Podcast
Questions and Answers
What is the primary function of saliva in initiating starch digestion?
What is the primary function of saliva in initiating starch digestion?
- To neutralize acids and prevent damage to the teeth.
- To denature proteins for easier breakdown in the stomach.
- To break down dietary starch into maltose via amylase. (correct)
- To emulsify fats through the action of bile salts.
How does the enteric nervous system (ENS) within the gastrointestinal tract differ from the central nervous system?
How does the enteric nervous system (ENS) within the gastrointestinal tract differ from the central nervous system?
- It secretes hormones directly into the bloodstream to regulate digestion.
- Its neurons are located within the walls of the digestive tract. (correct)
- It primarily regulates motility and secretion via hormonal control.
- It solely controls digestive functions without autonomic modification.
What is the main purpose of motility in the stomach and intestines?
What is the main purpose of motility in the stomach and intestines?
- To mix food with digestive enzymes and transport it down the GIT. (correct)
- To solely absorb nutrients from digested food.
- To solely secrete hormones for regulating digestion.
- To solely neutralize acids entering from the stomach.
What role do the autonomic nervous system and gastrointestinal hormones play in the control of the gastrointestinal system (GIS)?
What role do the autonomic nervous system and gastrointestinal hormones play in the control of the gastrointestinal system (GIS)?
In the context of saliva production, how does parasympathetic stimulation differ from sympathetic stimulation?
In the context of saliva production, how does parasympathetic stimulation differ from sympathetic stimulation?
How does the stomach contribute to the digestion process after food enters it?
How does the stomach contribute to the digestion process after food enters it?
Mucous cells, parietal cells, chief cells, and G cells are all found in the stomach. What roles do parietal cells play?
Mucous cells, parietal cells, chief cells, and G cells are all found in the stomach. What roles do parietal cells play?
What is the role of gastrin, a hormone secreted by G cells in the stomach?
What is the role of gastrin, a hormone secreted by G cells in the stomach?
How do the cephalic, gastric, and intestinal phases regulate gastric secretion?
How do the cephalic, gastric, and intestinal phases regulate gastric secretion?
How does the small intestine maximize its surface area for nutrient absorption given its limited space?
How does the small intestine maximize its surface area for nutrient absorption given its limited space?
Once food particles reach the small intestine, what substances are they exposed to that aid in digestion?
Once food particles reach the small intestine, what substances are they exposed to that aid in digestion?
What occurs when the contents reaching the small intestine are highly acidic or hyperosmolar?
What occurs when the contents reaching the small intestine are highly acidic or hyperosmolar?
How does the exocrine pancreas contribute to the digestive process, and what key components are involved?
How does the exocrine pancreas contribute to the digestive process, and what key components are involved?
What is the primary method of protein digestion by enzymes?
What is the primary method of protein digestion by enzymes?
In the digestion of lipids, which enzyme acts on triglycerides to form monoglycerides and fatty acids?
In the digestion of lipids, which enzyme acts on triglycerides to form monoglycerides and fatty acids?
Cholecystokinin (CCK) and secretin are important for pancreatic juice. Select the roles of CCK and secretin.
Cholecystokinin (CCK) and secretin are important for pancreatic juice. Select the roles of CCK and secretin.
Which of the following is NOT a primary role of the liver in metabolism and detoxification?
Which of the following is NOT a primary role of the liver in metabolism and detoxification?
How does the liver contribute to fat metabolism?
How does the liver contribute to fat metabolism?
The liver assists with protein metabolism. What is produced as a result of deamination of amino acids?
The liver assists with protein metabolism. What is produced as a result of deamination of amino acids?
How are bile salts involved in the digestion of fats?
How are bile salts involved in the digestion of fats?
What is the correct order of events for fat digestion and absorption?
What is the correct order of events for fat digestion and absorption?
How do the functions of the large intestine differ from those of the small intestine in the digestive system?
How do the functions of the large intestine differ from those of the small intestine in the digestive system?
