Podcast
Questions and Answers
What is the primary function of flat bones in the human body?
What is the primary function of flat bones in the human body?
- To store minerals and nutrients
- To provide support and structure to the body
- To facilitate movement and flexibility
- To protect internal organs and provide muscle attachment (correct)
During which week of gestation do limb buds begin to develop?
During which week of gestation do limb buds begin to develop?
- 8th week of gestation
- 6th week of gestation
- 10th week of gestation
- 4th week of gestation (correct)
What is the term for the process of converting a cartilage template into a long bone?
What is the term for the process of converting a cartilage template into a long bone?
- Intramembranous ossification
- Endochondral ossification (correct)
- Bone resorption
- Bone remodeling
Which of the following bones is an example of a sesamoid bone?
Which of the following bones is an example of a sesamoid bone?
What is the term for the bones that make up the central line of the body?
What is the term for the bones that make up the central line of the body?
Which of the following bones is an example of an irregular bone?
Which of the following bones is an example of an irregular bone?
What is the union between the axial and appendicular skeletons facilitated by?
What is the union between the axial and appendicular skeletons facilitated by?
What is the primary function of short bones in the human body?
What is the primary function of short bones in the human body?
What is the primary function of osteoclasts in bone remodeling?
What is the primary function of osteoclasts in bone remodeling?
What is the main characteristic of compact bone?
What is the main characteristic of compact bone?
What is the primary component of the inorganic substance of bone extracellular matrix?
What is the primary component of the inorganic substance of bone extracellular matrix?
What is the function of haversian systems (osteons) in bone structure?
What is the function of haversian systems (osteons) in bone structure?
What is the role of osteoblasts in bone formation?
What is the role of osteoblasts in bone formation?
What is the main difference between compact bone and cancellous bone?
What is the main difference between compact bone and cancellous bone?
What is the function of glycoproteins and proteoglycans in bone extracellular matrix?
What is the function of glycoproteins and proteoglycans in bone extracellular matrix?
What is the primary function of osteocytes in bone structure?
What is the primary function of osteocytes in bone structure?
What is the primary function of osteoclasts in the bone remodelling process?
What is the primary function of osteoclasts in the bone remodelling process?
During the inflammatory phase of fracture repair, what type of cells rush to the injury site?
During the inflammatory phase of fracture repair, what type of cells rush to the injury site?
What is the primary function of osteoblasts in the bone remodelling process?
What is the primary function of osteoblasts in the bone remodelling process?
During the hard/bony callus formation stage of fracture repair, what type of bone is formed?
During the hard/bony callus formation stage of fracture repair, what type of bone is formed?
What is the term for the process of removing old bone tissue and forming new bone tissue?
What is the term for the process of removing old bone tissue and forming new bone tissue?
During which stage of fracture repair is a soft callus composed of cartilage and collagen formed?
During which stage of fracture repair is a soft callus composed of cartilage and collagen formed?
What is the number of ossification centers in the cartilage model?
What is the number of ossification centers in the cartilage model?
At what stage of development is the primary ossification center formed?
At what stage of development is the primary ossification center formed?
What is the function of epiphyseal growth plates?
What is the function of epiphyseal growth plates?
What is the term for the production of flat bone from stem cells without a cartilage template?
What is the term for the production of flat bone from stem cells without a cartilage template?
What is the region of bone where the diaphysis meets the epiphysis?
What is the region of bone where the diaphysis meets the epiphysis?
What is the function of osteoblasts?
What is the function of osteoblasts?
At what stage of development do the epiphyseal growth plates fuse?
At what stage of development do the epiphyseal growth plates fuse?
What is the term for the process of bone development resulting from the replacement of cartilage with bone tissue?
What is the term for the process of bone development resulting from the replacement of cartilage with bone tissue?
