not in the stomach
- Lingual Lipase is secreted by lingual glands of tongue acts on triglycerides/fats
- Lingual Lipase is active in the mouth, but becomes even more activated in acidic environment of stomach
- Lingual lipase acts to breakdown dietary triglycerides into fatty acids and diglycerides
- Lingual Lipase works well in the stomach but not the mouth because the stomach is an acidic environment
Pharynx
- Membrane-lined cavity posterior to the nose and mouth, otherwise known as the throat
- Skeletal muscle wall of the pharynx plays a key role in swallowing along with the esophagus
- The pharynx is continuous w/ the esophagus
- Common passageway for solid food, liquids, and air
- Three regions: Nasopharynx (respiration only), Oropharynx, and Laryngopharynx
The Esophagus
- The esophagus actively moves food and liquids to the stomach
- No enzymes produced here, and no absorption takes place here
- The esophagus is a hollow, muscular tube
- The esophagus' narrowest point is at the beginning (posterior to cricoid cartilage)
- Esophagus descends posterior to the trachea
- Enters the abdominopelvic cavity through the esophageal hiatus (opening in the diaphragm)
Histology of the Esophagus
- Mucosa is made of Nonkeratinized stratified squamous epithelium – for protection
- Mucosa and submucosa form large folds extending the length of the esophagus, which allows for expansion with passage of bolus
- Submucosa contains areolar CT, blood vessels, and mucous glands
- The muscularis externa features different muscle setups
- The superior third is composed of skeletal muscle
- The middle third is composed of a mix of skeletal and smooth muscle
- The inferior third is composed of smooth muscle only
- Instead of a serosa, the esophagus features the adventitia of connective tissue that anchors it to the posterior body wall
Control of Movement in the Epophagus
- The upper esophageal sphincter is a band of smooth muscle that functions as a sphincter
- Upper Esophageal Sphincter prevents air from entering the esophagus
- The lower esophageal sphincter is aka cardiac sphincter
- The lower esophageal sphincter is at the inferior end of the esophagus
- The lower esophageal sphincter is normally contracted so it prevents backflow of stomach contents
Swallow of Deglutition
- Initiated voluntarily but proceeds automatically
- Facilitated by secretions of saliva and mucus
- Involves mouth, pharynx, and esophagus
- There are three phases of swallowing: Buccal Phase, Pharyngeal Phase, and Esophageal Phase
Buccal Phase
- Voluntary phase
- Begins with compression of bolus against hard palate
- Tongue forces bolus into the oropharynx and also elevates soft palate (sealing off nasopharynx)
- Entry into the oropharynx triggers reflex response
Pharyngeal Phase
- Begins with stimulation of tactile receptors in uvula and palatine arches
- Motor commands from the swallowing center (in medulla oblongata) coordinate muscle contraction in pharyngeal muscles
- Larynx is elevated; epiglottis is folded; and the uvula and soft palate are elevated
- Bolus is moved through the pharynx into the esophagus
Esophageal Phase
- Begins as bolus is forced through the entrance to the esophagus
- Bolus is pushed toward the stomach by peristalsis
- Approach of bolus triggers the opening of the lower esophageal sphincter
- Bolus enters the stomach
- Typical travel time is 9 seconds, but liquids may travel faster
- A dry (poorly lubricated) bolus may require secondary peristaltic waves
Peristalsis
- Smooth muscle contractions produce motility of the digestive tract
- Wave of muscle contraction
- Food enters the digestive tract as a bolus, which is a moist, compact mass of material
- Bolus is propelled along the tract by contractions of the muscularis externa (peristalsis)
GI Pathology
- Periodontal disease is the most common cause for loss of teeth
- Occurs when dental plaque forms between gums and teeth
- Resulting bacterial activity may cause gingivitis (inflammation of the gums), tooth decay and eventual breakdown of periodontal ligaments and surrounding bone
- Linked to cardiovascular disease due to inflammation and atherosclerosis
The Stomach
- Connects the esophagus to the duodenum in the upper left quadrant
- Serves as a mixing chamber and holding reservoir due to mechanical digestion
- In the stomach, digestion of starch continues (briefly), digestion of proteins begins, and digestion of triglycerides increases and certain substances are absorbed due to chemical digestion