Which process is directly responsible for the breakdown polysaccharides and disaccharides into monosaccharides?
Which process is directly responsible for the breakdown polysaccharides and disaccharides into monosaccharides?
Where does the process of starch digestion begin, and which enzyme is responsible for initiating this process?
Where does the process of starch digestion begin, and which enzyme is responsible for initiating this process?
What is the role of intestinal bacteria in the large intestine?
What is the role of intestinal bacteria in the large intestine?
How is propulsion accomplished in the GI tract?
How is propulsion accomplished in the GI tract?
What causes the simple reflex of salivation?
What causes the simple reflex of salivation?
Which of these is a function of saliva?
Which of these is a function of saliva?
Food is in the stomach in a semi-solid form called what?
Food is in the stomach in a semi-solid form called what?
Choose the answer that is NOT considered part of gastric juice.
Choose the answer that is NOT considered part of gastric juice.
Where are the chemical and osmoreceptors located that trigger an impulse in the intestinal phase of gastric control?
Where are the chemical and osmoreceptors located that trigger an impulse in the intestinal phase of gastric control?
Vitamin B can be absorbed by the intestinal walls due to which secretion?
Vitamin B can be absorbed by the intestinal walls due to which secretion?
Saliva is composed of:
Saliva is composed of:
Which of the following does the digestion of dietary carbohydrates start with?
Which of the following does the digestion of dietary carbohydrates start with?
Which of the following refers to the location of Neurons?
Which of the following refers to the location of Neurons?
What happens when there is interference with water absorption?
What happens when there is interference with water absorption?
Which of the following is a hormone that is secreted from the wall of the stomach and intestine?
Which of the following is a hormone that is secreted from the wall of the stomach and intestine?
What is the estimated amount of saliva that is secreted on a daily basis?
What is the estimated amount of saliva that is secreted on a daily basis?
Where do you find kupffer cells?
Where do you find kupffer cells?
Which of the following is NOT a primary function of the digestive system?
Which of the following is NOT a primary function of the digestive system?
How do the sympathetic and parasympathetic nervous systems interact to influence the activity of the enteric nervous system (ENS)?
How do the sympathetic and parasympathetic nervous systems interact to influence the activity of the enteric nervous system (ENS)?
Which of the following is an example of propulsive movement in the gastrointestinal tract?
Which of the following is an example of propulsive movement in the gastrointestinal tract?
How does the composition of saliva change under parasympathetic stimulation compared to sympathetic stimulation?
How does the composition of saliva change under parasympathetic stimulation compared to sympathetic stimulation?
What is the primary function of the grinding action in the stomach?
What is the primary function of the grinding action in the stomach?
How does the alkaline mucus secreted by mucous cells in the stomach contribute to gastric function?
How does the alkaline mucus secreted by mucous cells in the stomach contribute to gastric function?
What is the significance of hydrochloric acid (HCl) in gastric juice?
What is the significance of hydrochloric acid (HCl) in gastric juice?
What is the role of gastrin in gastric secretion, and where is it secreted?
What is the role of gastrin in gastric secretion, and where is it secreted?
During the cephalic phase of gastric secretion, what type of stimuli initiates the process, and through which nerve is it transmitted?
During the cephalic phase of gastric secretion, what type of stimuli initiates the process, and through which nerve is it transmitted?
During the intestinal phase of gastric secretion, what conditions in the small intestine inhibit gastric secretion, and how is this inhibition achieved?
During the intestinal phase of gastric secretion, what conditions in the small intestine inhibit gastric secretion, and how is this inhibition achieved?
What structural modifications in the small intestine contribute to its large absorptive surface area?
What structural modifications in the small intestine contribute to its large absorptive surface area?
What is the role of pancreatic juice in the small intestine, and how does it aid in digestion?
What is the role of pancreatic juice in the small intestine, and how does it aid in digestion?
What is the function of secretin in the context of pancreatic secretion?
What is the function of secretin in the context of pancreatic secretion?
