Podcast
Questions and Answers
What is the primary function of cholecystokinin in the digestive system?
What is the primary function of cholecystokinin in the digestive system?
- Promote the growth of colon mucosa
- Inhibit gastric emptying (correct)
- Stimulate insulin release
- Stimulate the secretion of gastric acid
Which statement best describes the role of gastrin?
Which statement best describes the role of gastrin?
- Inhibits gastric acid secretion
- Stimulates digestion of carbohydrates
- Stimulates secretion of gastric acid (correct)
- Facilitates absorption of proteins
What condition favors gastric emptying according to the physiological rules?
What condition favors gastric emptying according to the physiological rules?
- Relaxation of the esophagus
- Decreased tone of the stomach
- Forceful peristaltic contractions (correct)
- Increased tone of the pylorus
Which stage of colon cancer involves invasion into nearby organs?
Which stage of colon cancer involves invasion into nearby organs?
Which method of carbohydrate absorption does not require energy?
Which method of carbohydrate absorption does not require energy?
What is the primary function of the lower esophageal sphincter (LES)?
What is the primary function of the lower esophageal sphincter (LES)?
What physiological mechanism stimulates secondary peristalsis?
What physiological mechanism stimulates secondary peristalsis?
What effect does aldosterone have in the small intestine?
What effect does aldosterone have in the small intestine?
Flashcards
Peristalsis
Peristalsis
Involuntary muscle contractions that move food through the digestive tract.
Cholecystokinin (CCK)
Cholecystokinin (CCK)
Hormone released from the duodenum and jejunum in response to fatty acids, proteins, and weak acids; inhibits gastric emptying.
Gastrin
Gastrin
Hormone released from the antrum and duodenum in response to protein digestion products; stimulates growth of the stomach, duodenum, and colon mucosal lining.
Slow Waves
Slow Waves
Signup and view all the flashcards
Spike Potentials
Spike Potentials
Signup and view all the flashcards
Segmentation
Segmentation
Signup and view all the flashcards
Rapid Gastric Emptying
Rapid Gastric Emptying
Signup and view all the flashcards
Regulation of Gastric Emptying
Regulation of Gastric Emptying
Signup and view all the flashcards
Study Notes
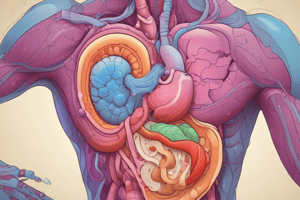
Digestion Overview
- Digestion begins in the mouth, with peristalsis moving food through the digestive tract to the anus.
- Cholecystokinin (CCK) is released from I-cells in the duodenum and jejunum, stimulated by fatty acids, proteins, and weak acids. It inhibits gastric activity.
- Gastrin, released from G cells in the antrum and duodenum, stimulates hydrochloric acid secretion and the growth of stomach, duodenum, and colon mucosa. Its release is stimulated by protein digestion products.
- Glucose-dependent insulinotropic polypeptide (GIP) stimulates insulin release.
Motility and Emptying
- Slow waves excite spike potentials, which are true action potentials.
- Rapid gastric emptying can cause diarrhea, hypertension, reactive hypoglycemia, and duodenal ulcers.
- Gastric emptying is regulated by factors like stomach tone, pylorus tone, and peristaltic contractions.
- Chyme must enter the duodenum at a proper rate after a meal.
Colon Cancer Stages
- Stage 1: Cancer spreads from the colon's inner lining to the muscle layer.
- Stage 2: IIa= cancer spreads through the muscle layer to the outer covering (serosa), IIb= cancer spreads through the serosa but not to nearby organs; IIc= tumor invasion and spread to nearby organs.
- Stage 3: IIIa= cancer spreads to muscle, and has spread to 1-3 nearby lymph nodes or 4-6 nearby lymph nodes; IIIb= cancer to muscle/serosa and 4-6 nearby lymph nodes; IIIc= cancer through serosa to nearby organs and 1+ nearby lymph nodes.
- Stage 4: Cancer spreads to other parts of the body through the bloodstream and lymphatic system.
Carbohydrate Absorption
- Membrane carrier (SGLUT-1): Absorbs glucose using energy from the Na+-K+ ATPase.
- Fructose (GLUT-5): Absorbed via facilitated diffusion (GLUT-5), does not require energy, but relies on a concentration gradient.
Intestinal Motility
- Peristalsis moves food in one direction (law of gut).
- Segmentation moves food in both directions (mixing movement).
- Secondary peristalsis is induced by distension.
Upper Gastrointestinal Sphincters
- Upper esophageal sphincter (UES): Prevents air from entering the esophagus.
- Lower esophageal sphincter (LES): Prevents acid reflux into the esophagus.
Sodium Absorption in the Small Intestine
- Absorption mechanisms: Sodium absorption in the SI and colon occurs via diffusion through water channels, co-transport with amino acids and glucose, co-transport with chloride, or counter-transport in exchange for hydrogen ions.
- Aldosterone: Increases sodium reabsorption and potassium secretion in the small intestine and colon.
Crypt Cell Secretion
- Mechanism: Cyclic AMP (cAMP) activates chloride channels, sodium follows the electrical gradient, and water moves along the osmotic gradient.
Secretin
- Function: A natural anti-acid.
Cirrhosis and Complications
- Definition: Chronic liver disease where healthy liver cells are replaced by scar tissue, often due to excessive alcohol intake.
- Complications: Jaundice, ascites, coma/death, esophageal varices, blood clotting abnormalities, and peripheral edema.
Autonomic Nervous System (ANS)
- Vagus stimulation: Information about how the vagus nerve stimulation plays a role in the ANS is not included in the provided text.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.