- Produces intrinsic factor
- A muscular, expandable, J-shaped organ with three layers in the muscular layer
- Highly variable shape depending on its contents
- When empty: a muscular tube with constricted lumen
- When full: the stomach can expand to contain 1 – 1.5 L of material - chyme
- Chyme is a viscous, highly acidic, soupy mixture formed from the combination of food, saliva, and gastric gland secretions
- The lesser curvature forms the medial surface and is attached to the mesentery of the lesser omentum
- The greater curvature forms the lateral and inferior surfaces and is attached to the mesentery of the greater omentum
Stomach Regions
- The four regions of the stomach are the fundus, cardia, body, and pylorus
- The fundus is superior to the junction between the stomach and esophagus
- The cardia is the superior, medial portion within 3 cm of gastroesophageal junction and secretes mucus to protect esophagus from stomach acid/enzymes
- The body is the largest region (majority of the stomach) and is located b/w the fundus and pylorus to function as a mixing bowl
- The pylorus is the sharp curve of "J" of the stomach, frequently changes shape w/ mixing movements and is made up of the pyloric antrum and pyloric canal
- Pyloric antrum – portion connected to stomach body (antron, cavity)
- Pyloric canal – empties into the duodenum (prox segment of small intestine)
- Chyme leaving the stomach is controlled by the pyloric sphincter
- Chyme is what the bolus converts to the stomach
Rugae
- Prominent, temporary mucosal folds
- Allow gastric expansion by flattening out with stomach expansion
- Otherwise known as wrinkles
- Muscularis mucosae is responsible for the wrinkles
Histology of the Stomach
- Features Mucosa, Submucosa, Muscular Layer, and Serosa
- Mucosa is composed of simple columnar epithelium
- Mucosa produces layer of alkaline mucus, which protects epithelial cells against acid and enzymes in gastric lumen
- Epithelial cells extend down into lamina propria to form columns of secretory cells called gastric glands which open up into gastric pits
- Secretions flow from gastric glands to gastric pits to the lumen
Gastric Pits
- Shallow depressions opening onto the gastric surface
- Active stem cells at the base of each pit replace superficial cells shed into the chyme
- Each pit communicates with several gastric glands
Gastric Glands
- Glands in the fundus and body secrete most of the acid and enzymes enabling gastric digestion and are dominated by parietal cells and chief cells
- Glands in the pylorus secrete mucus and hormones that coordinate and control digestive activity
- Submucosa is composed of areolar connective tissue
- The muscular layer contains 3 layers of smooth muscle (muscularis externa): Outer longitudinal layer, Middle circular layer, and Inner oblique layer
- The purpose of the third layer is for extra churning in the stomach for extra control
- The third layer of smooth muscle is only in the body
- Serosa is a part of visceral peritoneum
- From the lesser curvature, serosa forms the lesser omentum
- From the greater curvature, serosa forms the greater omentum
Cells of Gastric Glands
- Four main cell types: parietal cells, chief cells, mucous neck cells, and G cells
- Parietal cells' exocrine function into the lumen is to produce: intrinsic factor (glycoprotein that aids in vitamin B12 absorption) and hydrochloric acid – HCI which activates pepsinogen to keep the stomach at pH 1.5 - 2
- Intrinsic factor ferries B12 through the stomach
- Hydrochloric acid keeps stomach at pH 1.5 - 2
- Chief cells are exocrine function cells into lumen and produce: Pepsinogen (activated by HCI to become pepsin – active proteolytic protein-digesting enzyme) and Gastric lipase (fat digesting enzyme)
- Mucous neck cells are exocrine cells that function into the lumen, producing Mucus which protects the epithelial layer of the stomach from high acid contents
- G cells are endocrine cells that function into the blood, producing gastrin which regulates digestion
Digestion in the Stomach
- Digestion that started in the mouth continues in the stomach, both mechanical and chemical
Mechanical Digestion in the Stomach
- Mixing waves are gentle, rippling peristaltic movements and creat chyme by breaking down food, mixing it with secretions of the gastric glands