How does the liver contribute to carbohydrate, fat, and protein metabolism?
How does the liver contribute to carbohydrate, fat, and protein metabolism?
Which of the following describes the role of bile salts in the digestion and absorption of lipids?
Which of the following describes the role of bile salts in the digestion and absorption of lipids?
What is the role of the exocrine pancreas in digestion, and what key components are involved?
What is the role of the exocrine pancreas in digestion, and what key components are involved?
In protein metabolism, what is the significance of deamination in the liver?
In protein metabolism, what is the significance of deamination in the liver?
In the context of lipid digestion, what is the role of pancreatic lipase?
In the context of lipid digestion, what is the role of pancreatic lipase?
Following lipid digestion, what is the primary function of chylomicrons?
Following lipid digestion, what is the primary function of chylomicrons?
What are the main functions of the large intestine related to water and electrolyte balance?
What are the main functions of the large intestine related to water and electrolyte balance?
What are the main dietary carbohydrates and how they are digested?
What are the main dietary carbohydrates and how they are digested?
What is the composition of saliva, and how do these components contribute to its overall function?
What is the composition of saliva, and how do these components contribute to its overall function?
How does the enteric nervous system (ENS) influence gastrointestinal function, and where are its neurons located?
How does the enteric nervous system (ENS) influence gastrointestinal function, and where are its neurons located?
How is the simple reflex of salivation stimulated?
How is the simple reflex of salivation stimulated?
What is the primary role of segmentation in the small intestine?
What is the primary role of segmentation in the small intestine?
How does saliva facilitate speech?
How does saliva facilitate speech?
What are the two main types of motility in the gastrointestinal tract, and how do they differ in function?
What are the two main types of motility in the gastrointestinal tract, and how do they differ in function?
How does the composition of feces relate to the function of the large intestine, and what contributes to its characteristic color?
How does the composition of feces relate to the function of the large intestine, and what contributes to its characteristic color?
What is the main purpose of mixing movements (segmentation) in the small intestine?
What is the main purpose of mixing movements (segmentation) in the small intestine?
What is the role of Kupffer cells in the liver?
What is the role of Kupffer cells in the liver?
What can result from excessive secretion of gastric juices that damage the protective alkaline mucous?
What can result from excessive secretion of gastric juices that damage the protective alkaline mucous?
Where does the digestion of proteins starts?
Where does the digestion of proteins starts?
Which abnormality may occur as a result of obstruction in the Bile ducts?
Which abnormality may occur as a result of obstruction in the Bile ducts?
What is the main role of the liver in fat metabolism:?
What is the main role of the liver in fat metabolism:?
Flashcards
Gastrointestinal Tract
Gastrointestinal Tract
The gastrointestinal tract includes the mouth, oesophagus, stomach, small intestine, and large intestine.
Associated Digestive Organs
Associated Digestive Organs
Associated organs include the salivary glands, liver, and pancreas that supply secretions needed for digestion.
Digestion
Digestion
Digestion breaks down large molecules into small absorbable molecules.