Flashcards are hidden until you start studying
Study Notes
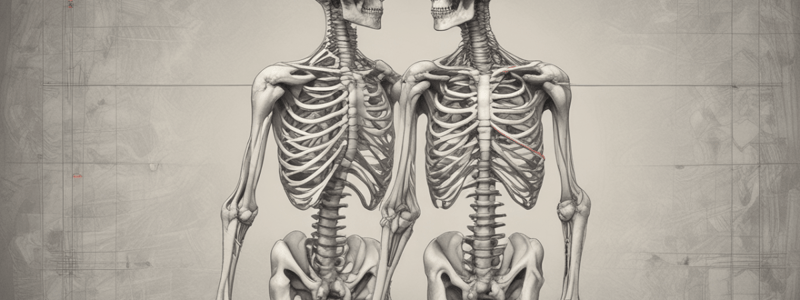
Bone Structure
- The skeleton consists of two large parts: Axial and Appendicular.
- Axial part: composed of bones of the skull, vertebral column, ribs, and sternum, forming the central line of the body.
- Appendicular part: consists of the axial part and bones of the limbs.
Axial and Appendicular Skeleton
- The union between axial and appendicular skeletons is formed by the pectoral girdle and pelvic girdle.
Types of Bones
- Long bones: examples include femur and humerus.
- Flat bones: generally used for protection or muscle attachment (e.g. sternum or parietal).
- Short bones: small bones found in some joints (e.g. carpal bones in the wrist and tarsal bones in the ankles).
- Sesamoid bones: bones embedded within tendons or muscle, used to transfer force (e.g. patella).
- Irregular bones: bones that do not occupy any of the other categories (e.g. vertebrae).
Limb Development
- Limb development begins during the 4th week of gestation, with limb buds appearing from the lateral plate mesoderm.
Bone Development
- Endochondral ossification: the process of converting a cartilage template into a long bone.
- Intra-membranous ossification: the production of flat bone from stem cells without a cartilage template.
Endochondral Ossification Process
- 5 weeks: complete cartilage template for long bones.
- 8 weeks: collar of bone starts forming around the middle of the bone.
- 12 weeks: primary ossification centre develops, causing bone development.
- At birth: secondary ossification centres form at the ends of the bone.
- During childhood: epiphyseal growth plates develop, and secondary ossification centres develop into bone.
- Adulthood: full bone length is achieved, epiphyseal growth plates fuse, and the ends of the bones remain capped with cartilage.
Descriptive Regions of Bones
- Epiphysis: ends of long bones, develop from secondary ossification centres.
- Epiphyseal plate: growth site in length, contains cartilage in actively growing bones.
- Metaphysis: junction where the diaphysis meets the epiphysis.
- Diaphysis: shaft of a long bone, represents the primary ossification centre.
Bone Cells
- Osteoblasts: cells responsible for bone formation, secrete collagen and other components for building mineralized bone matrix.
- Osteocytes: mature bone cells from osteoblasts, regulate osteoblasts and osteoclasts in response to mechanical signals.
- Osteoclasts: large cells responsible for bone resorption, essential for bone remodeling, repairing microdamage, and regulating calcium levels.
Osseous Tissues
- Compact bone: bony lamellae are strongly packed together with no space in between, more dense and rigid.
- Cancellous/Spongy/Trabecular bone: irregular bone trabeculae are loosely distributed, leaving space for bone marrow.
Haversian Systems (Osteons)
- Rings around a central canal with blood vessels and nerves for osteocytes, strengthen bones, enhance resistance and durability.
Bone Extracellular Matrix
- Organic substance: collagen provides flexibility and strength to bone, glycoproteins and proteoglycans aid in organization and stress resistance.
- Inorganic substance: primarily hydroxyapatite crystals, a calcium phosphate compound, gives bone hardness and resistance to compression.
Bone Remodelling
- Process that involves the removal of old bone tissue (resorption) and the formation of new bone tissue.
Stages of Fracture Repair
- Inflammatory phase (hematoma): blood clotting and inflammatory response begins, specialized cells rush to the injury site.
- Soft/fibrocartilaginous callus formation: fibroblasts and chondrocytes create a soft callus composed of cartilage and collagen, stabilizing the fracture site.
- Hard/bony callus formation: osteoblasts produce new bone tissue, replacing the cartilaginous callus, forming a hard bony callus made of woven bone.
- Remodeling phase: the final stage of fracture repair, where the bone is fully restored to its original shape and function.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.