- Once the food reaches the pyloric sphincter, each mixing wave forces about 3mL of chyme into the duodenum
- Gastric emptying is when each mixing wave forces about 3mL of chyme into the duodenum and it happens slowly b/c the food needs to touch the walls of the intestines in order to absorb, and the fattier the food the longer it stays in your stomach
Chemical Digestion in the Stomach
- Salivary amylase continues acting in the stomach until the churning mixes it with the acidic gastric juices
- Lingual lipase becomes more active in the stomach, acting to digest triglycerides into fatty acids and diglycerides
- Hydrochloric acid is Secreted by parietal cells, it kills many microbes, denatures proteins (unravels proteins) and stimulates the release of hormones that promote flow of bile and pancreatic juice
- Pepsin is Secreted by chief cells and is secreted as pepsinogen (inactive form)
- Pepsinogen is an inactive form because the body would just naturally eat all the proteins in your body
- Pepsinogen is activated once it comes in contact with HCI
- Gastric lipase is secreted by chief cells and splits triglycerides into fatty acids and monoglycerides
Absorption in the Stomach
- There is only a small amount of nutrient absorption that takes place in the stomach
- The small amount of absorption that happens in the stomach includes some Water, Ions, Short chain fatty acids, Caffeine, Certain drugs (aspirin), and Alcohol
- Regarding alcohol, the stomach has enzymes: alcohol dehydrogenase, so blood alcohol doesn’t go up in the stomach and if you eat with alcohol, its going to undergo metabolism and not affect you as much
- Alcohol can also get ingested to the small intestine, then go to the blood, and then blood alcohol level increases
The Small Intestine
- Plays a key role in nutrient digestion and absorption
- 90% of nutrient absorption occurs in small intestine
- Most of the remaining 10% occurs in the large intestine
- The average overall length is 6m (20 ft)
- The three segments are: Duodenum, Jejunum, Ileum
Segments of the Small Intestines
- Three segments include
- The Duodenum is the smallest in length and is the segment closest to the stomach that acts as a "mixing bowl"
- The Duodenum receives chyme from the stomach and digestive secretions from liver, gallbladder, and pancreas, is mostly retroperitoneal and features duodenal glands that produce mucous secretions, producing extremely alkaline mucous
- The Duodenum has few circular folds and small villi with the main function to neutralize acidic chyme
- The Jejunum is between the duodenum and ileum and second longest portion located in the peritoneal cavity, has numerous circular folds and abundant, long villi
- The Jejunum is responsible majority of chemical digestion and nutrient absorption
- The Ileum is the final segment of the small intestine and the longest portion that ends at the ileocecal valve
- The Ileum regulates theSphincter controlling flow from the ileum into the cecum of the large intestine and has few circular folds with none in the distal portion, villi are relatively stumpy
- The Ileum's submucosa contains aggregated lymphoid nodules
Histology of the Small Intestine
- Includes Mucosa, submucosa, muscularis, and serosa
- Mucosa features simple columnar epithelium and contains many different cells, including Absorptive cells (digest and absorb, most abundant), Goblet cells which produce mucus, Intestinal glands that create intestinal juice, Paneth cells that create lysozymes and Enteroendocrine cells
- Enteroendocrine cells include S cells which secrete secretin, CCK cells which secrete CCK and K cells which secrete glucose-dependent insulinotropic peptide (GIP)
- The abundance of MALT is present in the small intestine in Groups of lymphatic nodules called Peyer's patches that are present in the ileum
- Peyer's patches are big nodules of MALT (immune)
- The Submucosa contains Duodenal (Brunner's) glands that secrete alkaline mucus that helps neutralize gastric acid in chyme
- The Muscularis has outer longitudinal layer and inner circular layer
- The Serosa completely surrounds the small intestine except for majority of duodenum because it is retroperitoneal
Special Structures of the Small Intestine
-
Special structures include Circular Folds (Plicae Circulares), Villi, and Microvilli
-
Circular folds (Plicae Circulares) are a Series of transverse folds along the intestinal lining and are a permanent feature
-
Circular folds (Plicae Circulares) are different than rugae