Absorption
Absorption
Signup and view all the flashcards
Secretion
Secretion
Signup and view all the flashcards
Motility
Motility
Signup and view all the flashcards
Control of GIS
Control of GIS
Signup and view all the flashcards
Enteric Nervous System (ENS)
Enteric Nervous System (ENS)
Signup and view all the flashcards
Gastrointestinal Hormones
Gastrointestinal Hormones
Signup and view all the flashcards
Aim of Motility
Aim of Motility
Signup and view all the flashcards
Peristalsis
Peristalsis
Signup and view all the flashcards
Segmentation Movement
Segmentation Movement
Signup and view all the flashcards
Saliva Secretion
Saliva Secretion
Signup and view all the flashcards
Parotid Glands
Parotid Glands
Signup and view all the flashcards
Submandibular Glands
Submandibular Glands
Signup and view all the flashcards
Sublingual Glands
Sublingual Glands
Signup and view all the flashcards
Composition of Saliva
Composition of Saliva
Signup and view all the flashcards
Lubrication Function
Lubrication Function
Signup and view all the flashcards
Coating Function of Saliva
Coating Function of Saliva
Signup and view all the flashcards
Dissolving Function of Saliva
Dissolving Function of Saliva
Signup and view all the flashcards
Oral Hygiene Function of Saliva
Oral Hygiene Function of Saliva
Signup and view all the flashcards
Starch Digestion in Mouth
Starch Digestion in Mouth
Signup and view all the flashcards
Saliva and Speech
Saliva and Speech
Signup and view all the flashcards
Control of Salivary Secretion
Control of Salivary Secretion
Signup and view all the flashcards
Parasympathetic Saliva
Parasympathetic Saliva
Signup and view all the flashcards
Sympathetic Saliva
Sympathetic Saliva
Signup and view all the flashcards
Conditioned Reflex
Conditioned Reflex
Signup and view all the flashcards
Simple Reflex
Simple Reflex
Signup and view all the flashcards
Excessive Salivation
Excessive Salivation
Signup and view all the flashcards
Xerostomia
Xerostomia
Signup and view all the flashcards
Main Parts of Stomach
Main Parts of Stomach
Signup and view all the flashcards
Chyme Formation
Chyme Formation
Signup and view all the flashcards
Functions of the Stomach
Functions of the Stomach
Signup and view all the flashcards
Types of Stomach Cells
Types of Stomach Cells
Signup and view all the flashcards
Mucous Cells Function
Mucous Cells Function
Signup and view all the flashcards
Parietal Cells Function
Parietal Cells Function
Signup and view all the flashcards
Chief Cells Function
Chief Cells Function
Signup and view all the flashcards
G Cells
G Cells
Signup and view all the flashcards
Gastric Juice Composition
Gastric Juice Composition
Signup and view all the flashcards
Role of Acid
Role of Acid
Signup and view all the flashcards
Pepsinogen
Pepsinogen
Signup and view all the flashcards
Intrinsic Factor
Intrinsic Factor
Signup and view all the flashcards
Phases of Gastric Secretion
Phases of Gastric Secretion
Signup and view all the flashcards
Cephalic Phase
Cephalic Phase
Signup and view all the flashcards
Gastric Phase
Gastric Phase
Signup and view all the flashcards
Intestinal Phase
Intestinal Phase
Signup and view all the flashcards
Peptic Ulcer Cause
Peptic Ulcer Cause
Signup and view all the flashcards
Small Intestine Segments
Small Intestine Segments
Signup and view all the flashcards
Digestion in Sm Intestine
Digestion in Sm Intestine
Signup and view all the flashcards
Small Intestine Modifications
Small Intestine Modifications
Signup and view all the flashcards
Absorption in the Small Intestine
Absorption in the Small Intestine
Signup and view all the flashcards
Study Notes
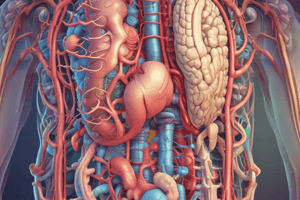
Overview of the Digestive System
- The digestive system's primary function is to break down large molecules into smaller, absorbable ones through digestion
- Absorption is the passage of digested food into the blood by crossing the mucosa of the gastrointestinal tract (GIT)
- Secretion involves the release of saliva and other GIT juices
- Motility aids in transporting food from the mouth to all parts of the alimentary canal
Control Mechanisms
- Motility and secretion in the gastrointestinal system (GIS) are controlled by the autonomic nervous system (ANS) and gastrointestinal hormones
- The Enteric Nervous System (ENS) is a special part of the ANS within the GIT
- Neurons are located within the wall of the intestine
- Sympathetic and parasympathetic systems can modify the activity
Gastrointestinal Hormones
- The stomach and intestine walls secrete hormones to control activity
- Examples are Gastrin, Cholecystokinin, Secretin, and Gastric Inhibitory Peptide (GIP)
Motility in the Stomach and Intestine
- Motility aims to mix food with digestive enzymes and push it down the gastrointestinal tract (GIT)
- Two types of motility are propulsive movement (peristalsis) and mixing movement (segmentation)
- Peristalsis carries food down the GIT and is stimulated by distension
- During peristalsis, the intestine part behind the food contracts, while the part in front dilates
- Segmentation mixes food with digestive enzymes
Saliva Production and Composition
- Saliva mixes with food in the mouth
- Approximately 1.5 liters of saliva are secreted daily
- Saliva is produced mainly by three pairs of glands in the oral cavity:
- Parotid glands produce a serous, watery secretion (25%)
- Submandibular glands produce a mixed serous and mucous secretion (70%)
- Sublingual glands secrete mainly mucous secretion (5%)
- Saliva consists of water, electrolytes, enzymes (amylase), and mucin
- It is rich in bicarbonate, calcium, and phosphate
- Alkaline pH, calcium, and phosphate help protect teeth from demineralization
Functions of Saliva
- Lubrication and binding: Mucus binds masticated food into a slippery bolus, aiding swallowing.
- Coating the oral cavity and esophagus: Protects against solid food particles.
- Dissolving dry food: Stimulates taste receptors.
- Oral hygiene: Mechanical flushing, lysozyme (lyses bacteria), and antibodies (IgA) are present.
- Initiates starch digestion: contains enzyme amylase, which starts digestion of dietary starch into maltose
- Speech assistance: facilitates movement of the lips, tongue, and teeth
Control of Salivary Secretion
- The autonomic nervous system controls salivary secretion
- Parasympathetic stimulation produces a large saliva volume, rich in electrolytes
- Sympathetic stimulation produces a small, thick secretion rich in enzymes
- Salivary secretion has two phases: conditioned (acquired) reflex and simple (inborn) reflex
- Conditioned reflex starts before food enters the mouth, triggered by sight, smell, or thought of food
- Specific visual, auditory, olfactory, or memory stimuli, interpreted in the cerebrum, initiate saliva production via the medulla and autonomic nerves
- A simple (inborn) reflex is stimulated by food or any object's presence in the mouth through sensory impulses sent to the medulla, leading to saliva production
Abnormalities in Salivary Secretion
- Excessive salivation is a symptom of lesions in the oral cavity
- Xerostomia is decreased salivary secretion that may lead to oral infections
The Stomach
- The main parts are fundus, body, antrum, and pylorus
- Food enters the stomach as a semi-solid bolus and is turned into a semi-liquid form by the grinding action of the stomach and gastric juice
- Liquidified food passes through the pyloric canal into the small intestine
Functions of the Stomach
- Serves as a short-term storage reservoir
- It grinds and mixes food with gastric secretions, resulting in liquefaction
- Slowly releases food into the small intestine for further processing
- Starts digestion of some foods, particularly proteins
- Releases iron from its compounds
Stomach Cell Types
- The stomach wall contains four main types of cells:
- Mucous cells secrete alkaline mucus that protects the epithelium.