-
There are roughly 800 folds in the small intestine, mostly in the jejunum
-
Increase surface area for absorption
-
Villi is the Small mucosal projections that increase surface area for absorption that and are finger-like projections giving a velvety appearance, are also Covered by epithelial cells and surfaces covered with microvilli
-
Each villi contains an arteriole, venule, blood capillary, and lacteal
Internal structure of a villus
- Extensive Capillary network in the lamina propria that carries absorbed nutrients to the hepatic portal circulation
- The Lymphatic Capillary, or Lacteal transports material that cannot enter blood capillaries, Absorbed fatty acids are assembled into protein-lipid packages (chylomicrons) too large to diffuse into bloodstream
- Transported by lymphatic system to venous circulation
- Smooth muscle in muscularis mucosae and within the villi moves villi back and forth, exposing surfaces to intestinal contents and Squeezes lacteal, assisting in lymph movement
Microvilli
- Projections of apical membrane of absorptive cells that creates a brush border with brush border enzymes
- Brush Border: Carpet of microvilli on the surface of the epithelial cells that increases surface area for absorption, Contains enzymes that digest material, and creates epithelial cells that can then absorb breakdown products
The Pancreas
- The pancreas has endocrine and exocrine functions
- The exocrine functions contribute to digestion
- Location - retroperitoneal organ that lies posterior to the greater curvature of stomach
- Also located behind the stomach
Ducts of the Pancreas
- Includes both the pancreatic duct and the accessory pancreatic duct
- The Pancreatic Duct delivers exocrine secretions to the duodenum and is aka the duct of Wirsung
- The Pancreatic Duct joins the common bile duct from the liver and gallbladder and enters duodenum as a common duct via the hepatopancreatic ampulla otherwise know as the Ampulla of Vater
- The ampulla opens at the major duodenal papilla
- The Accessory Pancreatic Duct is aka Santorini duct, branches from the pancreatic duct and empties separately into the duodenum
- Accessory Pancreatic Duct's are found in 3 – 10 % of the population
Pancreatic Tissue
- Made up of small clusters of glandular epithelial cells
- 99% are Pancreatic Acini, containing pancreatic acinar cells which secrete pancreatic enzymes and buffers, and are Exocrine cells
- 1% are Pancreatic Islets wich secrete hormones (glucagon, insulin, somatostatin, and pancreatic polypeptide), and are Endocrine cells
Pancreatic Juice
- About 1200 – 1500 mL of pancreatic juice are produced each day
- Combination of mostly water and ions (secreted by epithelial cells lining the duct) and exocrine secretions (enzymes and buffers)
- Sodium bicarbonate - buffers acidic stomach chyme
- Pancreatic juice is slightly alkaline helping stop action of pepsin and creates proper pH for enzymes to act in the small intestine
- 8 Enzymes are typically produced by the Pancreas
- Pancreatic amylase (digest starch)
- Proteolytic enzymes (digest protein)
- Pancreatic lipase is the main fat-digesting enzyme***
- Nucleases (Ribonuclease and Deoxyribonuclease) (digest RNA and DNA)
- Trypsinogen (digest protein)
The Pancreas - Enzymes
- Pancreatic Amylase is a Carbohydrase, breaks down certain starches and is very similar to salivary amylase
- Pancreatic Lipase breaks down certain complex lipids and is the main fat digesting enzyme
- Nucleases are Ribonuclease and Deoxyribonuclease, break down RNA or DNA
- Proteolytic Enzymes break proteins apart into mixture of dipeptides, tripeptides, and amino acids
- Proteolytic Enzymes are secreted as inactive proenzymes and are Activated in the duodenum
- The active form of Proteolytic Enzymes include
- Trypsin
- Chymotrypsin
- Carboxypeptidase
- Elastase
- Trypsin must be activated via enterokinase to activate any of the other proteolytic enzymes
Trypsin
- Trypsinogen is released from the pancreas and will reach the small intestine and will encounter enterokinase (a brush-border enzyme)
- Enterokinase activates trypsin, which then acts on the other inactive enzymes to activate them
The Liver
- Largest visceral organ and is inferior to the diaphragm
- Occupies most of the right hypochondriac and part of the epigastric region of the abdominopelvic cavity