- Parietal cells secrete hydrochloric acid and intrinsic factor
- Chief cells secrete pepsin, a proteolytic enzyme
- G cells secrete the hormone gastrin
Gastric Secretion
- About 2.5 liters of gastric juice are secreted into the stomach daily
- Gastric juice consists of mucus (bicarbonate-rich to protect and lubricate), hydrochloric acid (for acidic medium and pepsinogen activation), pepsinogen (inactive protease activated into pepsin), and intrinsic factor (for vitamin B12 absorption)
- The stomach secretes hormones (like gastrin) into the blood, which controls acid secretion and gastric motility
Control of Gastric Secretion
- Gastric secretion is divided into three phases:
- Cephalic phase: triggered by seeing, smelling, or anticipating food and prepares the stomach for a meal ; employs parasympathetic stimuli via the vagus nerve
- Vagus nerve stimulation releases ACH, stimulating gastrin and histamine secretion, which then stimulates gastric juice secretion
- Gastric phase: occurs when a meal enters the stomach, causing distension and mucosal irritation, which stimulates further gastric juice secretion by increasing gastrin and histamine
- Intestinal (inhibitory) phase: the small intestine detects highly acidic or hyperosmolar contents and sends inhibitory impulses and hormones to the stomach to inhibit secretion
Abnormalities of Gastric Secretion
- Excessive secretion or damage to the protective alkaline mucous barrier may result in peptic ulcer
- Drugs like aspirin, alcohol, and bacteria (Helicobacter pylori) can damage the protective layer
- Drugs like cimetidine, ranitidine, and omeprazole can decrease acid secretion
- Cimetidine and ranitidine are histamine antagonists
The Small Intestine
- The small intestine, extending from the pylorus to the large intestine, is the longest section of the digestive tube
- It consists of the duodenum, jejunum, and ileum
- Digestion and absorption of almost all nutrients occur here
- It is essential for life
Digestion and Absorption in the Small Intestine
- Exposure to pancreatic enzymes and bile enables the digestion of all food particles
- The final stages of digestion occur on the surface of the small intestinal epithelium (the brush border)
- Intestine’s absorptive surface area (brush border) is about 250 square meters
- Mucosal folds, villi, and microvilli increase the surface area
Absorption in the Small Intestine
- It is the primary site for nutrient absorption, where all nutrients are absorbed into the blood across the mucosa
- Absorbs water and electrolytes
Absorption of Water and Electrolytes
- The small intestine absorbs great quantities of water
- A normal person ingests roughly 1 to 2 liters of dietary fluid every day
- The small intestine receives another 6 to 7 liters daily from secretions
- Approximately 80% of the fluid is absorbed by the time the content enters the large intestine
- Water absorption is dependent on the absorption of solutes, particularly sodium
- Interference with water absorption can cause diarrhea
The Pancreas
- The pancreas consists of two main parts:
- Exocrine pancreas that secretes pancreatic juice important for digestion
- Endocrine pancreas that secretes hormones (insulin and glucagon) for glucose metabolism
Pancreatic Juice
- About 1.5 liters of pancreatic juice are secreted daily into the duodenum by the pancreas exocrine
- Pancreatic secretion and bile enter the duodenum through a common opening
- Pancreatic juice is alkaline (rich in bicarbonate)
- Pancreatic juice contains amylase, trypsin, chymotrypsin, and lipase
Functions of Pancreatic Juice
- Neutralizes acids coming from the stomach to the duodenum via Sodium Bicarbonate
- Prevents development of duodenal ulcer
- Adjusts the PH for the action of pancreatic enzymes
- Responsible for Protein digestion (trypsin, chymotrypsin, carboxypeptidase enzymes)
- Responsible for Lipid digestion (pancreatic lipase)
- phospholipase A2 is also secreted
- Responsible for Carbohydrate digestion via pancreatic amylase
Control of Pancreatic Secretion
- Secretin, produced by the duodenum, stimulates HCO3 secretion
- Cholecystokinin(CCK), produced by the duodenum, stimulates enzyme secretion
- Parasympathetic (Vagus) stimulates enzyme secretion
Functions of the Liver
- Carbohydrate metabolism: glucose to glycogen and vice versa
- Fat metabolism: desaturation of fat
- Protein metabolism: deamination of amino acids
- Removing nitrogenous portion to form urea
- Transamination: Remove the nitrogenous portion to form carbohydrate molecules
- Synthesis of plasma proteins and most of the blood clotting factors