- The gallbladder is a pear shaped sac that is located in a depression of the posterior surface of the liver and hangs from the anterior margin
- Wrapped in tough fibrous capsule
- Covered by layer of visceral peritoneum
- There are 4 lobes of the liver: Left lobe, Right lobe, Caudate lobe, and Quadrate lobe
Functions of the Liver
- Carbohydrate metabolism, important in maintaining a normal blood glucose level
- Lipid metabolism, store some TG, breakdown fatty acids, and synthesize lipoproteins and cholesterol
- Protein metabolism, Hepatocytes deaminate amino acids and will convert toxic ammonia to urea
- Processing of drugs and hormones, The liver detoxifies alcohol and excretes drugs
- Excretion of bilirubin
- Bilirubin is absorbed by the liver from the blood and secreted into bile
- Synthesis of bile salts
- Bile salts are used in the small intestine for emulsification and absorption of lipids
- Storage of glycogen and certain vitamins and minerals
- Phagocytosis
- Act to phagocytize aged WBC, RBC, and some bacteria
- Activation of vitamin D occurs with the skin, liver, and kidneys which participate in synthesizing active form of vitamin D
Associated Structures of the Liver
- The gallbladder Temporarily stores bile produced by the liver
- The bile duct caries bile from the liver and gallbladder to the duodenum
Cells of the Liver
- Hepatocytes make up 80% of the liver
- Major functional cells of liver
- Have wide variety of metabolic, secretory, and endocrine function
- Secrete bile (excretory product and digestive secretion)
- Stellate Macrophages are aka Kupffer cells and have immune function and are used for iron storage
Liver Ducts
- Bile canaliculi are Ducts between hepatocytes that collect bile and the bile Exits liver as common hepatic duct
- Hepatic sinusoids are Highly permeable blood capillaries that receive oxygenated blood from hepatic artery, and Receive deoxygenated nutrient-rich blood from hepatic portal vein
- Hepatic sinusoids will converge and deliver blood to a central vein which then drains into the inferior vena cava
Portal Triad
- Contains three structures:
- A branch of the hepatic portal vein
- Receives blood from the hepatic portal system bringing blood from abdominal viscera
- A branch of the hepatic artery
- A bile duct
- Branches from the arteries and veins of each portal area deliver blood to liver (hepatic) sinusoids of adjacent liver lobules
Functional Anatomy of a Liver Lobule
- Blood enters the liver sinusoids from branches of the hepatic portal vein and hepatic artery proper, including about 1/3 being arterial and about 2/3 coming from hepatic portal vein
- Hepatocytes adjacent to the sinusoids regulate solute and nutrient levels by absorption and secretion
- Stellate macrophages in the sinusoidal lining engulf pathogens, and cell debris and damages blood cells
- Stellate macrophages also store iron, some lipids, and heavy metals (tin, mercury) absorbed by the digestive tract
- Sinusoids all drain into a central vein, which the drains into hepatic veins, which drain into the inferior vena cava
- Hepatocytes secrete bile into a network of narrow channels called bile canaliculi
- Bile canaliculi merge to form bile ductules, and Bile ductules carry bile to bile ducts in nearest portal area
- Bile plays a role in the digestion of fats
Bile
- Hepatocytes secrete 800 – 1000 mL of bile daily
- Contains mostly water, bile salts, cholesterol, lecithin, bile pigments (bilirubin) and several ions
- Bilirubin is the principal bile pigment, and it comes from blood
- Partially excretory product/partially digestive secretion
- Bile salts play role in emulsification (the breakdown of large lipid globules into a suspension of small lipid globules)
- Bile salts aid in absorption of lipids following digestion
- This is a mechanical breaks down of fat causing the fat not to change, it just gets smaller
The Gallbladder
- Hollow, pear-shaped organ and is located in the depression on the posterior surface of the liver's right lobe
- The Mucosa layer consists of simple columnar epithelium arranged in rugae similar to that in the stomach
- Between meals stores and concentrates bile secreted from the liver
- Contraction of smooth muscle fibres ejects contents of gall bladder into cystic duct
- Production of bile never stops, it is always produced and is stored in the gallbladder
- Removing water out of the bile causes the concentrated bile to work better
- The bile from
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.