- Breakdown of erythrocytes and defense against microbes (Kupffer cells)
- Detoxification of drugs and noxious substances (ethanol)
- Inactivation of hormones (insulin and sex hormones)
- Synthesis of vitamin A from carotene
- Production of heat
- Responsible for Bile secretion and synthesis
- Storage: Fat-soluble vitamins, Iron and copper, and some water-soluble vitamins
Bile
- Bile is a yellow secretion formed in the liver
- It is collected by the bile ducts and secreted into the duodenum
- Bile is stored in the gall bladder between meals
Composition of Bile
- The bile consists of bile salts and bile pigments
- Bile salts emulsify fat
- Bile pigments (bilirubin) are waste products excreted in stools
Control of Bile Secretion
- Bile secretion is stimulated by the vagus nerve and the hormone cholecystokinin
- Secretion starts when a meal enters the duodenum
- Obstruction in the bile ducts causes jaundice due to increased bile pigments in the blood
Digestion and Absorption of Carbohydrates
- Polysaccharides and disaccharides must be digested to monosaccharides
- Starch, the main dietary carbohydrate, digestion starts in the mouth by the salivary amylase
- Pancreatic amylase continues the digestion of carbohydrates
- Amylase breaks down starch into maltose
- Enzymes on the wall of the small intestine (the brush border): lactose (milk sugar), sucrose (table sugar), and maltose
- Maltase cleaves maltose into two molecules of glucose
- Lactase cleaves lactose into a glucose and a galactose
- Sucrase cleaves sucrose into a glucose and fructose
- Monosacharides (glucose, galactose, and fructose) are absorbed into the intestinal cells and then into the blood
- Lactose intolerance (abdominal discomfort and diarrhea following intake of milk) is caused by the deficiency of lactase
Digestion and Absorption of Proteins
- Proteins must be digested to amino acids
- Protein digestion starts in the stomach
- The stomach secretes pepsinogen (activated to pepsin by the action of HCl)
- The pancreas secretes trypsin and chymotrypsin
- Proteases are secreted as inactive and activated after reaching the lumen of the intestine
- Gastric and pancreatic proteases digest proteins within the lumen of the small intestine into peptides
- The intestinal surface peptidase enzymes
- The peptidases complete the breakdown of peptides, converting them to free amino acids
- amino acids are absorbed into the blood
Digestion and Absorption of Lipids
- Triglyceride is a dietary lipid with glycerol and 3 fatty acids
- The foodstuffs contain cholesterol, fat-soluble vitamins
- The two processes that must occur for the triglyceride to be absorbed: emulsification and digestion
- Emulsification is dietary triglyceride , that broken down due to aqueos enviornment
- Triglyceride molecules undergo enzymatical breakdown to produce monoglyceride and fatty acids
- Emulsification is done by bile salts
- Bile salts have water and fat-soluble poles
- Dietary lipids are micelles
- Digestion involved pancreatic
Absorption of Lipids
- Digestion of triglycerides into monoglycerides and fatty acids occurs
- Monoglycerides, fatty acids form structures with bile salts and other lipids called micelles
Chylomicrons
After entry into the intestinal cells, lipids combine with proteins to form structures inside cells
- Chylomicrons enter the lymphatics before, and chort chain fatt acids may enter the bloodstream directly
Functions of the Large Intestine, Rectum, and Anal Canal
-
Involves water absorption until semisolid feces are produced
-
Mineral salts, vitamins, and some drugs are absorbed Involves microbial activity- certain types of bacteria are synthesized by bacterial and synthesized form vitamin K and folic acid
-
Gases produced by bacterial fermentation pass out as flatus
Mass Movement and Defecation
- Strong peristalsis sweeps along the transverse colon
- external anal sphincter is under conscious control through the pudendal nerve
- Defecation involves themuscle contraction of the rectum
- Abdominal mmuscles and lowering of the diaphragm assist the process of defecation
Feces
-
Normal feces consist roughly of 75% water and 25% solids
-
Buld is fecal solids are made up of bacteria and undigested organic matter/fibers
-
Brown cholor is due to stercobilinogen by bacterial degradation
-
Odor is due to gases proudced by bacterial metabolism
Intestinal Gas
- Is present in the gastrintestinal tract
- Common complaints of excessive gas by people is common
- Five major intestinal gases are nitrogen, oxygen, carbon dioxide, hydrogen, and methane
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.